Early Signs of Cognitive Decline You Shouldn’t Ignore
Early Signs of Cognitive Decline You Shouldn’t Ignore
The term “cognitive decline” encompasses a wide spectrum of neurological statuses. On one end of the spectrum, we find mild cognitive impairment (MCI), a condition that can become more commonplace as we age. Individuals living with this early stage of memory or cognitive ability loss may experience an increased risk of developing a more severe condition. These conditions, including many forms of dementia, lie on the other end of the spectrum. But what are the signs of cognitive decline, and when should you become concerned?
Signs of Mild Cognitive Impairment (MCI)
Symptoms of MCI often include:
- Increased forgetfulness. You may take longer to recall someone’s name, miss an important date such as a close friend’s birthday, or blank on a scheduled appointment.
- Interrupted train of thought. This often occurs during conversations or when engaging with entertainment (movies, television, books). You may find yourself rereading the same paragraph two, three, or more times.
- Decision-making stress. Becoming overwhelmed at the thought of making a decision, whether major or insignificant in nature, can be an indication of MCI.
- Confusion in the day-to-day. Many people with MCI start to feel uncertain about “next steps” or understanding instructions.
- Trouble navigating familiar environments. Getting lost on a familiar or frequently traveled route might indicate MCI is present.
- Impulsivity. Acting without thinking things through or expressing poor judgment in certain situations may also be a sign of MCI
- Mental health challenges. Individuals with MCI may present with depression, anxiety, apathy, irritability, or aggression.
Mild cognitive impairment isn’t uncommon and isn’t necessarily a sign of worsening capabilities to come. In fact, some medications and health conditions can cause these same symptoms on a temporary basis.
Most of us notice a gradual slowdown in our mental processes over the years, just as we do in our physical abilities. Although these changes in mental acuity aren’t inevitable, they also shouldn’t be cause for significant alarm — unless they begin to impair our ability to function on a day-to-day basis.
What Is Subjective Cognitive Decline?
A person’s family members or friends might be the first to pick up on symptoms of cognitive decline, but in many cases, individuals themselves recognize something isn’t quite right with their cognitive capacity. The Centers for Disease Control and Prevention (CDC) defines subjective cognitive decline as self-reported confusion or memory issues that have been occurring more frequently or getting worse over the span of a year.
The CDC also notes:
- Overall, the prevalence of subjective cognitive decline (SCD) is 11.1% among Americans (1 in 9 individuals).
- Prevalence is lower among individuals with more years of formal education.
- Nearly 30% of adults with SCD live alone.
- More than two-thirds (66.2%) of adults with SCD have two or more chronic diseases.
- 6% of adults with SCD experienced functional difficulties while performing day-to-day activities or chores.
Given this data, the CDC states SCD is a “growing public health issue.”
When Cognitive Decline Becomes More Severe

While MCI may stabilize or even improve with intervention, symptoms of MCI could also be the beginning of more severe cognitive decline. Many signs of worsening cognitive decline mimic those of MCI, just at more intense levels.
- Confusion becomes much more pronounced. Some people begin to lose track of time or are unsure what day/date it is.
- Making decisions becomes even more difficult, which can lead to frustration and anger towards others.
- Memory loss deepens, with many more instances of forgetting names, dates, places, and events.
- Individuals may be found wandering for unknown reasons, or placing items in odd locations (e.g. car keys in the freezer).
- People tend to have trouble conversing, possibly due to diminished concentration and train of thought.
These factors may contribute to increased social withdrawal. Many people with cognitive decline or dementia understand they’re developing characteristics they may be embarrassed about, or that others find undesirable, and withdraw from friends and family as a result. In other instances, depression or anxiety may prevent them from interacting with others like they used to.
Have you noticed changes in your memory, attention or thinking skills?
Download our free e-book, “What’s Happening to My Brain?” to learn how you can improve your brain health and cognitive vitality at any age.
Unfortunately, social isolation leads to an entirely new set of concerns. Isolated individuals are more at risk for poor health outcomes, self-neglect, and fall-related injuries.
Surprising or Unusual Signs of Cognitive Decline
When thinking about cognitive decline and dementia, people are often aware of the above symptoms (memory, confusion, etc.). But some lesser-known signs of cognitive decline include:
- Changes in sense of smell. A study published in the journal Neurology found that people who could no longer distinguish between two very different odors (e.g. lemons and gasoline) may be in the early stages of Alzheimer’s disease.
- Trouble with the law. Dementia sometimes impacts the areas of the brain that control judgment, self-control, violence, and sexual behavior. Individuals with cognitive decline may find themselves in criminal situations, such as theft, trespassing, or even assault.
- Altered sleep patterns. Many people with dementia develop sleep issues such as insomnia, hypersomnia (sleeping too much), or sleeping during the day. This may be due to changes in the body’s circadian rhythm.
- Changes in walking. Slower walking or changes in stride length/gait might indicate dementia-related shifts in the brain.
Take Charge of Your Brain Health With The Aviv Medical Program

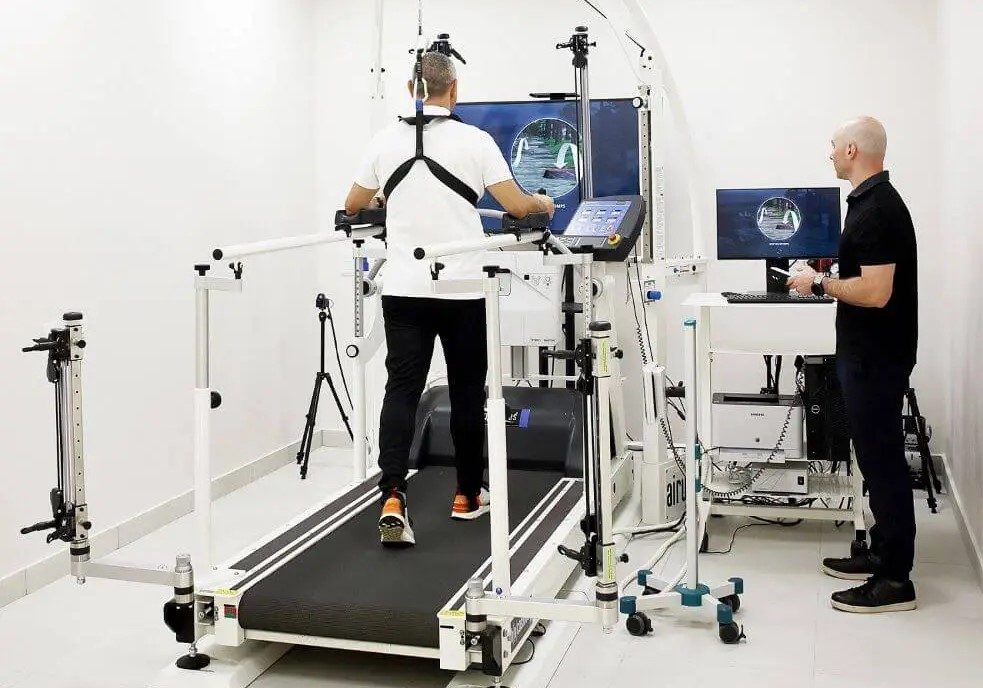
Noticing early signs of cognitive decline can be unsettling, whether it’s forgetfulness, slower processing, or difficulty multitasking. At Aviv Clinics, we help clients take proactive control of their brain health with a program built on nearly two decades of peer-reviewed, published scientific research.
For people concerned about declining cognitive abilities, the Aviv Medical Program can include advanced cognitive testing to identify subtle impairments and track meaningful improvements over time. Using evidence-based interventions like hyperbaric oxygen therapy and cognitive training exercises, our program targets the main cognitive domains most often affected by aging, including:
- Memory
- Attention
- Speed of information processing
- Multitasking
- Executive skills
Our board-certified physicians prescribe a personalized treatment program for each client to target their specific concerns and definicencies.
If you or someone you love is experiencing changes in memory or thinking, don’t wait for symptoms to worsen. Contact us to get clarity and start mapping your path forward with Aviv Clinics.
Last Update: July 17, 2025.
Benefits of Intermittent Fasting for Visceral Fat, Longevity, and Metabolic Health
Intermittent fasting has become a popular dietary buzzword over the last decade, but it’s far from being a new concept. In prehistoric times, fasting was just a part of daily life. As hunters and gatherers, our ancestors often went long stretches without food between successful hunts. We’ve come a long way since then to discover the true scientific benefits of intermittent fasting.
The documented benefits of intermittent fasting as a dietary method also stretch back centuries. In the 1500s, nobleman Luigi Cornaro, made significant changes to his diet and lifestyle habits in his 40s to strengthen his “weak constitution.” He eventually lived to be 103 years old, a shock to his colleagues. Twenty years before his death, he chronicled his dietary changes for posterity.
