The Powerful Link Between Music and Memory: What the Science Shows
The Powerful Link Between Music and Memory: What the Science Shows
Music has a special way of interacting with our brains. For a person with Alzheimer’s disease or other significant cognitive impairment, hearing a familiar song can trigger a memory, evoke an emotion, and enhance brain performance.
Studies have shown that music can have a profound effect on people with memory loss conditions, including Alzheimer’s disease and dementia. That growing body of evidence has led some long-term care facilities and caregivers to use music therapy to entertain, soothe, and help socialize residents with dementia and similar issues.
Music is a part of nearly everyone’s life. Many parents use music to soothe a fussy baby, and even for adults, music often serves as a soothing distraction, to elevate mood, as a motivator while exercising, or as a relaxation technique at bedtime. Still others use music as background noise as they go about their daily lives. Music may be such an ever-present fixture in everyday life that it becomes woven into the fabric of the brain. Music stirs our emotions and embeds itself in our memory, creating a link that ultimately becomes associated with a time, a person, or a place.
Why does music unlock memories? It activates those areas of the brain that are associated with memory and emotions: the hippocampus and the frontal cortex. When these areas of the brain are stimulated, they trigger the release of stored memories at the sound of a song.

How Music Impacts the Brain
Music can have a powerful effect on the psyche. For a person with dementia or in late-stage Alzheimer’s disease, music reduces agitation, soothes the spirit, and improves behavior and focus, research shows.
Music’s Effects on the Mind
- Music stimulates the brain by evoking an emotion that triggers a memory. For someone with memory loss, hearing a familiar song has the potential to transport them back to a more pleasurable time.
- It provides comfort. A person with cognitive decline can become easily agitated. Music has a way of reducing agitation and instilling a sense of calm.
- Music elevates mood and reduces stress. Playing music activates a part of the brain that can improve mood and reduce anxiety, especially if the music is familiar and well-liked. Studies have shown that different types of music may have different effects. Soothing music at less than 100 beats per minute, such as classical music, is associated with a positive effect on memory and cognition.
- It creates a connection without verbal communication. For someone in the late stages of Alzheimer’s disease, communicating may be difficult if not impossible. Expose a person with severe memory loss to a song from childhood, and they may break out in song or dance.
Music’s Role in Alzheimer’s and Stroke Recovery
Famed musician Tony Bennett was diagnosed with Alzheimer’s disease many years before his death. However, he was still able to perform and remember the lyrics despite memory impairment.
Music has also been used as a therapeutic method to help stroke patients with aphasia relearn speech. While they may not be able to converse, they can often sing a familiar tune. Using music can stimulate different parts of the brain to relearn and improve speech.
Tips for Using Music as a Caregiver
To use music to soothe a loved one with memory-loss issues, try these tips from the Alzheimer’s Association:
- Choose music your loved one is familiar with and once enjoyed. If they’re able, encourage them to offer suggestions for their customized playlist.
- Play commercial-free music, as interruptions can be disruptive and confusing for them.
- Base your choice of music on the emotion you’re trying to invoke. A tranquil song may induce a calm and serene feeling. A faster-paced tune from their youth might help elevate mood and evoke happy memories.
- Enhance their experience by encouraging them to tap to the beat, clap, or dance.
- Keep distractions to a minimum. Avoid other background sounds, and keep the music volume at a comfortable level. If it’s too loud, it could lead to aggression or agitation.
Supporting Brain Health at Aviv Clinics
The link between music and memory is significant. Studies show that hearing music from our past can trigger strong emotions and a nostalgic connection. Not only can music spark memories, it may also boost mood, calm anxiety, and reduce confusion.
At Aviv Clinics, we understand the deep connection between the brain, memory, and emotion. We designed our comprehensive Aviv Medical Program to address changes in the brain associated with aging, stroke, and conditions like Alzheimer’s and dementia. While music therapy is not a formal part of our program, it aligns with our philosophy: that targeted interventions can help unlock cognitive potential and improve quality of life.
If you or a loved one is experiencing early signs of cognitive decline, our team is here to help guide you.
Last Update: July 9, 2025
Nuts and Seeds: Small Superfoods with Big Brain and Heart Benefits
If you’re looking for a snack that’s rich in essential vitamins and minerals, may help in weight management, and offers health benefits to both your brain and heart, then consider adding a handful of mixed nuts to your daily diet.
Nuts and seeds are highly nutritious, low in carbs, and jam-packed with fiber, protein, antioxidants, essential vitamins and minerals, and an array of phytochemicals. Research suggests that eating nuts and seeds can lower the risk of certain conditions like high blood pressure, high cholesterol, and inflammation that can lead to heart disease, diabetes, cancer, and stroke.
Although nuts and seeds pack a wallop of nutrients and complement a well-balanced diet, they’re best eaten in moderation because of their high fat and caloric content. Fortunately, they’re high in unsaturated fats and omega-3 fatty acids, which are preferred heart-healthy substances. However, eating them in excess can be counterproductive.
Why Nuts and Seeds Deserve a Place in Your Diet
Nuts and seeds are considered superfoods, meaning a little can go a long way in providing health benefits. These superfoods:
- Won’t affect your lipids. Consuming them in moderation won’t increase your triglycerides or cholesterol. Research shows consumption does not affect your lipid panel, and can positively impact weight and blood pressure.
- Contain omega-3 fatty acids. Although we typically think of fish when we hear about omega-3 fatty acids, many nuts are also rich in this nutrient. These nutrients can help keep the heart, lungs, blood vessels, brain, and immune system functioning properly.
- Are packed with fiber. Fiber is necessary to regulate the immune system, fight inflammation, and help keep the bowel system regular. If you’re over the age of 50, the National Academy of Medicine recommends 21 grams of fiber per day for women and 30 grams per day for men. A handful of nuts provides nearly four grams of fiber.
- Contain Vitamin E and L-arginine. Nuts and seeds are a great source of Vitamin E, which deters the development of plaque in your arteries. L-arginine is a substance that can improve blood flow by making the artery walls more flexible and less prone to blockages.
- Are a protein source. Some nuts and seeds are higher in protein than others, which makes eating a variety a good idea. Protein helps your body maintain muscle, repair cells, and generate new ones. Protein should be about 15 to 25 percent of your daily calories. For older adults, that translates to 25 to 30 grams of protein per meal.
- Are antioxidant powerhouses. Antioxidants aid in reducing inflammation and oxidative stress. Walnuts, in particular, have been shown in studies to suppress oxidative stress by neutralizing free radicals.
- Contain phytosterols. This substance may help lower cholesterol.

How Often Should You Eat Nuts and Seeds?
The American Heart Association recommends eating about five servings of unsalted nuts a week, preferably raw or dry-roasted options. A serving is about a small handful of nuts and about a tablespoon of seeds.
Most nuts contain a host of beneficial nutrients. For good heart health, choose walnuts, almonds, macadamia nuts, hazelnuts, and pecans. Select walnuts and almonds for their antioxidant properties. To promote weight loss, opt for almonds. Pistachios may help reduce triglycerides plus fight inflammation. Brazil nuts are beneficial in fighting inflammation as well. So, when you eat an assortment, you cover all your bases.
