
Understanding the Link Between PTSD and Traumatic Brain Injury (TBI)


PTSD and Traumatic Brain Injury: A Complicated Relationship
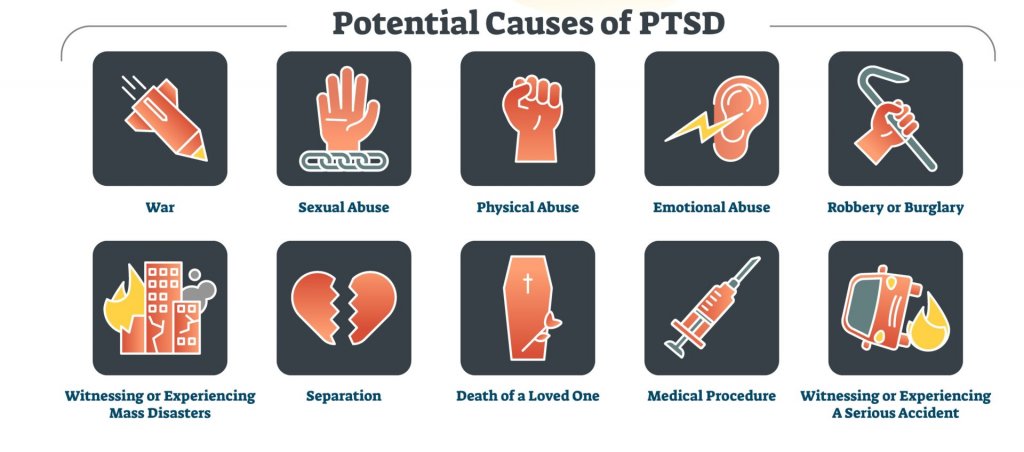
War Veterans probably spring to mind when most people think of post-traumatic stress disorder (PTSD). But many kinds of traumatic events can cause people to develop PTSD.
About 60-75% of Americans will experience at least one traumatic event during their lifetime, and the majority will experience more than one. Events could include natural disasters, life-threatening accidents, physical or sexual assault, the sudden death of a loved one, or the diagnosis of a serious illness; even simply witnessing such events can be traumatic.
Not everyone who experiences or witnesses a traumatic event will develop PTSD. Most people will process the trauma and move on. However, between 10 and 20 percent will develop PTSD.
How Post-Traumatic Stress Disorder Affects the Brain and Body
PTSD may take months or even years to develop. It can potentially affect your physical, mental, emotional, and cognitive health in several ways, including:
- Intrusive symptoms such as memories, flashbacks, or nightmares
- Avoidance of people, places, etc. that trigger memories of the event
- Negative changes in thinking patterns and mood
- Emotional changes, including heightened emotions or conversely feeling numb
- Heightened arousal and reactivity
- Cognitive impairments such as memory, attention, or concentration struggles
- Sleep disturbances and/or insomnia
PTSD can develop after physical trauma, such as an injury or accident, or due to psychological trauma alone, such as seeing someone die or being emotionally abused.
Why PTSD and TBI Frequently Occur Together
PTSD shares a considerable amount of overlap with traumatic brain injury (TBI), and researchers are still investigating this connection. Not only are the two conditions difficult for clinicians to distinguish, but they also frequently co-occur.
A large study of U.S. Army soldiers who fought in Operation Iraqi Freedom reported that 43.9% of the soldiers who had TBI with loss of consciousness also met diagnostic criteria for PTSD. Another study reported that having a TBI doubled the risk of developing PTSD.
Traumatic brain injuries are generally caused by a blow to the head, injuries that pierce the skull and brain, or actions such as whiplash that can cause the brain to bump into the skull. Like PTSD, TBI is not limited to combat Veterans; every year, at least 1.5 million people in the US experience a TBI.
What Causes a TBI and How Does it Affect Brain Function?