Today, intermittent fasting is supported by extensive clinical research. In 2019, the New England Journal of Medicine published a landmark peer-reviewed paper on its health benefits. For many, intermittent fasting is more than a tool for weight loss. It’s also a viable approach to living longer, healthier lives.

What is Intermittent Fasting and Why Does It Work?
The human body operates with one goal in mind: survival. If you go 8-12 hours without food, your entire body is out of its primary energy source. You have no more stored glycogen, which provides energy. Your liver and muscle cells are empty, and your brain is screaming for sustenance. As a result, your body begins burning fat for energy instead. Specifically, it targets visceral fat, or the fat that surrounds our organs.
It’s important to note that not all fat stored in the body is “bad.” Humans need certain types of fat to promote healthy metabolism and optimal hormone levels.
However, visceral fat doesn’t hold those positive connotations. High visceral fat levels are linked to conditions like:
- Diabetes
- Heart disease
- Stroke
- Arterial disease
- Certain types of cancers
By prompting the body to burn visceral fat, intermittent fasting may help reduce the risk of these conditions while also supporting metabolic health.
Scientific Benefits: Longevity, Inflammation Reduction and More
The research on intermittent fasting reveals its impact beyond weight loss. Additional benefits include improvements to:
- Thinking and memory
- Blood pressure
- Physical performance
- Type 2 diabetes
- Sleep apnea
Intermittent fasting may also have protective effects against certain cancers and promote longevity. One study reveals that 13 hours without ingesting calories reduces breast cancer recurrence. In laboratory rodents, intermittent fasting improved longevity by 15-20 percent.
Inflammation reduction is another benefit. Chronic inflammation plays a role in the development many serious conditions, such as:
- Alzheimer’s disease
- Arthritis
- Asthma
- Multiple sclerosis
- Stroke

The Easiest Diet? Real-life Benefits of Time-Restricted Eating
Aside from the health benefits, one of the best aspects of intermittent fasting is that it doesn’t require people to invest any extra time or money. It doesn’t require special foods, hours measuring and weighing your meals, or calorie counting. There are also no “off-limit” foods. You can still enjoy your favorite meals and snacks as long as you do so in moderation.
In truth, all intermittent fasting really takes is time. You already fast every night while sleeping, right?
A popular intermittent fasting schedule is 16:8, or fasting for 16 hours and feasting for eight. Your goal should be to fast for at least 13 hours a day, which is where the measurable health benefits take hold. However, there’s no detriment to switching up your schedule. Some days you may hit 13 hours, other days, you might aim for 16 or 18.
Consistently practicing intermittent fasting is more important than perception. You might fast for 16 hours on weekdays, then relax your schedule on weekends. This flexibility makes intermittent fasting easier to stick with long term.
That said, there is some risk in fasting for too long. For example, if you’re regularly hitting the 20-hour mark, you’ll likely start to lose muscle mass. The body can only absorb 30 grams of protein at a time. With a limited feast window, you may not be getting adequate protein intake.
Popular Fasting Schedules: 16:8, 5:2 and Alternate Day Plans
There are multiple different approaches to intermittent fasting. Some of the most common include:
- Time-Restricted Fasting. This approach works by limiting the daily window of feasting. For example, if you eat your first meal of the day at 10 a.m. and your last meal at 6 p.m., you’ve followed the 16:8 plan. Common ratios for time-restricted fasting include 14:10, 16:8, and 18:6.
- 5:2 fasting. In this strategy, individuals eat “normally” five days a week and fast for two days. On the fasting days, they restrict their calorie intake to one 500-calorie meal for women and one 600-calorie meal for men.
- Alternate Day Fasting. Using the same calorie intake as 5:2, fasting takes place every other day.
Time-restricted fasting is usually the best place to start, because you can ease into it by gradually shrinking your feast window. As you get more accustomed to fasting, you might venture into other methods to see if they work for you.
Intermittent Fasting Side Effects and Safety Considerations
Intermittent fasting is generally safe, but it isn’t for everyone. You should consult your doctor before changing your diet plan, especially if you live with one of these conditions:
- Diabetes. Diabetics should consult with their endocrinologist or diabetes educator before starting intermittent fasting. However, for people with insulin resistance, intermittent fasting may prevent diabetes from developing.
- Digestive issues. Some people experience constipation, which can occur especially if they don’t drink adequate amounts of water or eat enough high-fiber foods.
Of course, in the initial stages, one might experience some fatigue, hunger pangs, and possibly headaches. As with any lifestyle change, it takes persistence and time to adapt. Still, it’s critical to have a conversation with your healthcare provider if you’re curious about intermittent fasting’s effects.
Explore Nutrition Coaching and Health Support at Aviv Clinics
Intermittent fasting is a well-researched, low-effort approach to supporting physical health, cognitive performance, and longevity. Whether you’re aiming to lose weight, sharpen your mind, or reduce your risk of chronic disease, it’s a powerful tool—and it costs nothing to start.
At Aviv Clinics, nutrition coaching is one component of the personalized Aviv Medical Program. Our program incorporates physician-prescribed interventions, including a unique, evidence-based hyperbaric oxygen therapy protocol, to help you reach your health goals.
If you’re interested in exploring how Aviv Clinics can support your healthy living goals, we’re here to help.
Last Update: July 15, 2025.
HBOT for Athletes: Boosting Performance, Speeding Recovery, and Preventing Injury
Athletes are always looking for their next win, whether they are at the professional level or a weekend warrior. But, in doing so, they also encounter several challenges. Fatigue and injuries can seriously damage one’s competitive edge. In some cases, an injury or recurring injury forces athletes to abandon their sport entirely.
In recent years, hyperbaric oxygen therapy (HBOT) has emerged as an effective way to address injuries, aid in recovery, and improve athletic performance, both mentally and physically. Even if you’re an amateur athlete who is just passionate about your sport of choice, HBOT is a viable way to take your performance to the next level.
How Can Hyperbaric Oxygen Therapy Help Athletes?
Hyperbaric oxygen therapy can help athletes by:
- Enhancing physical performance and endurance
- Improving mental clarity and cognitive function
- Supporting better sleep and recovery
- Increasing energy and stamina
- Speeding up healing from injuries
- Reducing inflammation and preventing re-injury
As one of the largest and most advanced hyperbaric treatment centers in the world, Aviv Clinics has enhanced performance in athletes ranging from amateurs to elite professionals. Continue reading to learn more about the hyperbaric oxygen therapy benefits for athletes and how you can get started.
4 Ways Hyperbaric Oxygen Therapy Enhances Athletic Performance
There are four main HBOT benefits for athletes.
1. HBOT Can Boost Strength, Endurance, and VO2 Max
Studies speak volumes about HBOT’s transformative impact on physical athletic performance:
- Higher strength and endurance
- Increase mitochondrial efficiency
- Enhance maximal oxygen consumption (VO2 max)
- Contributes to faster healing after an injury
- Expedites recovery from non-injury soreness
- Reduces the incidence of injury occurrence or reoccurrence
- Breaks up the cycle of inflammation that athletes often experience
Hyperbaric chamber benefits don’t stop there.
Watch NFL neurosurgeon Dr. Joseph Maroon explain why he not only recommends the hyperbaric oxygen protocols of the Aviv Medical Program to patients with concussive injury to the brain, but also how his own participation in the program has improved his athletic performance and recovery times.
2. HBOT Can Increase Mental Clarity and Reaction Speed
Cognitive performance, which is a foundational focus of the Aviv Medical Program, plays a crucial role in athleticism. Intensity, focus, and attention support the physical fundamentals of a sport.
Research illustrates that patients who have undergone HBOT experience improvement in areas such as attention, focus, and information processing speed—all of which contribute to better athletic performance.
Two athletes who previously completed HBOT have spoken openly about its benefits.
Peter Paltchik is a Judo champion who was not just looking to maximize his physical capacity, but also his cognitive fortitude. Paltchik describes the program as his “ace card” to success:
“To be an Olympic medalist, every second counts. You must be able to analyze, to react, to think very quickly. This is the difference between winning and losing. In order to be the most complete athlete and the best fighter I can, I must have the best cognitive capabilities such as handling extreme levels of stress, concentration, making decisions in real time. After I joined the program, I felt the improvements in my mind and body. I was sharper, more focused in fights, and I was able to make quicker decisions.”
Alon Day, a four-time European NASCAR champion, also benefited from the program. Unlike other sports, race car driving is about intense, small motor movements. Drivers require significant grip strength to control the steering wheel at high speeds. Small movements of the hand and foot can make the difference between finishing first or crashing. The environment also takes a physical toll, as drivers wear a fireproof suit with no air conditioning, which can lead to dehydration.