Easy Ways to Add Nuts and Seeds to Your Diet
- Add pumpkin seeds to salads, oatmeal, rice, sweet potatoes, and quinoa for added flavor, fiber, and texture.
- Add nuts and seeds—like pine nuts, sunflower seeds, chia seeds, and pumpkin seeds—to smoothies. These choices are great for their protein, fiber, and omega-3 nutrients.
- Prepare your own trail mix with a blend of nuts and seeds and add the mix to yogurt or enjoy a handful as a snack.
The Bottom Line: Nutrition That Fuels Your Body and Brain
A well-balanced diet that includes eating nuts and seeds can deliver a host of heart- and brain-health benefits. The key to enjoying this nutritious, high-fiber superfood is in moderation.
At Aviv Clinics, we understand that optimal brain and body performance starts with the right fuel. As part of the Aviv Medical Program, many of our clients receive one-on-one dietary coaching tailored to support cognitive function, cardiovascular health, and overall well-being. Nutritional counseling is one of the many therapies we offer as part of the personalized Aviv Medical Program.
Whether you’re managing an existing condition or looking to elevate your brain performance through better nutrition, our team is here to help you make smart, sustainable choices.
Last Update: July 9, 2025
Seasonal Affective Disorder: How Winter Darkness Impacts Mood and Brain Health
Shorter days, cooler temperatures, and less sunlight can trigger mood and cognition changes in some people. Seasonal Affective Disorder (SAD) can impact brain health, but it is treatable.
What is Seasonal Affective Disorder?
SAD is a type of depression that emerges as seasons change. People who experience seasonal affective disorder can feel anxious, irritable, fatigued, sad, and have trouble sleeping, staying engaged, or thinking clearly. Some may even have thoughts of death and suicide, lose their appetites, and experience weight gain or loss.
Symptoms of winter-pattern SAD typically begin when the days get shorter in the fall and winter. Many describe it as winter blues. Symptoms typically subside with the onset of change of seasons.
Who is Most Affected by SAD?
Mental Health America estimates that about five percent of the U.S population suffers from seasonal depression, and four out of five people with SAD are women. However, many people may not even realize their depression is linked to seasonal changes, according to the National Institute of Mental Health. Not surprisingly, winter-pattern SAD is more common in people living farther north, where there are fewer sunny days and fewer hours of daylight in the winter.
Researchers are still studying the mechanisms of seasonal affective disorder. The National Institute of Mental Health notes that “SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.”
The condition can also be more common in people with major depressive disorder or bipolar disorder. Those with attention deficit hyperactivity disorder (ADHD), an anxiety disorder, or an eating disorder are also more prone to developing SAD. It can also impact more than one family member.
How Seasonal Changes Affect the Brain
Sunlight helps the body produce vitamin D, which is essential for maintaining serotonin, a neurotransmitter in the brain. Insufficient levels of serotonin can negatively affect mood and cognition because the brain is not firing properly. If these neurotransmitters are not firing, memory, learning, and concentration can all suffer
When the season shifts to fall and winter, and days become shorter, there is less sunlight available and less opportunity to produce vitamin D.
Shorter days also can interfere with the circadian rhythm or sleep-wake cycle, resulting in an overproduction of melatonin, a hormone critical for maintaining the body’s normal daily rhythm. Too much melatonin can cause sleepiness and reduce energy.
Lifestyle Factors That Can Worsen Symptoms
Shorter days and less sunlight not only rob the body of vitamin D, but also tend to spend more time indoors and potentially become less active. The lack of physical activity and social interaction because of being indoors can exacerbate SAD symptoms. Neither the brain nor the body has much energy, leading to increased fatigue and worsening symptoms.
Eating poorly can also intensify symptoms. Winter holidays like Thanksgiving are celebrated with hefty feasts that often include sugar-laden foods, lower-quality carbohydrates, and highly saturated fatty foods, which can create inflammation in the body. Studies have shown that sugary drinks, refined carbs, trans fats, processed foods, artificial sweeteners, and alcohol can increase inflammation and impact memory and learning.
Treating Seasonal Affective Disorder
SAD is mainly treated with light therapy. Other methods that may be used in conjunction with light therapy include talk therapy, vitamin D supplementation, and antidepressant medications.
- Light therapy. To make up for the loss of sunlight, a SAD sufferer can soak up intense light using a light box, which provides up to 20 times more light than ordinary indoor light without the damaging UV rays associated with natural sunlight. To reap the most benefit, the person should sit 30 to 45 minutes each morning in front of the box. Light therapy is not recommended for someone with bipolar disorder, however, because the intense illumination can lead to a manic episode.
- Talk therapy. Because some people associate winter with negative thoughts, psychotherapy may be beneficial to help restructure thinking. Talk therapy works well in conjunction with light therapy.
- Medications. For some people with SAD, antidepressants may be useful. Medications called selective serotonin reuptake inhibitors (SSRIs) are used to treat SAD when symptoms occur.
- Vitamin D supplements. A lack of sunlight will result in a vitamin D deficiency. A vitamin D deficiency causes fatigue, bone pain, muscle weakness, and mood changes like depression. Although sunlight is the best and preferred source for vitamin D, light therapy, food, and nutritional supplements are alternative sources.
Recognizing When to Seek Help for SAD
If symptoms of SAD interfere with quality of life, it’s time to talk to your doctor.
Can the symptoms of seasonal affective disorder be prevented? All of the symptoms may not be entirely preventable, but there are things you can do to reduce the severity of how you feel.
- Begin light therapy before the onset of symptoms.
- Take advantage of daylight hours to exercise outdoors.
- Be socially active even when you feel like you would rather stay indoors.
- Choose brain-beneficial foods that promote good mental health.
- Maintain your sleep routine and cycle.
How Aviv Clinics Can Support Brain and Mood Health
Understanding the root causes of mood and cognitive shifts is key to personalized treatment for seasonal affective disorder.
At Aviv Clinics, our multidisciplinary team includes clinical psychologists and neuropsychologists who assess and treat changes in cognitive functioning. By integrating mental health support with other evidence-based interventions in the Aviv Medical Program, we help clients better understand the factors contributing to their symptoms and offer proactive solutions.
Fuel Your Game: Nutrition Tips for Golfers to Stay Focused and Energized
You have invested in the most advanced golf equipment and the newest apparel, but have you considered that the food and beverages you consume are perhaps equally important to the game?
What you eat and drink before, during, and after you hit the links will determine how well you perform, as well as help you recover after your game.
Golf may not be a high-endurance sport, but it does require energy, focus, and keen hand-eye coordination, all amid an environment that can be taxing if temperatures soar. Your golf nutrition will help you sustain your energy, maintain concentration, and remain competitive so that you can play at your optimal level.
Before You Tee Off: What to Eat and When

Staying hydrated is key because dehydration can stop your progress quickly by causing muscle cramps and leaving you feeling extremely tired and out of focus. Of course, when you are unable to think clearly, your performance will suffer. Weigh yourself without clothing before your round so you’ll know how much water you’ll need to replenish after you finish (more on that later).
What to eat before golf is just as important as when to eat. If your tee time is early, eat your normal breakfast two to three hours before your round begins. Your body will need this fuel to make it through at least the first nine holes. Yogurt with mixed nuts and fruit is one example of a pre-game meal. High fiber cereal with low-fat milk and fruit is another example. You’ll want to enjoy your coffee, but also drink plenty of water as part of your golf nutrition plan before heading out to the course.