Depending on the severity, TBI can be classified as mild, moderate, or severe. It’s even possible to have experienced a TBI and not even realize it. Mild TBIs (mTBI), also known as concussions, can involve the following symptoms:
- Headache
- Dizziness
- Nausea
- Fatigue or drowsiness
- Speech problems
- Sensory issues such as a bad taste in the mouth
- Sensitivity to light or sound
In moderate TBIs, the symptoms above can be more severe and accompanied by a loss of consciousness.
Mild TBI and PTSD: When Symptoms Don’t Go Away
Most people with mild and even moderate TBI recover within days to several weeks. However, 15% or more will develop post-concussion syndrome, with ongoing symptoms lasting for more than 3 months. The symptoms include most of the same ones that could have immediately followed the trauma. But it could also include persistent emotional challenges such as mood instability, anxiety and/or depression, and cognitive impairments like mental slowness, difficulties with memory, or concentration issues like brain fog.
Interestingly, those who have a mild TBI are more likely to develop PTSD than those with more severe brain injuries. This may be because those who experience a more violent blow to the head can develop amnesia around the traumatic event. Ironically, this can spare trauma survivors from the flashbacks, nightmares, bad memories, and other PTSD symptoms.
How Mild Brain Injuries May Increase PTSD Risk

The same traumatic event can cause TBI, PTSD, or both, especially if the traumatic event involved psychological as well as physical trauma, such as war combat or domestic violence.
One condition can also affect the course of the other. For example, PTSD that develops following a car accident could complicate recovery from brain injuries sustained; conversely, a TBI may block the person’s ability to get emotional closure from the psychological aspects of the event.
How PTSD and TBI Work Together to Impact Cognitive Function
Until recently, researchers didn’t understand exactly what these conditions were doing in the brain, and in particular how they affected cognition.
According to this review, TBI and PTSD represent “brain disorders with disruptions in neural networks that communicate via long axonal pathways through white matter tracts, termed the “connectome.” The connectome is the brain’s “wiring” pattern; the sum total of billions of neurons and the pathways or routes that they use to carry out their function.
Both TBI and PTSD have been shown to produce neural inflammation, excitotoxicity, and oxidative stress within the brain. These processes, all of which can affect one another, represent normal functions in the body that, under everyday conditions, don’t cause harm. If these functions get pressed into service too often or for too long, they can spiral out of control, leading to cellular damage and physical changes in the brain.
For example, the amygdala is largely responsible for the “raw data” of emotions that arise in the body. But it’s your prefrontal cortex that actually works with the amygdala to regulate emotions. A critical connection between the prefrontal cortex and amygdala may be broken in brains with TBI or PTSD, which could explain the commonly seen lack of emotional control.
How Hyperbaric Oxygen Therapy Can Support Brain Recovery
CBS Sunday Morning featured Dr. Shai Efrati and his research team at the Sagol Center for Hyperbaric Medicine and Research in a story about how hyperbaric oxygen therapy (HBOT) can treat combat veterans and civilians with post-traumatic stress disorder. The same HBOT protocol developed by Dr. Efrati is available in the U.S. at Aviv Clinics as part of the customized Aviv Medical Program.
Watch: A Promising New Treatment for PTSD
Treating PTSD and Brain Injury Together at Aviv Clinics
PTSD and TBI can both be debilitating conditions that greatly affect everyday life for those who suffer from them. However, recent research into the neural mechanisms of these disorders has opened the door for the discovery of new treatment options, including the Aviv Medical Program.
The Aviv Medical Program offers an evidence-based, multidisciplinary approach to help individuals recover from the lingering effects of PTSD and TBI. Using a unique HBOT protocol validated in peer-reviewed studies, the program targets the root causes of cognitive and neurological dysfunction. Each client’s program is fully personalized based on an in-depth assessment by Aviv’s clinical team. To support recovery, Aviv’s board-certified physicians may recommend additional therapies, including cognitive exercises, physical training, and/or nutritional coaching.
For those living with the lasting impact of brain trauma or psychological stress, the Aviv Medical Program offers real, measurable improvement and a renewed path forward. Contact us to learn more.
Last update: July 1, 2025
Aviv Medical Program provides you with a unique opportunity to invest in your health while you age