Racing requires intense cognitive focus for an extended period. This is one area where Day made significant strides. After completing the Aviv Medical Program, Alon achieved approximately 15% improvement in cognitive function.
“There is nothing like it in the world. You cannot go to the gym and get the same results. When I came over there every morning, I felt like I was a bionic man, being in the hyperbaric chamber at the cutting edge of medicine. At the end of the hyperbaric treatment, when the season started, I was at my best. I won the championship, and I broke every record. In my opinion, this treatment is for whoever needs to be on top of their game.”
3. HBOT Enhances Sleep Quality and Recovery
Sleep is imperative to restoring the body after a hard workout. But sometimes, depending on injuries, daily stressors, and the pressure athletes face, getting consistent, quality sleep is easier said than done.
The good news is that research indicates the cognitive and physical improvements that come with HBOT help improve sleep quality. This has also been the case for those who have suffered from long COVID and experienced chronic insomnia.
4. HBOT Elevates Energy and Stamina Levels
HBOT encourages the body to heighten its aerobic stamina, including lung capacity and cardiovascular endurance. The exciting part about the therapy is that it focuses on helping individuals of all ages.
Watch PGA Tour golfer and Ryder Cup winner Tommy Fleetwood as he describes his experience with the Aviv Medical Program:
When 14-year-old Linden Perry suffered from post-concussion syndrome due to a sports injury, she regained her health and performance through a holistic treatment program—one that entailed HBOT, cognitive, and physical training. The personalized treatment plan left Perry more energized and gave her the confidence to continue to excel in her athletic programs.
Choosing the Right Type of HBOT for Athletes
While all hyperbaric chambers have the same goal, to deliver 100% oxygen in a high-pressure environment, not all chambers are created equally. There are different types of chambers that each possess a unique process.
Monoplace Chambers: Pros and Limitations
- Monoplace chambers administer oxygen to one person at a time. The chamber’s structure reflects a tube or cylinder in which individuals lie in a horizontal position while the chamber is typically compressed with 100% oxygen.
- Soft-side monoplace chambers are more “portable” than the rigid cylindrical HBOT chambers made of glass or plastic. These chambers, however, cannot reach the level of pressurization to produce high-level results.
But neither of these chambers is manufactured with the intent of offering oxygen fluctuation, which peer-reviewed published studies reveal is a key technique to optimizing results from HBOT.
Multiplace Chambers: Optimal for Athletes
Multiplace chambers or “suites,” such as the one at Aviv Clinics in The Villages, Florida, can utilize the science behind oxygen fluctuations in a pressurized environment. This mechanism produces the underlying elements of enhanced athletic performance. Research indicates that this specialized protocol, known in the scientific community as the hyperoxic-hypoxic paradox, can produce:
- Stem cell proliferation and differentiation. Stem cells can exist as any cell type in the human body. As it relates to physical performance, stem cell production supports the heart, lungs, and muscles. Lungs breathe deeper and more efficiently, allowing athletes to perform at a higher level for longer periods without becoming winded. The heart is able to pump out more oxygenated blood to other organs and muscles, and muscle growth occurs at a faster pace.
- Hypoxia-inducible factor (HIF). HIF plays a role in angiogenesis, or the creation of new blood vessels. With more routes for blood to travel throughout the body — to the heart, lungs, and muscle tissue — more oxygen is also getting to those areas. This prevents fatigue and muscle soreness. HIF is also instrumental in creating new red blood cells, ensuring that maximum oxygen flow goes to the organs.
- Vascular endothelial growth factor (VEGF). VEGF is a protein that gets released during HBOT treatments and “signals” blood vessel formation. Again, the more blood that can flow to key areas of the body, the higher one’s athletic capacity.
Maximizing HBOT for Athletes with a Holistic Program
For any athlete looking to reap the benefits of a hyperbaric chamber, it’s not just about the oxygen or even the oxygen fluctuations. Athletes need to incorporate additional components to reach their full potential.
Paltchik and Day both experienced brain-based enhancements thanks to the cognitive training element of the Aviv Medical Program. Nutritional coaching and physical training are other areas that can help athletes push their bodies to maximum output. That’s why the Aviv Medical Program can be personalized for each individual client.
A personalized program considers variables like an athlete’s unique biology, medical history, and performance goals to create a customized prescription for treatment.
How to Maximize Your Athletic Performance With HBOT
In short, to get the most out of HBOT as an athlete:
- Choose a clinic that uses fluctuating oxygen protocols (the hyperoxic-hypoxic paradox)
- Combine HBOT with cognitive and physical training
- Follow a personalized treatment plan tailored to your sport
- Incorporate nutrition coaching for energy and recovery
- Track your progress with performance metrics
The Bottom Line: Personalized HBOT for Athletic Performance
Whether you are a professional athlete or simply want to advance your athletic capabilities to their best potential, HBOT can help. To truly transform your game, the personalized approach of the Aviv Medical Program is second to none in achieving peak performance.
Athletes who go through the Aviv Medical Program may undergo HBOT along with physical, cognitive, and nutritional training. This holistic program is key to helping our patients enhance their health for the long run.
Contact us to learn more about how the Aviv Medical Program can help you achieve your goals.
Last Updated July 14, 2025
Mental Health Benefits of Golf: Boosting Mood, Reducing Anxiety and Building Connection
Since the COVID-19 pandemic, we’ve all become more aware of mental health challenges, the importance of addressing them, and the various ways they can be mitigated. Uncertainty, loss, and isolation have contributed to higher instances of depression and anxiety. Exercise and socializing are two ways to help maintain good mental health and reduce the risk of depression and anxiety.
The mental health benefits of golf offer a great way to easily combine exercise and socializing and support your mental health. Here are three primary reasons hitting the course is good for your brain.
How Golf Helps Depression and Anxiety
You may have heard of a ‘runner’s high.’ Many runners experience an exhilarating feeling during a great race or even during an everyday jog. However, running isn’t the only way to release endorphins, the brain’s “feel-good” neurotransmitters. Any form of exercise, including golf, can produce these mood-boosting chemicals.
For women, this can be particularly important. Many experts estimate that women are nearly twice as likely as men to be diagnosed with depression. The number could be even higher for those who suffer from depression, but do not have a formal diagnosis.
In an Australian study, researcher Kristiann Heesch looked at the effect of exercise on women’s depression. The results of her study showed that women who averaged 150 minutes of moderate exercise (golf, tennis, aerobics classes, swimming, or dancing) or 200 minutes of walking every week, had more energy, were more social, and felt better emotionally. These same women were not as limited by their depression, even three years after the study.
Endorphins also help ease anxiety, which is the most common mental health concern in the United States. According to data from the National Alliance on Mental Illness (NAMI), over 40 million adults in the U.S. (19.1%) have an anxiety disorder.
The exposure to sunshine when playing golf also has mental health benefits. Research has linked vitamin D deficiency with instances of depression and other mental health struggles. Even a cloudy day on the golf course provides the sun exposure required to optimize your vitamin D levels.

Golf as Stress Relief and Green Exercise
Most people encounter periods of stress in their lives. However, when stress becomes chronic, it can affect other components of health.
The National Institute on Mental Health (NIMH) reports that repeated stress can disrupt the functioning of the immune, digestive, cardiovascular, sleep, and reproductive systems. Even more cause for concern, the continued strain that stress places on your body may contribute to serious health problems, such as heart disease, high blood pressure, diabetes, and mental illness.
Chronic stress also negatively impacts the brain through memory problems, and weakened mental health. Stress can lead to neural atrophy, or actual shrinking of the brain.
The restorative impact of the endorphins from a round of golf, along with the meditative nature of the focus it requires may help reduce stress. Additionally, exercising outdoors, or “green exercise,” is actually better than indoor exercise when it comes to stress reduction.
Shedding your tensions during the course of playing nine or 18 holes can leave you feeling calmer, clearer, more focused, and ready to manage both daily and extraordinary challenges in your life.
Golf for Social Connection and Loneliness
Humans are naturally social beings. Although we’re not all social butterflies, interaction with others has been shown to improve overall health and well-being. This is one of the reasons so many individuals suffered with mental health concerns during the COVID pandemic: being forced to isolate themselves from friends and family for weeks or even months at a time. Loneliness is a factor in poor mental health outcomes.
Research has revealed that person-to-person interaction triggers the nervous system to release a combination of neurotransmitters that regulate the body’s response to stress and anxiety. Dopamine is another feel-good chemical produced by the brain, which has a compounding effect on one’s mental health.
“It’s part of our reward center, and when our brain produces dopamine in response to what we do, we feel good and want to do more of whatever it is that’s making us feel so mentally healthy. That, in turn, leads to even more dopamine production,” explains Tanya J. Peterson, NCC, DAIS, a mental health educator.