Fueling Your Round: What to Eat and Drink on the Course
As you progress around the fairways, remember to hydrate every 20 minutes. Avoid drinking alcohol or caffeinated beverages, which can lead to dehydration and impair your ability to drive, swing, and chip effectively on the golf course.
If the heat index is high and you plan to spend more than 60 minutes outside, you will need to replenish your electrolytes. Drinking sports drinks, such as Gatorade or Powerade, diluted with water will help restore these essential nutrients. Ideal snacks during your game include fruit, nuts, and pretzels.
Post-Round Recovery: How to Rehydrate and Refuel
As soon as you return home, weigh yourself again without clothing. For every pound of weight lost, drink 16 ounces of water to replenish yourself throughout the evening. Although you might want to celebrate (or drown your sorrows) after your round with beer or a cocktail, these beverages can further aggravate your dehydration.
The Bottom Line: Nutrition and Performance go Hand-in-Hand
If you love the game of golf and want to perform at your optimum level, invest well in your game by making smart choices in your equipment and good golf nutrition. To take your golf game to even greater heights, the Aviv Medical Program can help you regain your stamina and optimize your brain and body performance.
Watch how PGA Tour golfer and Ryder Cup winner Tommy Fleetwood elevated his golf game through the Aviv Medical Program.
Aviv Clinics’ groundbreaking treatment enhances cognitive and physical function and triggers the body’s natural capability for self-regeneration. The program can include a unique hyperbaric oxygen therapy protocol, alongside other doctor-prescribed interventions, including cognitive exercises, physical training, and nutrition coaching to tailor a personalized program to your individual needs.
Want to learn more about how Aviv Clinics in central Florida can elevate your skills? Click the button below to schedule a free consultation with one of our board-certified physicians.
Understanding Alzheimer’s Risk: Causes, Prevention, and the Promise of Hyperbaric Oxygen
We all experience occasional memory lapses, especially as we age. For most of us, these minor cognitive issues are usually just annoyances. But if your cognitive issues interfere with your daily life, they could be the beginning of something much more serious.
Read on to learn more about the risk factors for Alzheimer’s disease and how you can preserve your cognitive health.
What Is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia that impacts a person’s ability to think, reason, and remember. As it progresses, Alzheimer’s can severely affect quality of life, eventually becoming completely debilitating.
The most common type of Alzheimer’s disease is the late-onset form, when symptoms usually “become apparent in [a person’s] mid-60s or later.”
10 Early Signs and Symptoms of Alzheimer’s Disease:

According to the Alzheimer’s Association, ten early warning signs of late-onset Alzheimer’s disease include:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks
- Confusion with time or place
- Trouble understanding visual images and spatial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgment
- Withdrawal from work or social activities
- Changes in mood and personality
If you experience a cognitive problem that impacts your daily life, don’t ignore it. Dementia is not a normal part of the aging process. The sooner you seek help, the sooner you can take action against cognitive decline.
Get in touch with our care team>>
What Are the Risk Factors for Alzheimer’s Disease?
Science is still learning how Alzheimer’s disease develops and why some people are at greater risk of developing it than others. It’s an active area of study, and researchers are making new discoveries every day.
The consensus among scientists is that a combination of age, sex, genetic, environmental, and lifestyle factors all contribute to the development of Alzheimer’s disease.
Let’s take a closer look at some of the greatest risk factors for Alzheimer’s:
- Although old age does not directly cause Alzheimer’s disease, the risk of developing Alzheimer’s “doubles about every 5 years” after age 65.
- More women than men develop Alzheimer’s disease, although this may be because women live longer than men on average.
- Suffering from a traumatic brain injury (TBI) can increase the long-term risk of developing Alzheimer’s or another type of dementia.
- Acute and chronic inflammation are both associated with an increase in cognitive decline. Eating a diet full of inflammatory foods like processed sugar may exacerbate the risk of developing inflammation in the brain.
- Exposure to environmental pollutants has been linked to an increased risk of dementia. Some researchers believe that nearly half of the individual differences in Alzheimer’s risk may be because of environmental factors.
- Being a smoker carries a significantly increased risk of developing Alzheimer’s disease. This risk factor offers another compelling reason to quit.
- People with Down syndrome also have a greater risk of developing Alzheimer’s disease. About 30% of people with Down syndrome develop Alzheimer’s disease by their 50s. The risk reaches closer to 50% in their 60s.
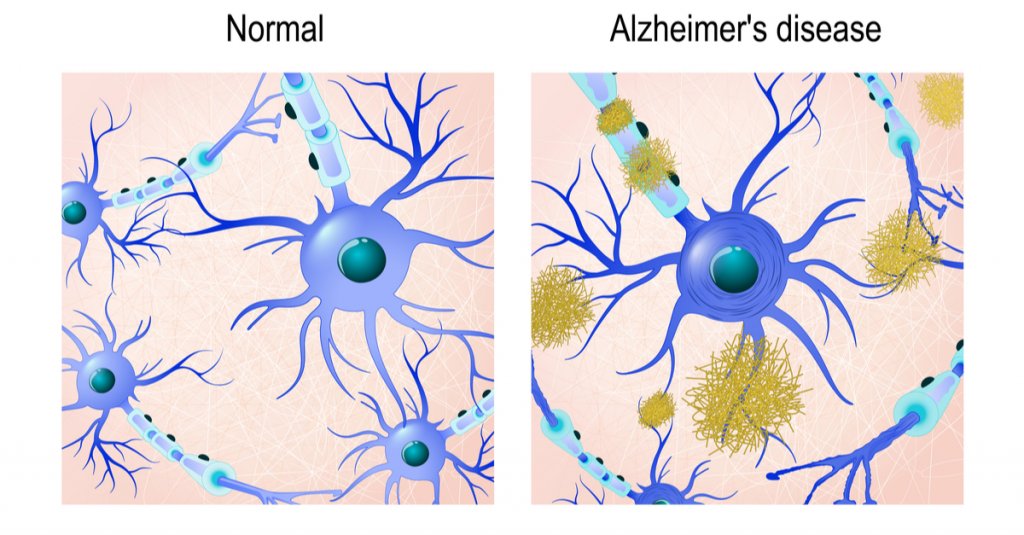
The Role of Brain Proteins in Alzheimer’s: Amyloid Plaques and Tau Tangles
Scientists typically focus on two different protein structures in the brain associated with Alzheimer’s disease: Neurofibrillary tangles and amyloid plaques.
It’s not currently known whether the presence of these structures causes Alzheimer’s disease or if they’re simply byproducts of it. But both can impair cognitive function and can worsen as the disease progresses.
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a simple blood test available at Aviv Clinics may be able to answer this question: pTau Testing
Neurofibrillary Tangles
Neurofibrillary tangles are accumulations of a harmful protein called tau in the brain’s neurons. These tangles can inhibit the neurons’ ability to communicate, causing cognitive decline. Some studies reveal that a lack of oxygen to the brain is associated with neurofibrillary tangles.
Amyloid Plaques
Amyloid plaques are hard, insoluble clumps of beta-amyloid proteins that build up between neurons. Like neurofibrillary tangles, these plaques are toxic to brain cells and disrupt cell-to-cell communication. They can eventually result in cellular death, harming cognitive abilities even further.
