
Cortisol and Brain Health: How Chronic Stress Impacts Cognition and Memory


If you have heard of the stress hormone cortisol, it certainly has a negative connotation. Stress is bad, right? So how do the effects of stress on the brain work?
High chronic stress and cortisol can negatively harm the body. You may notice changes in cognition, whether it is challenges with attention, slowed processing, poor memory or word recall, or simply muddled thinking. These shifts may make tasks more difficult than they should be.
However, stress does not inevitably lead to brain fog or cognitive impairment.
Rather, many variables, such as environmental factors, type of situations, and stress severity, affect how your body regulates and releases cortisol. The type of stressors dictates how you, as an individual, respond to them.
Is All Stress Bad for the Brain?
Stress itself is not inherently a bad thing. Our ability to learn, grow, and thrive is dependent on stress.
For example, our muscles need physical stress to grow big and strong. As individuals, we adapt and grow physically, psychologically, emotionally, and socially, in part because of stress.
In fact, if we don’t experience enough stress as babies and toddlers, we can actually develop a maladaptive stress response. It’s been well documented that stress, in small amounts, is beneficial. However, prolonged and/or severe stress can result in the sustained or repeated release of the hormone cortisol. The classic example is exam anxiety—without some stress, you may not prepare for the test.
What is Cortisol and How Does it Affect the Brain?
Cortisol coordinates the physiological stress response. The body releases cortisol when you experience any type of stress (i.e. acute, chronic, and traumatic stress) via the hypothalamic-pituitary-adrenocortical (HPA) axis.
The HPA axis uses two different parts of the autonomic nervous system:
- Sympathetic nervous system for when a threat is detected (our “fight or flight” response).
- Parasympathetic nervous system (PNS) to calm down the system after the threat is gone (the “rest and digest” system).
So imagine you’re on a hike through the woods, and an angry bear jumps out in front of you. What happens in your body?
- As the threat is registered in your brain, a small brain area called the hypothalamus sends out chemical messengers to the pituitary gland — the small endocrine gland at the base of your brain.
- Cortisol rushes to coordinate the physical response. It increases heart rate and respiration, narrows your sensory perception, and tunes out distractions — all in anticipation of avoiding eye contact and backing away from the bear slowly.
- The pituitary gland then sends a different set of hormones to the adrenal glands, positioned atop your kidneys. These adrenal glands release cortisol.
Cortisol’s Function in the Body: Beyond Stress Response
Cortisol has many responsibilities in the body, including regulating metabolism and blood sugar, mediating immune function, and coordinating our stress response.
One of cortisol’s jobs is to relay instructions from one part of the body to the next. But before you dismiss it as “just the messenger,” understand that the messages Cortisol delivers are often critical, depending on the “content” of the message.
Nearly every cell in your body has been found to contain cortisol receptors, from your heart to your gut to your brain. Bone formation, immune response, electrolyte balance, gut function, and circadian rhythm are all partially mediated via cortisol.
Do High Cortisol Levels Always Indicate High Stress?
Although the association between stress and cortisol is certainly there, research has made one thing clear: the stress response is extremely variable. Thus, the association between the two is difficult to connect with specific metrics.
Researchers have yet to identify one definitive biological indicator that conveys a person is under stress. There are many hallmarks of the stress response, including blood pressure, heart rate, and respiratory rate. However, these aren’t reliably caused by stress alone, so other variables can’t be eliminated.
Although it would be convenient if our bodies always responded in exactly the same way, the fact is that the situation is highly complex. There are different types and severities of stressors. The environment makes a difference, and the consequences or costs of various responses matter. And perhaps most of all, individual responses vary considerably depending on a person’s development, beliefs, and predisposition.
Normal vs. Abnormal Cortisol Levels
Cortisol levels rise and fall in the body according to a 24-hour cycle following our circadian rhythm. At midnight, levels of cortisol are very low (if detectable at all). Cortisol then slowly builds up during the night, is highest after waking, then declines steadily throughout the day.
According to the University of Rochester Medical Center, the normal range for blood cortisol levels from 6:00 am to 8:00 is between 10-20 mcg/dL, and levels off around 4:00 pm to 3-10 mcg/dL.