Playing golf with your friends, spouse, or colleagues can help reap these socialization benefits. Aviv Clinics clients already enjoy the camaraderie naturally fostered by their hyperbaric oxygen therapy sessions in our state-of-the-art HBOT suites. Golf games provide more opportunities for socializing and improving their overall experience.

Supporting Brain Health Beyond the Golf Course
The clinical team at Aviv Clinics understands that good mental health isn’t just about what happens in your mind. Our mental health is also shaped by what we do with our bodies. Whether it comes from golf or another source, physical activity, cognitive stimulation, social connection, and time outdoors all play a role in supporting a healthy, resilient brain.
That’s why Aviv’s personalized treatment plans can be custom-designed to support both brain and body performance. Our goal is to help clients feel more energized, focused, and emotionally well. Whether it’s getting back to your favorite activities like golf or feeling more present and connected with loved ones, our multidisciplinary team can help you achieve your cognitive and physical goals.
If you’re ready to take a proactive approach to your mental wellness and cognitive health, we invite you to learn more about how the Aviv Medical Program can help.
8 Questions to Ask Before Starting Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) is growing in popularity, as recent research has highlighted its ability to improve cognitive performance, physical recovery, and even potentially reverse aging biomarkers. But it’s important to understand that not all HBOT programs are created equal. From hospital wound care clinics to medi-spas promising to heal anything and everything, the types of HBOT available today vary widely in safety, science, and effectiveness. No matter where you’re considering treatment, there are important hyperbaric oxygen therapy questions you should ask first.
As more HBOT facilities open around the United States, it has become increasingly important to understand the differences and identify the option best able to meet your health goals and needs. As the largest and most advanced civilian HBOT facility in the nation, Aviv Clinics encourages you to educate yourself prior to treatment with hyperbaric medicine. Before you commit to a treatment plan, ask these seven questions to ensure the program aligns with your goals and delivers meaningful results.
1. What Type of Hyperbaric Oxygen Chamber Will I Be Using?
There are two main types of hyperbaric oxygen therapy chambers: monoplace and multiplace. Monoplace chambers treat one person at a time in an enclosed tube, while multiplace chambers are larger and accommodate multiple patients comfortably.
- Monoplace chambers are the most commonly used type of chamber and are frequently found in hospital burn units or wound care facilities. Patients typically recline in the tube while it is pressurized with 100% oxygen. Monoplace chambers are sometimes referred to as “Michael Jackson” tubes because the singer was once pictured inside one on the cover of the National Enquirer tabloid.
- Multiplace chambers, like the hyperbaric suites used at Aviv Clinics, are spacious, comfortable rooms that accommodate multiple people at once. Aviv’s suites resemble a first-class airplane seat, with comfortable seating, personal entertainment tablets, and a medical team member inside the chamber during every treatment. Instead of being pressurized with 100% oxygen, these suites are pressurized with medical-grade air, and patients breathe oxygen through a specialized mask.

Aviv Clinics – Multiplace HBOT suite
What about soft-sided “mild” chambers?
A growing number of people are asking this hyperbaric oxygen therapy question, as many clinics tout the use of soft-sided “mild HBOT” chambers. However, these portable bag chambers are only approved for treating altitude sickness. They also operate at much lower pressures than hard-sided monoplace and multiplace chambers, limiting their therapeutic effect. Additionally, many clinics that offer “mild HBOT” often don’t meet the rigorous regulatory or fire safety code requirements for HBOT facilities.
2. What Conditions or Goals Does This HBOT Program Support?
HBOT can be used for a wide range of medical and wellness goals. Some clinics treat only acute wounds or infections, while others, like Aviv Clinics, offer research-backed programs that address cognitive decline, brain injury, PTSD, and more. Choose a clinic aligned with your specific condition or health objective.
Traditional HBOT facilities only treat acute conditions like gangrene, infections, burns, or decompression sickness. HBOT has been used for decades to treat these “on-label” conditions, which are typically urgent, treated at hospitals, and covered by insurance. In these instances, the number of HBOT treatments can be as few as one or two sessions.
Other facilities offer spa-like experiences, providing “wellness” dives without a clear protocol or clinical oversight.
In contrast, the research-backed Aviv Medical Program treats conditions that affect brain and body function. These include:
- Age-related cognitive and physical decline
- Stroke recovery
- Traumatic brain injury (TBI) and post-concussion syndrome
- PTSD
- Fibromyalgia
- Long COVID
- Lyme disease
- Chronic carbon monoxide poisoning
- Athletic performance issues
- Surgical recovery
3. Is the HBOT Protocol Backed by Scientific Research?
Many facilities offer hyperbaric oxygen therapy without peer-reviewed evidence or standardized protocols. Ask whether the treatment is rooted in science, and how the facility’s protocols compare to those used in the clinical trials. Every treatment you choose can affect your body positively or negatively, so doing your research and choosing a reputable clinic is paramount.
The pressure and length of treatments, as well as the oxygen dosage used in Aviv’s HBOT treatments, are the result of peer-reviewed scientific research. Aviv Clinics’ HBOT treatment protocol is based on nearly two decades of rigorous, published research. It was developed at the Sagol Center for Hyperbaric Medicine and Research, the world’s most advanced facility of its kind. The Aviv Protocol is uniquely designed to spark the body’s innate capacity for regeneration using oxygen fluctuation techniques, a method known in the scientific community as the hyperoxic-hypoxic paradox. In clinical trials, this protocol has proven to stimulate stem cell activity, reduce inflammation, and improve blood flow in the brain and tissues.
Notably, this protocol is difficult to replicate in single-person monoplace chambers and is not possible to administer in low-pressure “mild” chambers.
4. Who Makes Up the Clinical Team Supporting the HBOT Program?
An important hyperbaric oxygen therapy question is to ask about the type of expert on-site support available for treatment and guidance. Some clinics operate more like spas, with minimal or no clinical oversight by an on-site physician. Others focus narrowly on wound healing, with limited scope for treating complex or neurological conditions.
At Aviv Clinics, clients have access to a multidisciplinary team that includes:
- Hyperbaric physicians
- Clinical psychologists and neuropsychologists
- Physical therapists
- Physiologists
- Nutrition specialists
- Nursing professionals
5. Will Medical Staff Be Present During My HBOT Sessions?
Hyperbaric oxygen therapy is a medical treatment, so professional oversight and support during your sessions are critical. Some facilities and spas offering mild HBOT don’t even have a physician on site during treatments, or choose to monitor clients remotely via video feed.
Aviv Clinics offers a medically supervised HBOT experience:
- A nurse or other medical professional is inside the multiplace suite to provide care during every session
- A trained hyperbaric technician monitors each session from a control console next to the HBOT suite
- A physician is on site at all times during hyperbaric treatments.
Your safety and comfort are always top priorities.
6. What Pre- and Post-Treatment Assessments are Included?
If a clinic doesn’t offer detailed assessments before and after treatment, there’s no objective way to track your progress. At a minimum, your provider should conduct a detailed medical history and physical examination and a chest x-ray before hyperbaric treatment. Depending on your individual needs, you may also need blood work or heart and lung function testing to determine your suitability for the treatment.
In addition to these assessments, the Aviv Medical Program can include the most comprehensive battery of pre- and post-treatment evaluations available.
At your request, these cognitive and physical tests can include:
- Extensive blood panels
- High-resolution brain imaging with MRI or SPECT
- Cognitive testing to measure memory, attention, and other cognitive domains
- Cardiopulmonary exercise test (CPET)
- Body composition analysis
- Gait, balance, and overall motor function assessment
- Stem cell count and assessment of aging biomarkers
These assessments help define your health goals, guide your physician-prescribed treatment plan, and track measurable improvements.
7. Will I Receive a Detailed Report of My HBOT Progress?
Too often, clients leave HBOT clinics with no clear understanding of their results. Some facilities that work on a session-to-session basis may only provide minimal or per-visit tracking. Others may not offer results at all.
While some of our clients are perfectly happy with simply “feeling better,” others prefer a detailed before-and-after report. For those clients, we offer in-depth post-treatment reporting. Depending on your condition or reason for treatment, this report may track changes in:
- Physical health
- Cognitive performance
- Brain imaging
- Aging biomarkers
- Cellular health
- Condition-related metrics
Clients review their progress one-on-one with their Aviv Clinics physician, who explains and interprets the data and provides next steps.
8. Will The HBOT Clinic Coordinate With My Physician?
Some hyperbaric clinics operate outside the traditional medical system and don’t communicate with your personal healthcare team. If you’re working with a physician, specialist, or other provider, it’s important to choose an HBOT program that can integrate with your broader care plan.