Brain scans can reveal the presence of both protein structures, so your doctor can alert you to the presence of Alzheimer’s disease or if you’re at risk for developing it.
Is Alzheimer’s Disease Genetic?
Both early-onset and late-onset Alzheimer’s disease have a genetic component, meaning if you have a family history of Alzheimer’s, you carry a greater risk for developing the disease. The risk factor is greater if an immediate family member suffers from the disease, such as a parent or sibling.
Genetics are almost always the primary contributing factor of early-onset Alzheimer’s disease, which can affect people as young as their 30s or 40s.
Gene Mutations
Researchers have yet to identify any specific genes directly responsible for the development of late-onset Alzheimer’s. However, certain mutations of the APOE gene, which are found on chromosome 19, are currently considered the strongest genetic risk factor for Alzheimer’s disease.
For example, the specific gene mutation APOE ε4 is linked to higher levels of amyloid plaques and is often found in people with Alzheimer’s disease.
Your doctor may order genetic testing if you have a family history of cognitive problems or early-onset dementia.
Remember, this doesn’t mean you’re destined to develop Alzheimer’s if a parent or sibling has had it. Some people who possess the APOE ε4 gene never develop Alzheimer’s disease, and some people with Alzheimer’s don’t have any gene mutations at all.
Genetics is just one of many Alzheimer’s risk factors. We still need more research to develop a complete picture of what the largest risk factor for Alzheimer’s disease is.
Can Hyperbaric Oxygen Therapy Help Prevent Alzheimer’s Disease?

A specific hyperbaric oxygen therapy (HBOT) protocol shows promise as a potential preventative measure for Alzheimer’s disease. HBOT is a treatment that involves breathing 100% oxygen in a pressurized chamber to increase oxygen levels in the body and brain. A unique HBOT protocol used at Aviv Clinics has shown several benefits in individuals at risk for or experiencing early cognitive decline:
Benefits of HBOT for Alzheimer’s Disease:
- Improves brain tissue oxygenation
- Lowers neuroinflammation (inflammation in the brain)
- Shrinks beta-amyloid plaques (in laboratory animals)
- Reduces pTau protein levels (in laboratory animals)
- Improves memory recall and cognitive performance
- May slow or reverse early signs of cognitive decline
These benefits have been documented in peer-reviewed studies. This specialized HBOT protocol is available exclusively at Aviv Clinics in Central Florida.
In one study, repeated HBOT sessions showed reduced brain hypoxia, reduced amyloid plaques and pTau, and improvements in cognitive performance. Another study found improvements in memory recall in people with mild cognitive impairment (MCI), a potential early stage of Alzheimer’s. Researchers concluded that HBOT “should be considered as a therapeutic approach to slow the progression or even improve the pathophysiology responsible for [Alzheimer’s] disease.”
Lifestyle Habits That May Lower Your Alzheimer’s Risk
While none of us can change our genetic makeup, we can change our lifestyle. Healthy habits can help lower your risk factor for nearly any disease, not just cognitive conditions. Lowering inflammation levels in your body can also help lower inflammation in the brain. To help preserve your cognitive health:
- Eating a healthy diet full of fruits and vegetables
- Exercising regularly
- Maintaining healthy blood pressure
- Keeping your mind active
- Maintaining a healthy weight
- Practicing mindfulness and meditation
- Avoiding excess alcohol
- Avoiding smoking
- Getting plenty of restful sleep
- Taking care of your mental health
How the Aviv Medical Program Can Support Brain Health
The Aviv Medical Program is a personalized intervention designed to improve brain and body health. Using the unique HBOT protocol discussed earlier, alongside other evidence-based interventions, this program can treat both physical and cognitive performance in older adults. In clinical trials, this protocol has also reversed key biomarkers of the aging process.
Depending on your symptoms, needs, and goals, our clinical team will perform an assessment that may include:
- In-depth medical history review
- Comprehensive physical and neurological exam
- Physical therapy evaluation
- Highly advanced brain imaging scans
- Neurocognitive tests
Once our board-certified physicians review your results, they’ll prescribe a customized treatment program designed to treat your concerns. This program may include:
- A specialized hyperbaric oxygen therapy protocol
- Physical training
- Dietary coaching
- Cognitive exercises
- Other interventions as prescribed
Real Client Results: Carl and Vickie’s Cognitive Improvements
Married couple Carl and Vickie both had parents with dementia and cognitive decline. They soon realized they were beginning to experience the same cognitive issues that they saw in their parents.
The couple’s quality of life was not where it should have been, so they took action with the Aviv Medical Program. They use one word to describe their improvements in cognitive performance: “remarkable.”
I’m dancing, I’m hiking, I’m running again. It’s just remarkable. I don’t know how else to say it.” –Vickie Eckert, Aviv Medical Program Alumna
Take Control of Your Brain Health With Aviv Clinics
While science is still investigating all of the risk factors for Alzheimer’s disease, anyone can lower their likelihood by taking charge of their lifestyle.
Preserving your cognitive health starts with the choices you make every day. Partnering with Aviv Clinics is just one of them. Contact our medical team to learn how we can help you.
Last Update: July 8, 2025
How Anxiety Affects Brain Health: Long Term Impact and 7 Natural Ways to Cope
Worry and everyday stressors are common triggers for anxiety, a condition that ignites areas of the brain responsible for detecting and responding to real-life threats. Anxiety affects brain health because it produces the “fight-or-flight” response, which can “make the heart pound and breathing quicken.”
Anxiety disorders are the most common mental health concern in the U.S., affecting 40 million adults. Those who live with anxiety are all too familiar with the cascade of physical symptoms, from a racing heart to sweating to hyperventilating.
What you may not realize, however, is that all those episodes of anxiety may be harmful to the brain, especially if the anxiety goes untreated for a long period.

What Is Anxiety and How Does it Affect the Brain?
Anxiety is a feeling of worry, dread, or nervousness. It is an emotional and physiological response to an impending event or an uncontrollable situation. In severe cases, this state of apprehension can lead to compulsive behaviors or panic attacks.
It’s perfectly normal to experience some degree of anxiety in certain situations, like having to give a speech in front of an audience or taking a test.
When anxiety becomes chronic and excessive, or interferes with your quality of life, that’s when the brain begins to experience its negative effects.
Common Causes of Anxiety and Brain Dysfunction
Several variables can lead to chronic anxiety:
- Genetics
- Brain dysfunction or injury
- Post-traumatic stress syndrome
- Environmental stressors like abuse and neglect
- Substance abuse
- Medical conditions like thyroid disease
- Repetitive negative thinking
How Anxiety Affects Brain Health (and the Fight or Flight Response)
When a person experiences anxiety, the brain’s amygdala, hippocampus, and prefrontal cortex (PFC) become hyperactive.
These parts of the brain are responsible for sensing danger, whether that danger is real or imagined. They trigger a surge of adrenaline and cortisol (the stress hormone) throughout the body in response to that perceived danger. This activates the fight-or-flight response.
The reaction serves the body well in a truly life-threatening situation because the adrenaline and cortisol allow the body to react quickly with heightened awareness. In these cases, the brain is doing exactly what it’s designed to do to protect the body.