What causes abnormal cortisol levels? There are many causes beyond stress. These can include:
- Long-term use of corticosteroid medications
- Autoimmune disorders
- Inflammation
- Physical trauma
- Pregnancy in the third trimester
- Shift work
- Depression
- Alcoholism
- Malnutrition
How Chronic Stress and Cortisol Impact the Brain
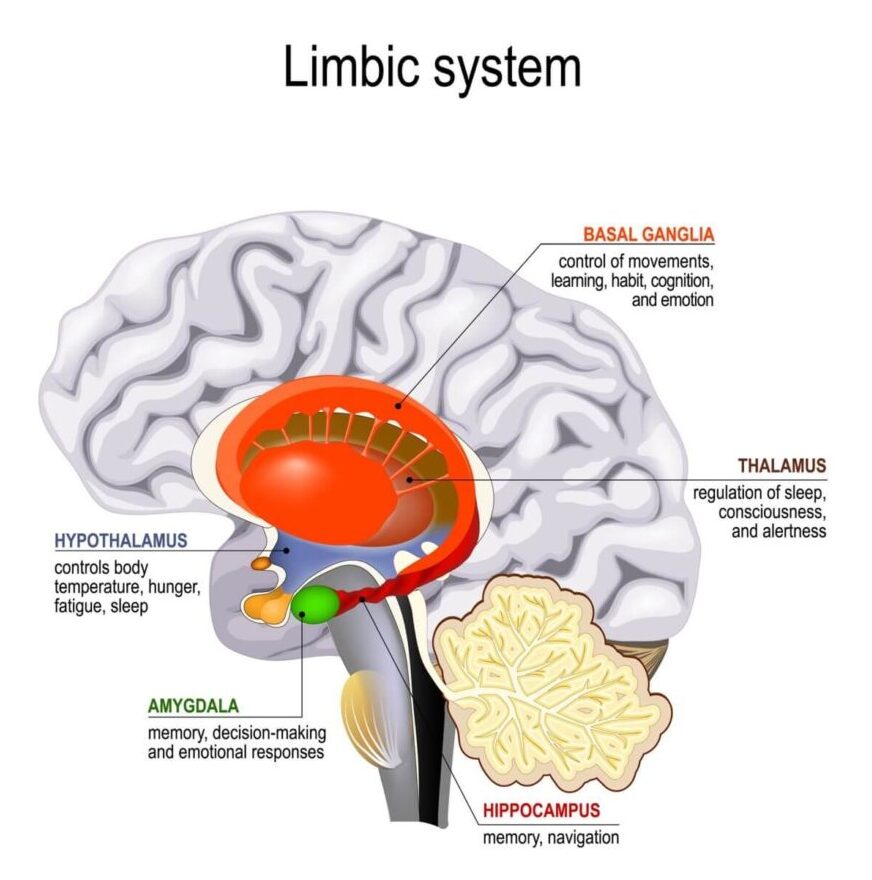
The effects of stress on the brain include functional atrophy of the HPA, hippocampus, amygdala, and the frontal lobe.
Functional atrophy means that the brain is losing neurons and connectivity between those neurons. This can impair brain functions such as thought processing, memory, and emotional regulation.
In general:
- Healthier people have lower levels of overall cortisol throughout the day.
- In less healthy people, there is a difference in the daily cortisol curve: the lows are higher and the highs are lower. Although the peaks are lower, people showing this pattern released more total cortisol compared to healthier subjects.
Cortisol, Cognitive Decline, and Brain Structure
Research indicates long-term high cortisol levels are linked to reduced hippocampal volume, a feature also common in people with depression.
If you have ever felt like stress affects the way you think, that’s in part because of the consequences of high cortisol levels on the brain:
- The amygdala, hippocampus, and prefrontal cortex are the most affected areas of the brain. Together, they control emotions, learning, memory, executive function, and decision-making.
- Mild cognitive impairment (MCI), which is sometimes a precursor to dementia or Alzheimer’s disease, is associated with the hippocampus and elevated cortisol levels.
- Over-exposure to cortisol can kill off brain cells. The hippocampus volume is also lower for people with chronic stress, elevated cortisol levels, and depression.
- HPA activity has been linked to a more rapid decline in patients with Alzheimer’s disease.
Lowering Cortisol Naturally and Managing Stress Effectively

“Reduce your stress” is a phrase commonly used by doctors, therapists, and even friends. Amid the current uncertainty, you might wonder…how, exactly?
Life is unpredictable, and stress is inevitable. Remember that how you respond to stress matters. Although your response may be ingrained, it’s not hardwired. You can learn to respond better to stress and potentially lower your risk for stress-related diseases.
There are many ways to take control of cortisol and stress. Find what works for you.
- Move: Studies show exercise improves hormonal function and your stress response. If you are sitting for prolonged periods, get up every hour at least for 5 minutes–many fitness watches have this reminder.
- Get enough sleep: Sleep at least 8 hours every night. Cortisol is regulated by growth hormone, which is secreted at certain times at night.
- Use stress to your advantage: Stress inoculation has been shown to improve PTSD symptoms.
Balancing Cortisol for Better Brain Health
Stress and the cortisol hormone are not inherently bad, but an inability to cope with them can lead to various physical and mental health issues. Understand your stressors and find healthy coping mechanisms.
Last Update: July 2, 2025
Aviv Medical Program provides you with a unique opportunity to invest in your health while you age