At Aviv Clinics, we consider ourselves part of your overall care team. With your permission, we’ll coordinate directly with your existing physicians, share your assessment data and progress reports, and provide pre- and post-program evaluations for your permanent medical record.
Some clients are hesitant to tell their doctors that they’re exploring HBOT or other nontraditional therapies, but Aviv Clinics encourages transparency. In fact, many physicians are excited when they learn about the science behind our program and the measurable improvements their patients experience. We believe collaboration leads to better outcomes, and we’re here to support your health journey from every angle.
The Bottom Line: Not All HBOT is Equal
Before you invest time and money, make sure you know what you’re getting by asking these hyperbaric oxygen therapy questions. Your HBOT treatment protocol should be scientifically validated, supported by a caring, expert medical team, and offer a full range of assessments to show your progress.
This comprehensive approach allows Aviv Clinics’ clients to improve memory, regain physical stamina, and live with greater clarity and resilience.
Contact us to learn more about the Aviv Medical Program and how it can benefit you.
Last Update: July 10, 2025
Seasonal Affective Disorder: How Winter Darkness Impacts Mood and Brain Health
Shorter days, cooler temperatures, and less sunlight can trigger mood and cognition changes in some people. Seasonal Affective Disorder (SAD) can impact brain health, but it is treatable.
What is Seasonal Affective Disorder?
SAD is a type of depression that emerges as seasons change. People who experience seasonal affective disorder can feel anxious, irritable, fatigued, sad, and have trouble sleeping, staying engaged, or thinking clearly. Some may even have thoughts of death and suicide, lose their appetites, and experience weight gain or loss.
Symptoms of winter-pattern SAD typically begin when the days get shorter in the fall and winter. Many describe it as winter blues. Symptoms typically subside with the onset of change of seasons.
Who is Most Affected by SAD?
Mental Health America estimates that about five percent of the U.S population suffers from seasonal depression, and four out of five people with SAD are women. However, many people may not even realize their depression is linked to seasonal changes, according to the National Institute of Mental Health. Not surprisingly, winter-pattern SAD is more common in people living farther north, where there are fewer sunny days and fewer hours of daylight in the winter.
Researchers are still studying the mechanisms of seasonal affective disorder. The National Institute of Mental Health notes that “SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.”
The condition can also be more common in people with major depressive disorder or bipolar disorder. Those with attention deficit hyperactivity disorder (ADHD), an anxiety disorder, or an eating disorder are also more prone to developing SAD. It can also impact more than one family member.
How Seasonal Changes Affect the Brain
Sunlight helps the body produce vitamin D, which is essential for maintaining serotonin, a neurotransmitter in the brain. Insufficient levels of serotonin can negatively affect mood and cognition because the brain is not firing properly. If these neurotransmitters are not firing, memory, learning, and concentration can all suffer
When the season shifts to fall and winter, and days become shorter, there is less sunlight available and less opportunity to produce vitamin D.
Shorter days also can interfere with the circadian rhythm or sleep-wake cycle, resulting in an overproduction of melatonin, a hormone critical for maintaining the body’s normal daily rhythm. Too much melatonin can cause sleepiness and reduce energy.
Lifestyle Factors That Can Worsen Symptoms
Shorter days and less sunlight not only rob the body of vitamin D, but also tend to spend more time indoors and potentially become less active. The lack of physical activity and social interaction because of being indoors can exacerbate SAD symptoms. Neither the brain nor the body has much energy, leading to increased fatigue and worsening symptoms.
Eating poorly can also intensify symptoms. Winter holidays like Thanksgiving are celebrated with hefty feasts that often include sugar-laden foods, lower-quality carbohydrates, and highly saturated fatty foods, which can create inflammation in the body. Studies have shown that sugary drinks, refined carbs, trans fats, processed foods, artificial sweeteners, and alcohol can increase inflammation and impact memory and learning.
Treating Seasonal Affective Disorder
SAD is mainly treated with light therapy. Other methods that may be used in conjunction with light therapy include talk therapy, vitamin D supplementation, and antidepressant medications.
- Light therapy. To make up for the loss of sunlight, a SAD sufferer can soak up intense light using a light box, which provides up to 20 times more light than ordinary indoor light without the damaging UV rays associated with natural sunlight. To reap the most benefit, the person should sit 30 to 45 minutes each morning in front of the box. Light therapy is not recommended for someone with bipolar disorder, however, because the intense illumination can lead to a manic episode.
- Talk therapy. Because some people associate winter with negative thoughts, psychotherapy may be beneficial to help restructure thinking. Talk therapy works well in conjunction with light therapy.
- Medications. For some people with SAD, antidepressants may be useful. Medications called selective serotonin reuptake inhibitors (SSRIs) are used to treat SAD when symptoms occur.
- Vitamin D supplements. A lack of sunlight will result in a vitamin D deficiency. A vitamin D deficiency causes fatigue, bone pain, muscle weakness, and mood changes like depression. Although sunlight is the best and preferred source for vitamin D, light therapy, food, and nutritional supplements are alternative sources.
Recognizing When to Seek Help for SAD
If symptoms of SAD interfere with quality of life, it’s time to talk to your doctor.
Can the symptoms of seasonal affective disorder be prevented? All of the symptoms may not be entirely preventable, but there are things you can do to reduce the severity of how you feel.
- Begin light therapy before the onset of symptoms.
- Take advantage of daylight hours to exercise outdoors.
- Be socially active even when you feel like you would rather stay indoors.
- Choose brain-beneficial foods that promote good mental health.
- Maintain your sleep routine and cycle.
How Aviv Clinics Can Support Brain and Mood Health
Understanding the root causes of mood and cognitive shifts is key to personalized treatment for seasonal affective disorder.
At Aviv Clinics, our multidisciplinary team includes clinical psychologists and neuropsychologists who assess and treat changes in cognitive functioning. By integrating mental health support with other evidence-based interventions in the Aviv Medical Program, we help clients better understand the factors contributing to their symptoms and offer proactive solutions.
Can Sleep Apnea Cause Memory Loss? How OSA Affects Brain Health
Obstructive sleep apnea (OSA) is a breathing disorder characterized by the blockage of a part or all of the upper airway that occurs during sleep. An estimated 30 million Americans suffer from sleep apnea, although 80% of these cases are undiagnosed. Poor quality sleep is already associated with weight gain, issues with blood sugar, lower immunity, cardiovascular problems, and psychological concerns. OSA compounds these potential issues by intermittently depriving the brain of oxygen (a condition known as hypoxia). Over time, these nightly lapses in breathing can lead to long-term damage to brain structure and function.
Why Treating Sleep Apnea Matters for Memory and Brain Function
If left untreated, changes in the brain caused by OSA can cause:
- Strokes
- Impaired memory
- Depression
- Headaches
- Mild cognitive impairment
- Alzheimer’s disease
OSA is common in adults aged 65 and older. However, physicians often fail to see the causal connection between OSA and cognitive impairment, meaning cognitive decline may have already begun by the time sleep apnea is diagnosed.
Fortunately, treating OSA can improve a patient’s quality of life and prevent further neurodegenerative decline.
How Sleep Apnea Disrupts Brain Health and Causes Memory Loss
OSA episodes can occur many times throughout the night. Even in mild cases, a patient may stop breathing five times an hour, and in severe cases, there may be more than 30 events an hour. Each episode interrupts the flow of oxygen to the body and brain. This results in damage to every cell in the body.
These repeated interruptions in sleep:
- Prevent deep, restorative REM sleep
- Impair memory consolidation
- Inhibit the brain from removing waste
- Cause cellular damage
- Disrupt mood, focus, and recall
Sleep apnea is also associated with an increased risk of developing cognitive decline and dementia, including vascular dementia and Alzheimer’s disease. Over time, the brain may begin to accumulate plaque, a key biomarker of Alzheimer’s disease. Research suggests that proper oxygen-rich blood flow in and out of the brain is critical to preventing this buildup.
Common Signs and Symptoms of OSA
Early diagnosis of sleep apnea is essential to avoid potential long-term cognitive effects. Common signs include:
- Snoring loudly and frequently. Often, people do not realize they snore. But if you notice you awaken frequently and suddenly throughout the night, this may be because your snoring is disrupting your sleep. If you have a partner, they can attest to the type of snoring, which is helpful when meeting with a physician.
- Experiencing excessive daytime sleepiness. A person with OSA may wake up feeling tired, even after a full night of sleep. Daytime drowsiness associated with OSA may emerge while reading, watching TV, or driving. People living with sleep apnea may also report brain fog or issues with memory throughout the day.
- Waking suddenly, gasping for air. People with OSA are often jolted awake when they stop breathing, because the airway has narrowed or collapsed. They may also wake with a dry mouth because they’ve been breathing through their mouth to draw in more oxygen.