However, your brain’s well-equipped, danger-interpreting processes may be impaired by unhealthy reasoning and inappropriate thought responses. How your brain interprets the perceived threat will dictate how well you can quell the fight-or-flight response and return to a state of calm.
Excessive and prolonged anxiety affects brain health by producing an overabundance of stress hormones. This can ultimately lead to panic attacks, a more severe side of anxiety.
An overly anxious brain becomes much like the boy who cried wolf: always on high alert for incoming danger, despite many false alarms. In this heightened state, the brain has a harder time reasoning rationally and is less able to interpret real-life danger.
What Research Says about Anxiety and Brain Health
Studies illustrate that stress reduces hippocampal volume. The hippocampus processes long-term and contextual memory, so persistent anxiety can impact the brain’s ability to store and access our memories.
Stanford University biological sciences professor Robert Sapolsky noted that research “shows links between long-term stressful life experiences, long-term exposure to hormones produced during stress, and shrinking of the part of the brain involved in some types of memory and learning.”
That makes treating anxiety early ever more critical as you move closer to your golden years, especially because stress can have other negative impacts on the brain.
7 Natural Ways to Reduce Anxiety and Protect Brain Health
The first step in overcoming anxiety is recognizing that there is a problem. If you notice any of these signs, it’s time to seek help:
- Your anxiety is limiting your ability to enjoy life.
- You’re consistently unable to sleep.
- You feel irritable.
- You notice changes in your appetite.
- You’re experiencing physical and mental changes.
Medications are available to help cope with anxiety. However, cognitive therapy can assist in restructuring reasoning and ultimately relieve chronic anxiety. The goal of cognitive therapy is to replace the negative self-talk during an anxiety-driven episode with more realistic and reasonable thought processing. This ultimately works to de-escalate the fight-or-flight response.
Stress or anxiety occurs when our pressures exceed our resources. Here are seven healthy coping strategies to incorporate into your daily life for managing stress and the effects of anxiety on brain health:
1. Use Self-Care to Calm an Anxious Brain
Listen to music, meditate, get a massage, or practice yoga. Wellness apps such as Headspace offer meditation and yoga guides, as well as relaxing music to help you wind down.
Look into local massage therapy services, such as kneading or face/neck rubbing, to reduce tension in your body.
2. Eat a Brain-Healthy Diet to Ease Anxiety
Choose healthy options and avoid overeating. Consider following the MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet.
MIND is a blend of two diets:
- Mediterranean: A heart-healthy eating plan
- DASH: Addresses hypertension or high blood pressure
This evidence-based diet encourages you to consume a variety of fruits, vegetables, and healthy fats and proteins, and is linked to better cognitive function, memory, and increased brain volume.
3. Cut Back on Alcohol and Caffeine to Manage Anxiety
Despite some feelings of stimulation, alcohol depresses the central nervous system and can worsen symptoms of anxiety. So can caffeine, which is a stimulant. Instead, drink more water. Although conventional wisdom tells us that most people should drink about four to six cups of water each day, the total amount we should consume varies. For example, if you’re exercising or sweating heavily, you may need at least two to three cups of water per hour.
Non-caffeinated teas, such as chamomile tea, are well known for their relaxing properties, and you can enjoy them any time of the day.
4. Improve Sleep to Reduce Chronic Anxiety Symptoms
Stress can disrupt sleep. Create a healthy environment conducive to a good night’s sleep. Experts recommend that healthy adults get an average of 7 to 9 hours of sleep per night.
Here are some tips:
- Shut down all electronics an hour before bedtime. Too much screen time in the evening can disrupt the surge of melatonin we need to fall asleep.
- Read a good book or take a warm bath. These activities help your mind and body wind down.
- Keep a consistent sleep schedule. This will encourage your circadian rhythm to stabilize.
- Keep a cool temperature in your room. Our body temperature naturally drops in the evening, so a cooler room can help reinforce your body’s natural instinct for slumber.
5. Boost Brain Health with Regular Exercise
Shoot for at least 30 minutes of moderate exercise at least three days a week. To help motivate yourself to exercise consistently:
- Find a type of movement you love. Whether gardening, dancing, playing pickleball, or golfing, stick to an activity that makes you feel good.
- Start small and work your way up. Don’t start with high-intensity exercises. You don’t want to get burned out or suffer an injury. Instead, start with light activities like a brisk walk, and as you become more comfortable and confident, gradually build the intensity.
6. Reduce Anxiety Through Social and Spiritual Support
Lean on trusted friends, family members, or faith leaders for support. They can offer a listening ear, honest advice, or an activity to get your mind off stressors. Simply talking with someone can often ease anxiety.
7. Seek Professional Help for Chronic Anxiety
If you’re feeling overwhelmed by anxiety, talk to your family doctor or seek help from a therapist. Speaking to a professional can help you process your feelings and suggest personalized ways to cope.
Each person is different, so seeking a customized approach from a therapist or doctor can make a big difference, especially if you haven’t seen any improvements from the strategies listed above.
Final Thoughts: Controlling Anxiety to Protect Long-Term Brain Health
Anxiety affects brain health, but it is both treatable and controllable. There are healthful ways to cope with anxiety, so you can protect your brain from its potential detrimental effects. With practice, you can learn how to take a deep breath, assess a situation appropriately, and avoid an impending wave of anxiety.
For more help on enhancing your physical and cognitive performance, contact Aviv Clinics in The VillagesⓇ.
Last Update: July 8, 2025
The Health Benefits of Playing Golf: 10 Reasons Why You Should Play
Last Updated July 8, 2025
Golf is challenging yet also can be exhilarating. The game rewards regular players with more than just some fresh air and the elusive hole-in-one. Playing golf also benefits your cognitive and physical health. Here are 10 benefits of playing golf, in particular for older adults:
1. Golf Improves and Extends Longevity
Golfers, on average, live five years longer than their non-golfing counterparts. One long-term study revealed that golfers experienced a 15.1% lower death rate compared to non-golfers (at 24.6%).
More than just “living longer,” golf improves your healthspan, or the number of years you feel healthy, stay active, and enjoy the vitality of both your mind and body.
2. Golf Enhances Brain Health
Playing golf can have positive benefits for the brain, as well as the body. A National Institutes of Health study found that golf enhances focus and attention in individuals who experience “subjective memory complaints.”
Exercise itself can produce numberous brain health benefits, including:
- Increased blood flow to the brain
- Sharpened focus
- Increased stimulation of the cerebellum, one of the areas of the brain responsible for coordination
3. Playing Golf Promotes Healthier Sleep
A good night’s rest is one of the key factors to physical and mental health and well-being. During deep sleep, the body and brain perform restorative and repairing processes, which can help you function at an optimal level in your waking hours.
After a day on the links, your body is ready for a well-deserved rest, and science supports this. Research shows moderate aerobic exercise increases the amount of deep sleep a person gets. Exercise also helps stabilize your mood and decompress the mind, a process important for naturally transitioning into sleep.
4. Playing Golf Fosters Socialization
Socialization is another benefit of playing golf, as participating in a group activity can also help your health. Socializing has been proven to:
- Stave off loneliness and depression
- Sharpen memory and cognitive capacity
- Increase feelings of happiness and well-being
- Help you live longer
Socializing triggers the nervous system to release certain neurotransmitters that regulate the body’s response to stress and anxiety. Social connections also release dopamine, the “feel-good” hormone.
5. Golf Reduces Stress
It might be hard to believe, because golf can be such a frustrating activity, but a prime mental health benefit of golf is that it helps reduce stress.
A round of golf can help reduce cortisol (the “stress hormone”) and spur the release of endorphins—the chemicals that help to relieve stress and boost happiness. Spending time outdoors in nature can help you feel calmer and more clear-headed. Plus, engaging in a fun activity is always a great stress reducer.

6. Golf Offers a Low-Impact Physical Activity and Burns Calories
Despite what many may think, golf is an excellent workout! The average 18-hole game burns between 800-2,000 calories (amounts vary depending on whether you walk or ride in a cart). Burning those extra calories will help keep you at a healthy weight. Less extra baggage leads to even more health advantages, such as reducing the risk of certain cancers, heart disease, stroke, diabetes, infertility, arthritis, sleep apnea, and more.
But because golf is a low-impact sport, you’ll be less likely to be injured while playing. Golf is also easier on your joints than many other sports.
7. The Entire Family Can Enjoy a Round of Golf
Why not bring along your kids or grandkids on your next golf outing? Golf is a family-friendly activity that people of all ages and fitness levels can enjoy.
Golf coaches say five is a great age to teach kids to golf, but kids as young as two can learn the basics. That’s the beauty of a sport like golf. You’re never too young (or old) to learn.
8. Golf Gets You Outside in the Fresh Air
The long-term impact of COVID-19 made some of us more accustomed to staying indoors. Golf is a healthy reason to get out of the house and stay active in the fresh air.
Playing golf means spending time outdoors, and time outside can help:
- Fight seasonal depression
- Boost creativity
- Improve concentration levels
Being outside also produces additional positive effects. For example, fresh air increases the flow of oxygen in the body, leading to other benefits like healthy digestion and improved cell function.
9. Time Outdoors Increases Vitamin D Exposure
Vitamin D is one of the essential vitamins in the human body. It’s most known for promoting healthy bones, but this crucial vitamin also supports immune health, muscle function, and brain cell activity.
Sun exposure is one of the benefits of playing golf and a natural way to get the vitamin D your body needs for peak performance. Just be sure to wear sunscreen.
10. You Can Practice Golf Anywhere
If you’re looking to improve your game, you can easily practice your swing at home with a mat and net or launch monitor in your backyard.
You can also practice your grip and posture in front of a mirror and do swing drills from the privacy of your own home. Practicing putting is even easier: All you need is a club, a ball, and a carpeted floor.
Discover Even More Health Benefits with the Aviv Medical Program
The Aviv Medical Program can help you take your golf game to the next level by helping you regain your stamina and optimize your brain and body performance.
This innovative, science-backed treatment can include a unique hyperbaric oxygen therapy protocol, plus cognitive and physical training, nutrition coaching, and the industry’s most comprehensive assessments to tailor a personalized program to your individual needs.
Watch how PGA Tour golfer and Ryder Cup winner Tommy Fleetwood elevated his golf game through the Aviv Medical Program.
Contact us to learn more about how to improve your brain health and elevate your physical performance with the Aviv Medical Program.
Menopause Brain Fog vs. Dementia: Understanding Hormonal Impact on Memory Loss
We all know that menopause changes your body. But did you know that menopause can also affect brain health? Hormone changes caused by menopause can cause cognitive issues like memory loss, learning problems, and trouble concentrating. These changes may be so gradual that you might not notice them at first, or so insignificant that you don’t pay them much attention. But is the brain fog you’ve been experiencing caused by menopause, or something more serious? Let’s discuss menopause and brain health.
How Menopause Hormones Trigger Cognitive Decline & Memory Lapses
Menopause is the gradual shutdown of the female reproductive system. In the United States, the average starting age for menopause is 52. However, perimenopause (the symptomatic period) can occur much earlier, lasting anywhere from two to eight years.
Perimenopause brings a whole host of symptoms with it, including hot flashes, sleep problems, menstrual changes, and notably, cognitive difficulties. More than two-thirds of menopausal women report experiencing problems with memory, concentration, and executive function. For a long time, we only had anecdotal evidence of the cognitive difficulties that menopausal women face. But recent studies have revealed scientific evidence that “menopause brain fog” can be clinically detected.
If you’ve been having trouble concentrating on your favorite book or struggling to remember words since beginning your menopause transition, it’s not just in your head. The fluctuating hormone levels in your brain could be the cause of your minor memory loss. There’s still a lot we don’t understand about why menopause impacts the brain. But one of the key factors is thought to be the declining levels of the hormone estrogen, which plays a crucial role in the brain.
Estrogen isn’t only produced in the ovaries. The hypothalamus gland in your brain also manufactures precursor signal hormones that ultimately end up making estrogen elsewhere in your body. Estrogen is active in the prefrontal cortex and hippocampus, which are important to maintaining memory and executive function.
Having proper levels of estrogen in the brain is also vital to proper aging because estrogen imbalances are thought to play a role in the development of Alzheimer’s disease. More research on the physiological differences between male and female brains is needed to understand whether this is one of the reasons why women may be more susceptible to dementia than men.
Menopause Brain Fog vs. Dementia: Key Differences You Should Know

Fortunately, menopause-related brain fog is often mild and can disappear on its own with time, just like other unpleasant aspects of menopause, such as hot flashes. For many women, this is a huge relief. It can be incredibly cathartic to know that there’s a reason behind why you keep misplacing your phone or struggle to concentrate on your favorite book. But how do you know if your cognitive problems are actually caused by menopause?
The symptoms of menopause-related brain fog and other age-related cognitive disorders often overlap. You might have been dismissing your brief lapses in memory as just another quirk of menopause, when in reality, they could be the start of early-onset dementia or Alzheimer’s disease. Just because menopause and brain health are interrelated, this doesn’t mean that your memory lapses are menopause-related.
But how do you tell the difference?
What’s the Difference Between Menopause Brain Fog and Early Dementia?
Menopause-related brain fog often includes mild, temporary issues such as forgetfulness, difficulty concentrating, or struggling to find the right word. These symptoms usually improve over time as hormone levels stabilize.
In comparison, early signs of dementia may involve more serious or progressive concerns, such as:
-
- Repeating the same questions frequently
- Getting lost in familiar places
- Struggling with simple tasks or directions
- Forgetting common words or names
- Difficulty making decisions
- Noticeable changes in personality or behavior
If cognitive symptoms interfere with your daily life or worsen over time, it’s important to consult your physician for a full evaluation.
Women are nearly twice as likely to develop dementia as men, so it’s vital to stay vigilant for the warning signs of dementia early on. When in doubt, it’s always best to raise your concerns with your doctor rather than dismiss them as nothing. However, even if you don’t have dementia or Alzheimer’s disease, there are times when menopause-related cognitive decline can linger rather than naturally fade.
Estrogen, Menopause and Brain Health: Scientific Connections
In a study published in the Journal of the Menopause Society, researchers discovered that the advancement of menopause was a “key determinant of cognition” among both pre- and post-menopausal women. The women included in the study were primarily low-income women of color, some of whom also had HIV. The study followed the women for several years, from pre-menopause through post-menopause. Every two years, the women underwent testing to assess their cognitive abilities, including memory, verbal learning, attention span, processing speed, motor skills, executive function, and more.