To confirm an obstructive sleep apnea diagnosis, your physician may recommend an at-home sleep study or overnight monitoring at a sleep clinic. These studies usually involve wearing an apparatus that will measure your oxygen level, heart rate, and respiration while you sleep.
What Causes Obstructive Sleep Apnea?
Several anatomical and health-related factors may contribute to the development of obstructive sleep apnea, including
- Large neck circumference
- Obesity
- An enlarged uvula
- Blocked nasal passages (from issues like allergies or a deviated septum)
- Swollen tonsils or adenoids
- Smoking or alcohol use
- Medical conditions like type 2 diabetes and high blood pressure
Treating Sleep Apnea to Prevent Cognitive Decline
Treatment of obstructive sleep apnea includes nonsurgical and surgical approaches. Nonsurgical methods include:
- Weight loss: Losing weight, especially around the neck, can significantly improve OSA symptoms.
- Continuous Positive Airway Pressure (CPAP): This method uses a mask-style apparatus that prevents partial or complete collapse of the airways while sleeping. It forces compressed air into those compromised areas to prevent obstruction.
- Oral appliances: Those averse to machines may prefer oral appliances. These mouthpieces are crafted to open your airways by either bringing your jaw forward or holding your tongue in place.
- Surgical options: Procedures can be performed using conventional or laser techniques to alter or remove any physical obstructions, like adenoids or enlarged tonsils. Other surgical methods may include altering the jawbones, soft tissue, or nose.
For those experiencing cognitive decline from obstructive sleep apnea, Aviv Clinics’ proprietary Aviv Medical Program can help reverse damage caused by OSA. Our board-certified physicians can prescribe a personalized treatment program to address your cognitive and physical concerns. Depending on your lifestyle, health conditions, and symptoms, your customized Aviv Medical Program may include an evidence-based hyperbaric oxygen therapy protocol, cognitive exercises, physical training, nutritional coaching, and other interventions as prescribed. 96% of Aviv Clinics clients experience clinically verifiable improvements in brain function after completing the program.
Why Early OSA Treatment is Critical for Brain Health
Untreated OSA can impair memory, learning, and concentration, and undermine long-term brain health. The long-term effects can be debilitating. Studies have shown that untreated OSA can lead to decreased brain activation, diminished memory recall, and impaired learning.
The good news is that OSA treatment can improve these symptoms, curtail further neurodegeneration, and preserve your brain function.
The Bottom Line: Sleep Apnea, Memory Loss and Your Brain
Obstructive sleep apnea is more than just snoring. It’s a serious condition that can accelerate cognitive decline and other health issues. If untreated, symptoms will worsen with age.
The good news? With the right treatment, these effects can be treated. Based on nearly two decades of research and development, the Aviv Medical Program is available in the United States only at Aviv Clinics in The Villages, Florida
If you suspect you are experiencing sleep apnea, you can get help to improve—and even resolve—symptoms like daytime sleepiness, brain fog, and memory lapses.
Contact Aviv Clinics today to schedule a consultation and explore how the Aviv Medical Program can help you reclaim your brain health.
Last Update: July 9, 2025
Diagnosed with Cognitive Decline? Here’s What to Do Next to Protect Brain Health
You’ve Been Diagnosed With Cognitive Decline. Now What?
Whether your cognitive decline diagnosis indicates mild cognitive impairment (MCI), dementia, or Alzheimer’s disease, exploring the possible causes is the first step in moving forward.
Symptoms, like forgetting where you placed your glasses, frequently asking the same questions, or failing to recognize familiar people, may have led you to seek medical attention. Perhaps your family noticed changes in your mood or personality and urged you to see a doctor. While your diagnosis is likely frustrating and disconcerting, the most important thing is how you proceed from here.
Sometimes, cognitive issues are caused by something treatable like high blood pressure, high blood sugar, stress, anxiety, medications, or drug and alcohol use. No matter the cause of your decline, the key is to address those factors that can be controlled and treated, then choose a healthier lifestyle moving forward.
Understanding Cognitive Decline and How It Affects Daily Life
Cognitive impairment occurs when a person experiences difficulty remembering, learning new things, concentrating, or making decisions that impact their everyday life. It can range from mild to severe, escalating to the point where the person loses the ability to comprehend, write, or speak. At that stage, a person can no longer live independently.
Age is the greatest risk factor for cognitive impairment.
According to the CDC, cognitive disabilities affect 13.9 million Americans, making it the most common type of disability in the U.S. The Alzheimer’s Association estimates that 7.2 million Americans aged 65 and older currently have Alzheimer’s disease. That number translates to roughly 1 in 9 older adults.
Six Actions to Take After a Cognitive Decline Diagnosis
Stress and anxiety will most certainly follow on the heels of a diagnosis. Learning to cope in healthy ways will be crucial because stress and anxiety can worsen symptoms of cognitive decline. You may be tempted to isolate because you fear being embarrassed by your condition or want to hide your frustration when you are challenged to remember. However, do not shy away from being challenged. Do just the opposite. Interact even more and engage in things that bring you joy. How you proceed after diagnosis could slow the progression or alter the trajectory of the disease.
Here are six things to do immediately, no matter the diagnosis:
- Eat a balanced diet with plenty of brain-beneficial foods, including blueberries, nuts, leafy vegetables, and fatty fish like salmon, tuna, and sardines. Fatty fish contain omega-3 fatty acids, which the brain uses to build neurons, and are essential for learning and storing memories.
- Exercise for at least 30 minutes, five times a week. When you exercise, you feed your brain with oxygen and other nutrients vital for its functioning.
- Challenge your brain daily with activities that keep it stimulated. They help exercise the brain, enhance creativity, improve problem-solving, and may slow memory decline.
- Get adequate sleep. Stay away from things that may overstimulate your brain or body before bedtime. Sleep allows your body to cleanse the brain of toxins and waste. Getting enough is essential.
- Find a good support system. It will be critical to build a good support system now that you have received a diagnosis. Whether it is a spouse, a friend, a family member, or a support group, having social connections can keep you from feeling alone.
- Manage stress. Self-medicating with drugs and alcohol will only worsen the symptoms of cognitive decline. Instead, try journaling, prayer, meditation, exercise, or similar activities to reduce your stress load.

Have you noticed changes in your memory, attention or thinking skills?
Download our free e-book, “What’s Happening to My Brain?” to learn how you can improve your brain health and cognitive vitality at any age.
Is Cognitive Decline Reversible?
In some people, mild cognitive impairment can be reversed or remain stable, especially if it is linked to a medication. For others with a diagnosis of dementia or Alzheimer’s disease, the outlook can be more challenging. Both Alzheimer’s and dementia are progressive conditions, meaning symptoms will eventually worsen. However, making lifestyle changes like healthy eating and exercising may slow the rate of decline.
Maintaining healthy lifestyle choices, including proper nutrition, exercise, social and cognitive activities, and adequate sleep, may help prevent or delay the onset of cognitive challenges.
Hope After Diagnosis: How Aviv Clinics Can Treat Early Cognitive Decline
At Aviv Clinics, we understand how overwhelming a diagnosis of cognitive decline, dementia, or Alzheimer’s can feel. But we also believe that hope doesn’t end with a diagnosis — it starts with a plan.
Our board-certified team of clinical experts specializes in helping people take control of their cognitive future. The Aviv Medical Program is an evidence-based, personalized treatment approach that goes far beyond symptom management. This comprehensive program uses a unique hyperbaric oxygen therapy (HBOT) protocol and advanced diagnostics to prescribe interventions tailored specifically to your concerns. These may include physical training, nutritional guidance, and cognitive exercises to target the causes of your cognitive decline.
Clinical research has shown that the unique HBOT protocol used in the Aviv Medical Program can improve memory, attention, and processing speed in older adults. Studies show it may even reverse key biomarkers associated with Alzheimer’s disease. For individuals looking to protect and optimize brain performance, this program offers a proactive path forward.
Whether your symptoms are mild or more advanced, our goal is the same. We want to help you preserve what matters most — your independence, your memories, and your quality of life.
Contact us to schedule a free consultation and learn how the Aviv Medical Program can help you or your loved one maintain long-term cognitive health.
Last Update: July 9, 2025
Understanding Alzheimer’s Risk: Causes, Prevention, and the Promise of Hyperbaric Oxygen
We all experience occasional memory lapses, especially as we age. For most of us, these minor cognitive issues are usually just annoyances. But if your cognitive issues interfere with your daily life, they could be the beginning of something much more serious.
Read on to learn more about the risk factors for Alzheimer’s disease and how you can preserve your cognitive health.
What Is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia that impacts a person’s ability to think, reason, and remember. As it progresses, Alzheimer’s can severely affect quality of life, eventually becoming completely debilitating.
The most common type of Alzheimer’s disease is the late-onset form, when symptoms usually “become apparent in [a person’s] mid-60s or later.”
10 Early Signs and Symptoms of Alzheimer’s Disease:

According to the Alzheimer’s Association, ten early warning signs of late-onset Alzheimer’s disease include:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks
- Confusion with time or place
- Trouble understanding visual images and spatial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgment
- Withdrawal from work or social activities
- Changes in mood and personality
If you experience a cognitive problem that impacts your daily life, don’t ignore it. Dementia is not a normal part of the aging process. The sooner you seek help, the sooner you can take action against cognitive decline.
Get in touch with our care team>>
What Are the Risk Factors for Alzheimer’s Disease?
Science is still learning how Alzheimer’s disease develops and why some people are at greater risk of developing it than others. It’s an active area of study, and researchers are making new discoveries every day.
The consensus among scientists is that a combination of age, sex, genetic, environmental, and lifestyle factors all contribute to the development of Alzheimer’s disease.
Let’s take a closer look at some of the greatest risk factors for Alzheimer’s:
- Although old age does not directly cause Alzheimer’s disease, the risk of developing Alzheimer’s “doubles about every 5 years” after age 65.
- More women than men develop Alzheimer’s disease, although this may be because women live longer than men on average.
- Suffering from a traumatic brain injury (TBI) can increase the long-term risk of developing Alzheimer’s or another type of dementia.
- Acute and chronic inflammation are both associated with an increase in cognitive decline. Eating a diet full of inflammatory foods like processed sugar may exacerbate the risk of developing inflammation in the brain.
- Exposure to environmental pollutants has been linked to an increased risk of dementia. Some researchers believe that nearly half of the individual differences in Alzheimer’s risk may be because of environmental factors.
- Being a smoker carries a significantly increased risk of developing Alzheimer’s disease. This risk factor offers another compelling reason to quit.
- People with Down syndrome also have a greater risk of developing Alzheimer’s disease. About 30% of people with Down syndrome develop Alzheimer’s disease by their 50s. The risk reaches closer to 50% in their 60s.
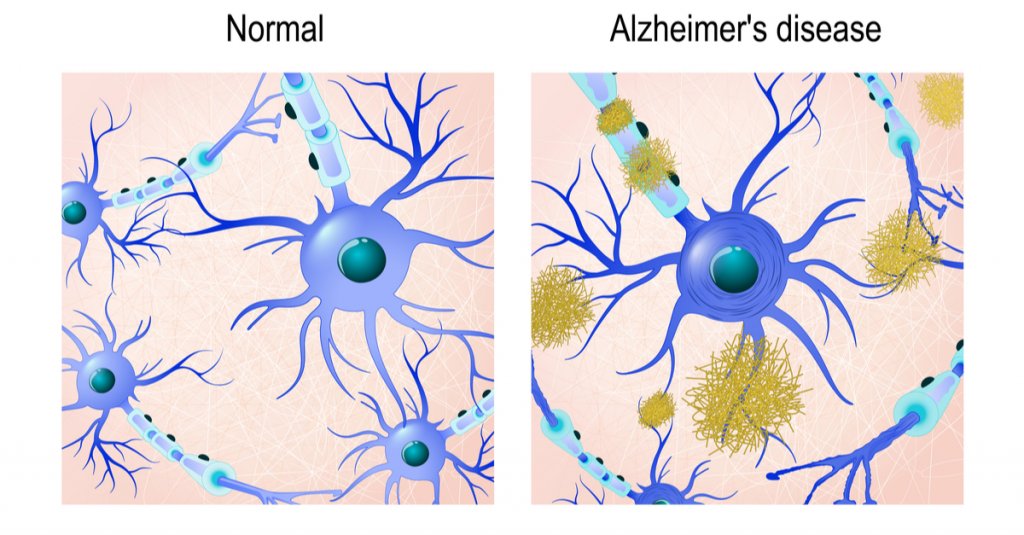
The Role of Brain Proteins in Alzheimer’s: Amyloid Plaques and Tau Tangles
Scientists typically focus on two different protein structures in the brain associated with Alzheimer’s disease: Neurofibrillary tangles and amyloid plaques.
It’s not currently known whether the presence of these structures causes Alzheimer’s disease or if they’re simply byproducts of it. But both can impair cognitive function and can worsen as the disease progresses.
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a simple blood test available at Aviv Clinics may be able to answer this question: pTau Testing
Neurofibrillary Tangles
Neurofibrillary tangles are accumulations of a harmful protein called tau in the brain’s neurons. These tangles can inhibit the neurons’ ability to communicate, causing cognitive decline. Some studies reveal that a lack of oxygen to the brain is associated with neurofibrillary tangles.
Amyloid Plaques
Amyloid plaques are hard, insoluble clumps of beta-amyloid proteins that build up between neurons. Like neurofibrillary tangles, these plaques are toxic to brain cells and disrupt cell-to-cell communication. They can eventually result in cellular death, harming cognitive abilities even further.
Brain scans can reveal the presence of both protein structures, so your doctor can alert you to the presence of Alzheimer’s disease or if you’re at risk for developing it.
Is Alzheimer’s Disease Genetic?
Both early-onset and late-onset Alzheimer’s disease have a genetic component, meaning if you have a family history of Alzheimer’s, you carry a greater risk for developing the disease. The risk factor is greater if an immediate family member suffers from the disease, such as a parent or sibling.
Genetics are almost always the primary contributing factor of early-onset Alzheimer’s disease, which can affect people as young as their 30s or 40s.
Gene Mutations
Researchers have yet to identify any specific genes directly responsible for the development of late-onset Alzheimer’s. However, certain mutations of the APOE gene, which are found on chromosome 19, are currently considered the strongest genetic risk factor for Alzheimer’s disease.
For example, the specific gene mutation APOE ε4 is linked to higher levels of amyloid plaques and is often found in people with Alzheimer’s disease.
Your doctor may order genetic testing if you have a family history of cognitive problems or early-onset dementia.
Remember, this doesn’t mean you’re destined to develop Alzheimer’s if a parent or sibling has had it. Some people who possess the APOE ε4 gene never develop Alzheimer’s disease, and some people with Alzheimer’s don’t have any gene mutations at all.
Genetics is just one of many Alzheimer’s risk factors. We still need more research to develop a complete picture of what the largest risk factor for Alzheimer’s disease is.
Can Hyperbaric Oxygen Therapy Help Prevent Alzheimer’s Disease?

A specific hyperbaric oxygen therapy (HBOT) protocol shows promise as a potential preventative measure for Alzheimer’s disease. HBOT is a treatment that involves breathing 100% oxygen in a pressurized chamber to increase oxygen levels in the body and brain. A unique HBOT protocol used at Aviv Clinics has shown several benefits in individuals at risk for or experiencing early cognitive decline:
Benefits of HBOT for Alzheimer’s Disease:
- Improves brain tissue oxygenation
- Lowers neuroinflammation (inflammation in the brain)
- Shrinks beta-amyloid plaques (in laboratory animals)
- Reduces pTau protein levels (in laboratory animals)
- Improves memory recall and cognitive performance
- May slow or reverse early signs of cognitive decline
These benefits have been documented in peer-reviewed studies. This specialized HBOT protocol is available exclusively at Aviv Clinics in Central Florida.
In one study, repeated HBOT sessions showed reduced brain hypoxia, reduced amyloid plaques and pTau, and improvements in cognitive performance. Another study found improvements in memory recall in people with mild cognitive impairment (MCI), a potential early stage of Alzheimer’s. Researchers concluded that HBOT “should be considered as a therapeutic approach to slow the progression or even improve the pathophysiology responsible for [Alzheimer’s] disease.”
Lifestyle Habits That May Lower Your Alzheimer’s Risk
While none of us can change our genetic makeup, we can change our lifestyle. Healthy habits can help lower your risk factor for nearly any disease, not just cognitive conditions. Lowering inflammation levels in your body can also help lower inflammation in the brain. To help preserve your cognitive health:
- Eating a healthy diet full of fruits and vegetables
- Exercising regularly
- Maintaining healthy blood pressure
- Keeping your mind active
- Maintaining a healthy weight
- Practicing mindfulness and meditation
- Avoiding excess alcohol
- Avoiding smoking
- Getting plenty of restful sleep
- Taking care of your mental health
How the Aviv Medical Program Can Support Brain Health
The Aviv Medical Program is a personalized intervention designed to improve brain and body health. Using the unique HBOT protocol discussed earlier, alongside other evidence-based interventions, this program can treat both physical and cognitive performance in older adults. In clinical trials, this protocol has also reversed key biomarkers of the aging process.