Even after adjusting for age and other factors, the overall odds for a decline in cognitive function still increased throughout menopause. Many of those in the test group had even reached a “clinically significant level of cognitive impairment” by the end of the study. Although HIV might have had a role to play in the severity of the decline, cognitive problems also persisted in women who didn’t have HIV.
Science still hasn’t determined exactly why menopause-related cognitive problems naturally fade in some women and linger in others. Fortunately, there are ways to help yourself through these cognitive issues.
Effective Lifestyle Strategies to Alleviate Menopause-Related Brain Fog
In general, living a healthy lifestyle can help you balance your hormones during menopause and alleviate cognitive symptoms. This includes a healthy diet, exercise, and keeping your mind active.

Nutrition. Eat foods that promote brain health, such as whole fruits, vegetables, lean meat, and nuts.
- Fish are full of omega-3s, which can boost brain power.
- Leafy greens such as kale, spinach, and collards are rich in brain-healthy nutrients like folate and vitamin E.
- Take care to avoid eating sugar and processed foods, which can not only increase brain fog but also worsen other menopausal symptoms, like hot flashes and sleep disruptions.
- Eating dairy products rich in calcium can also help offset your risk of developing osteoporosis, which increases during menopause.
Exercise. Regular exercise increases blood flow to the brain, and an oxygenated brain is a healthy brain. Even a brisk walk down the block with your partner or pet can help you lift your mental fog. Exercise can also help ward off menopause-related weight gain, if you’re concerned about that.
Meditation. Of course, you can also exercise your brain directly. Mindfulness activities like meditation can increase your focus and help you concentrate on your important tasks more easily. You can even combine mindfulness with physical activities like yoga to get the best of both worlds!
The Bottom Line: Supportive Solutions for Menopause-Related Cognitive Decline
While menopause can leave you feeling foggy or out of sorts, you can take steps to alleviate your symptoms by living a healthy lifestyle. Keep an eye out for any cognitive problems that negatively impact your life, and contact your doctor if you feel that something is out of place. Whether you or someone you love is going through this transitional period in life, remember to always be kind, patient, and understanding.
Restore Cognitive Clarity with the Aviv Medical Program
At Aviv Clinics, we understand the frustration that comes with cognitive changes. The personalized Aviv Medical Program addresses cognitive decline at its source — whether it stems from aging, illness, or other health factors. Using a unique, evidence-based hyperbaric oxygen therapy (HBOT) protocol, advanced brain imaging, and complementary therapies like nutritional counseling, physical activity, and cognitive exercises, we help clients restore clarity, memory, and focus.
If you’re concerned that menopause — or another cause — is affecting your brain health more than it should, we’re here to help you get to the root of the issue and create a plan for optimal long-term brain performance.
To learn more about the personalized health program available at Aviv Clinics and discover how we can help, contact the clinic.
Last Update: July 7, 2025
Technology and Brain Health: How Screen Time Affects Focus, Memory, and Mental Clarity
Technology is advancing at a shockingly rapid pace. Screens are now a staple of our daily lives — we interact with them everywhere: at home, in the office, and in our pockets. We use them to communicate, conduct business, shop, entertain ourselves, and more.
Between booming technology, the ever-increasing pace of life in general, and rising rates of ADHD diagnoses, many people may wonder if our attention spans are diminishing. Could technology be negatively affecting our brain health?
To some extent, we aren’t sure yet how technology affects us, cognitively or socially.
Experts have warned against the maladies of screens ever since the television became a staple of the American living room almost 70 years ago. Passive television watching, however, may not compare to the technological onslaught of modern culture.
In a world where everyone has a supercomputer in their pocket that provides access to the entirety of accumulated human knowledge via the internet, what’s happening to our brains?
Here is what we know so far about technology and brain health, as well as strategies for adapting to this new normal.
Is Technology Causing ADHD Symptoms in Adults?
If it seems like everybody you know has ADHD (attention deficit hyperactivity disorder) lately, you might not be imagining it. From 2007 to 2016, rates of adult ADHD diagnoses doubled. Although most studies on screen time involve children, the correlation between screens and poor attention in adults is nonetheless present.
It should be noted that these studies are not necessarily saying that people who use screens often will “develop” ADHD. ADHD is a neurological condition that a person is born with and that often persists through childhood into adulthood. It represents a different “wiring pattern” in the brain.
However, these studies demonstrate that screen time and media use are highly correlated with symptoms of ADHD. In other words, while the underlying mechanism might be different from true ADHD, too much screen time leads to something that looks a lot like ADHD.

The main symptoms of ADHD are:
- Short attention span, especially for non-preferred tasks
- Hyperactivity, which may be physical, verbal, and/or emotional, can also manifest as fidgeting or restlessness
- Impulsivity
- Disorganization and difficulty prioritizing tasks
- Poor time management and time blindness
- Frequent mood swings and emotional dysregulation
- Forgetfulness and poor working memory
- Trouble multitasking and executive dysfunction
- Inability to control anger or frustration
- Trouble completing tasks and frequent procrastination
- Distractibility
- Difficulty awaiting turn
(If you have several of these symptoms, it’s worth discussing them with your doctor.)
Part of the rise in diagnoses could be due to increased awareness and education. Some adults may realize they have always struggled with these symptoms. For an ADHD diagnosis, symptoms must have been present in childhood, even if they were initially missed.
As an adult, if you “suddenly” develop ADHD-like symptoms that weren’t there before, there may be many reasons for these new cognitive or attentional issues.
Cognitive Decline vs. Screen Overload: What’s Really to Blame?
If you think your attention is suffering, ditching screens may or may not be the ideal solution. When it comes to impaired cognitive function, there are other causes that also should be considered.
Normal aging will cause some minor changes in cognition, including slowed processing speed, taking longer to learn new information, and an increase in distractibility, for example. But normal aging shouldn’t impair daily functioning.
Forgetting a name on occasion isn’t a cause for concern, but repeatedly forgetting the same information, on the other hand, could be a symptom of mild cognitive impairment (MCI). Although MCI rates increase with age, cognitive impairment isn’t inevitable for everybody of advancing age.
Other factors can contribute to MCI, including:
- Depression, stress, and anxiety
- Thyroid, kidney, or liver problems
- Sleep apnea and other sleep disorders
- Diseases or conditions that affect blood flow in the brain
- Low vitamin B12 levels or other nutrient levels
- Eye or hearing problems
- An infection
- History of alcoholism
Stress can also contribute to deficits in cognitive abilities, such as short-term memory loss and brain fog. Self-care, including looking after your physical, mental, emotional, intellectual, and social health, is critical for brain health.
Is Technology Making Our Brains Lazy?

Some might argue that the tools of technology have become our crutches. For example, most of us no longer bother to remember phone numbers. A smartphone can remember vastly more information than our brain could ever hope to remember.
There are many challenges to studying the effects of technology and brain health, whether on the biology of the brain or the impact on society, that make this question difficult to answer. Experts are divided, with some seeing technology as a boon to society and others taking a more cynical view.
The one thing both sides agree on is technology’s ability to exploit the inherent human tendency towards laziness and the “quick fix.” As evolutionary geneticist David Krakauer said, “I’m most concerned about the unthinking acceptance of convenient short-term solutions.”