Depending on your symptoms, needs, and goals, our clinical team will perform an assessment that may include:
- In-depth medical history review
- Comprehensive physical and neurological exam
- Physical therapy evaluation
- Highly advanced brain imaging scans
- Neurocognitive tests
Once our board-certified physicians review your results, they’ll prescribe a customized treatment program designed to treat your concerns. This program may include:
- A specialized hyperbaric oxygen therapy protocol
- Physical training
- Dietary coaching
- Cognitive exercises
- Other interventions as prescribed
Real Client Results: Carl and Vickie’s Cognitive Improvements
Married couple Carl and Vickie both had parents with dementia and cognitive decline. They soon realized they were beginning to experience the same cognitive issues that they saw in their parents.
The couple’s quality of life was not where it should have been, so they took action with the Aviv Medical Program. They use one word to describe their improvements in cognitive performance: “remarkable.”
I’m dancing, I’m hiking, I’m running again. It’s just remarkable. I don’t know how else to say it.” –Vickie Eckert, Aviv Medical Program Alumna
Take Control of Your Brain Health With Aviv Clinics
While science is still investigating all of the risk factors for Alzheimer’s disease, anyone can lower their likelihood by taking charge of their lifestyle.
Preserving your cognitive health starts with the choices you make every day. Partnering with Aviv Clinics is just one of them. Contact our medical team to learn how we can help you.
Last Update: July 8, 2025
How Anxiety Affects Brain Health: Long Term Impact and 7 Natural Ways to Cope
Worry and everyday stressors are common triggers for anxiety, a condition that ignites areas of the brain responsible for detecting and responding to real-life threats. Anxiety affects brain health because it produces the “fight-or-flight” response, which can “make the heart pound and breathing quicken.”
Anxiety disorders are the most common mental health concern in the U.S., affecting 40 million adults. Those who live with anxiety are all too familiar with the cascade of physical symptoms, from a racing heart to sweating to hyperventilating.
What you may not realize, however, is that all those episodes of anxiety may be harmful to the brain, especially if the anxiety goes untreated for a long period.

What Is Anxiety and How Does it Affect the Brain?
Anxiety is a feeling of worry, dread, or nervousness. It is an emotional and physiological response to an impending event or an uncontrollable situation. In severe cases, this state of apprehension can lead to compulsive behaviors or panic attacks.
It’s perfectly normal to experience some degree of anxiety in certain situations, like having to give a speech in front of an audience or taking a test.
When anxiety becomes chronic and excessive, or interferes with your quality of life, that’s when the brain begins to experience its negative effects.
Common Causes of Anxiety and Brain Dysfunction
Several variables can lead to chronic anxiety:
- Genetics
- Brain dysfunction or injury
- Post-traumatic stress syndrome
- Environmental stressors like abuse and neglect
- Substance abuse
- Medical conditions like thyroid disease
- Repetitive negative thinking
How Anxiety Affects Brain Health (and the Fight or Flight Response)
When a person experiences anxiety, the brain’s amygdala, hippocampus, and prefrontal cortex (PFC) become hyperactive.
These parts of the brain are responsible for sensing danger, whether that danger is real or imagined. They trigger a surge of adrenaline and cortisol (the stress hormone) throughout the body in response to that perceived danger. This activates the fight-or-flight response.
The reaction serves the body well in a truly life-threatening situation because the adrenaline and cortisol allow the body to react quickly with heightened awareness. In these cases, the brain is doing exactly what it’s designed to do to protect the body.
However, your brain’s well-equipped, danger-interpreting processes may be impaired by unhealthy reasoning and inappropriate thought responses. How your brain interprets the perceived threat will dictate how well you can quell the fight-or-flight response and return to a state of calm.
Excessive and prolonged anxiety affects brain health by producing an overabundance of stress hormones. This can ultimately lead to panic attacks, a more severe side of anxiety.
An overly anxious brain becomes much like the boy who cried wolf: always on high alert for incoming danger, despite many false alarms. In this heightened state, the brain has a harder time reasoning rationally and is less able to interpret real-life danger.
What Research Says about Anxiety and Brain Health
Studies illustrate that stress reduces hippocampal volume. The hippocampus processes long-term and contextual memory, so persistent anxiety can impact the brain’s ability to store and access our memories.
Stanford University biological sciences professor Robert Sapolsky noted that research “shows links between long-term stressful life experiences, long-term exposure to hormones produced during stress, and shrinking of the part of the brain involved in some types of memory and learning.”
That makes treating anxiety early ever more critical as you move closer to your golden years, especially because stress can have other negative impacts on the brain.
7 Natural Ways to Reduce Anxiety and Protect Brain Health
The first step in overcoming anxiety is recognizing that there is a problem. If you notice any of these signs, it’s time to seek help:
- Your anxiety is limiting your ability to enjoy life.
- You’re consistently unable to sleep.
- You feel irritable.
- You notice changes in your appetite.
- You’re experiencing physical and mental changes.
Medications are available to help cope with anxiety. However, cognitive therapy can assist in restructuring reasoning and ultimately relieve chronic anxiety. The goal of cognitive therapy is to replace the negative self-talk during an anxiety-driven episode with more realistic and reasonable thought processing. This ultimately works to de-escalate the fight-or-flight response.
Stress or anxiety occurs when our pressures exceed our resources. Here are seven healthy coping strategies to incorporate into your daily life for managing stress and the effects of anxiety on brain health:
1. Use Self-Care to Calm an Anxious Brain
Listen to music, meditate, get a massage, or practice yoga. Wellness apps such as Headspace offer meditation and yoga guides, as well as relaxing music to help you wind down.
Look into local massage therapy services, such as kneading or face/neck rubbing, to reduce tension in your body.
2. Eat a Brain-Healthy Diet to Ease Anxiety
Choose healthy options and avoid overeating. Consider following the MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet.
MIND is a blend of two diets:
- Mediterranean: A heart-healthy eating plan
- DASH: Addresses hypertension or high blood pressure
This evidence-based diet encourages you to consume a variety of fruits, vegetables, and healthy fats and proteins, and is linked to better cognitive function, memory, and increased brain volume.
3. Cut Back on Alcohol and Caffeine to Manage Anxiety
Despite some feelings of stimulation, alcohol depresses the central nervous system and can worsen symptoms of anxiety. So can caffeine, which is a stimulant. Instead, drink more water. Although conventional wisdom tells us that most people should drink about four to six cups of water each day, the total amount we should consume varies. For example, if you’re exercising or sweating heavily, you may need at least two to three cups of water per hour.
Non-caffeinated teas, such as chamomile tea, are well known for their relaxing properties, and you can enjoy them any time of the day.
4. Improve Sleep to Reduce Chronic Anxiety Symptoms
Stress can disrupt sleep. Create a healthy environment conducive to a good night’s sleep. Experts recommend that healthy adults get an average of 7 to 9 hours of sleep per night.
Here are some tips:
- Shut down all electronics an hour before bedtime. Too much screen time in the evening can disrupt the surge of melatonin we need to fall asleep.
- Read a good book or take a warm bath. These activities help your mind and body wind down.
- Keep a consistent sleep schedule. This will encourage your circadian rhythm to stabilize.
- Keep a cool temperature in your room. Our body temperature naturally drops in the evening, so a cooler room can help reinforce your body’s natural instinct for slumber.
5. Boost Brain Health with Regular Exercise
Shoot for at least 30 minutes of moderate exercise at least three days a week. To help motivate yourself to exercise consistently:
- Find a type of movement you love. Whether gardening, dancing, playing pickleball, or golfing, stick to an activity that makes you feel good.
- Start small and work your way up. Don’t start with high-intensity exercises. You don’t want to get burned out or suffer an injury. Instead, start with light activities like a brisk walk, and as you become more comfortable and confident, gradually build the intensity.
6. Reduce Anxiety Through Social and Spiritual Support
Lean on trusted friends, family members, or faith leaders for support. They can offer a listening ear, honest advice, or an activity to get your mind off stressors. Simply talking with someone can often ease anxiety.
7. Seek Professional Help for Chronic Anxiety
If you’re feeling overwhelmed by anxiety, talk to your family doctor or seek help from a therapist. Speaking to a professional can help you process your feelings and suggest personalized ways to cope.
Each person is different, so seeking a customized approach from a therapist or doctor can make a big difference, especially if you haven’t seen any improvements from the strategies listed above.
Final Thoughts: Controlling Anxiety to Protect Long-Term Brain Health
Anxiety affects brain health, but it is both treatable and controllable. There are healthful ways to cope with anxiety, so you can protect your brain from its potential detrimental effects. With practice, you can learn how to take a deep breath, assess a situation appropriately, and avoid an impending wave of anxiety.
For more help on enhancing your physical and cognitive performance, contact Aviv Clinics in The VillagesⓇ.
Last Update: July 8, 2025