The human brain, in an attempt to be energy-efficient, often chooses the thing that benefits us immediately, foregoing potentially greater future benefits.
Persuasive Technology: How Social Media Hijacks Your Attention
Social media platforms, such as Facebook, Instagram, and Twitter, drive the progress of technology, particularly artificial intelligence (AI), in a way that targets our subconscious minds. After analyzing billions of data points collected each time you swipe, click, or tap online, social media platforms and other websites know you better than you know yourself.
Tristan Harris, president and co-founder of the Center for Humane Technology, calls this “persuasive technology,” or “technology that shapes attitudes and behavior.” By exploiting natural human psychological vulnerabilities, the website explains, “it begins to train us: our thoughts, feelings, motivations, and attention start to replicate what the technology is designed to produce.” This all happens beneath our level of conscious awareness, and yet it’s guiding our behavior; this presents, they argue, a very real threat to personal autonomy.
As these platforms learn your habits, they know exactly what to show you next to keep you scrolling. Thought you were going to breeze through social media in 15 minutes, and 2 hours later, you’re still there? That’s because your 50,000-year-old brain is trying to compete with the most complex supercomputers ever made.
How to Take Control: 3 Strategies to Improve Brain Health
How do you know if you need a break from screens?
Awareness is key for any form of self-improvement. If you look at your screen habits and find that you’re missing out on too much of your life and relationships in favor of screen time, here are three ways to reduce or counter the effects:
1. Spend More Time in Nature to Support Brain Function
Technology has many merits, but one way in which it causes collateral damage is that we tend to stay indoors to use it.
The average person spends up to 93% of their time indoors or in an enclosed vehicle. For a species that has spent most of its history as homeless nomads who knew only nature, transitioning to an indoor concrete jungle is not without consequences for our health. Getting out into nature can have a profound effect on our physical, mental, and emotional health.
Richard Louv, a journalist and author who coined the term “Nature Deficit Disorder”, summarized the research on the effects of nature: “Nature is not only nice to have, but it’s a have-to-have for physical health and cognitive functioning.”
According to a 2019 study, two hours or more per week of nature exposure is enough to significantly improve reported well-being.
2. Try a Digital Detox to Reduce Screen Time and Improve Focus
While we may not understand the mechanisms involved with the brain and media use, we do know one thing: the brain performs its best when exposed to variety and balance. While some amount of educational media or video games can improve cognition, too much of anything can be a bad thing. The brain needs many different kinds of stimulation, or lack thereof, in order to run at its best.
There are lots of tricks and methods for cutting back on screen time, from charging your phone outside of the bedroom to full-on silent meditation retreats. Turning off push notifications for apps that profit from your attention (like social media) is another way to cut down on the number of dopamine hits you get from your phone.
Why target these apps in particular? Because each notification, despite typically being of relatively little importance, registers in our nervous system as a minor threat or alert. Turning off notifications can reduce the number of “pings” on your nervous system.
3. Focus on Quality Screen Time, Not Just Less Screen Time
Of course, technology has provided us with lots of conveniences that we have become accustomed to and may not want to sacrifice completely. If we can’t (or don’t want to) give up technology, are we doomed to fry our brains?
A lot of it might have to do with how we interact with the media, not just how much we interact. Although most studies have focused on the quantity of screen time in hours spent watching, not all screen time is created equally.
One question to ask when it comes to technology and brain health is:
How does the value of whatever you’re doing using technology compare to other things you could be doing?
Or put another way, what’s the tradeoff? If you have free time and feel like doing a deep dive into the biology of narwhals, for example, and that’s the best way you could imagine spending your time, no problem.
But if you’re still on Wikipedia at 3:30 am and you’re losing sleep — or you’re ignoring friends and family in favor of social media — it might be worth re-examining the relationship.
The Bottom Line: Protecting Brain Health in a Digital World
Technology is a fascinating and ever-changing tool of human creation. Like any tool, it can be used to confer great benefits, but used improperly has the potential to cause harm. As the pace of life quickens, it’s more important than ever to slow down, stay aware, and focus on balance.
Last Updated July 7, 2025
Improving Brain Health Naturally at Any Age
Old Beliefs, New Possibilities: Can Brain Health Really Improve With Age?
When it comes to brain health, most scientists used to believe the old saying, “you can’t teach an old dog new tricks.” The long-held belief was that the adult brain lost the ability to grow after a certain age. In other words, the conventional wisdom believed that once we lost certain cognitive functions, they were gone forever. Fortunately, new research has revealed that improving brain health is possible at any age.
Not only is it possible to change your brain at any life stage, but you can improve your cognitive functions just by making a few simple lifestyle changes. Here’s how you can improve your brain health naturally, no matter how old you are!
What is Neurogenesis and Why Does it Matter for Brain Health?
The human brain is home to millions of hard-working neurons, or brain cells, firing their synapses to create connections. As we age, the number of neurons in our brains naturally begins to decline, which can lead to cognitive problems. You might find yourself forgetting where you put your keys more often, or struggling to solve a simple brain teaser that might’ve taken you minutes in earlier years. These small slips in your cognitive functions can become frustrating. They can interfere with your daily life and even become outright debilitating over time. Fortunately, some people can recover their cognitive functions with a little help.
The creation of new neurons is called “neurogenesis.” New research suggests that the brain can continue to create neurons well into adulthood. The findings reveal that adults with Alzheimer’s disease have fewer neurons in their brains than neurologically healthy adults, suggesting that Alzheimer’s disease and a lack of neurons are directly connected.
Treatment options, like the non-invasive HBOT (hyperbaric oxygen therapy) protocol offered at Aviv Clinics, have been shown to stimulate neurogenesis in the adult brain, slowing and even reversing the effects of age-related cognitive decline. It’s also possible to stimulate neurogenesis on your own.
Neuroplasticity Explained: How Your Brain Adapts and Grows
When you experience something new, such as playing your grandkid’s favorite video game for the first time, the stimulation causes the neurons to form new pathways in your brain. The more you play the game and hone your skills, the stronger those connections become. This is “neuroplasticity”—the brain’s ability to change itself in response to new information. With neuroplasticity, your brain can rewire itself by changing its physical structure.
But neuroplasticity can do more than help you level up your gaming skills. Through neuroplasticity, the brain can even restructure itself after suffering an injury, such as a traumatic brain injury (TBI) or stroke, by forming new neural connections in undamaged parts of the brain. Building and strengthening your neural connections is a key aspect of maintaining brain health at any age. Here are a few ways to promote neuroplasticity you can try out at home.
5 Tips for Improving Brain Health Naturally
Eat for Your Brain: Foods That Fuel Neurogenesis
Think of the brain as your body’s engine. If you want your brain to run optimally, you need to give it the proper fuel. Eating processed foods high in saturated fat and sugar can stall neurogenesis, slow your thinking, or cause “brain fog” and other cognitive issues.
The good news is, eating a diet with foods that promote neurogenesis can improve your cognitive health. The omega-3 fatty acids in salmon and fish can increase neuron production. So can the flavonoids in foods like dark chocolate and fresh berries. Even the resveratrol in a glass of wine can give your brain a boost, although drinking in excess can have the opposite effect.
The amount of food you eat and how often you eat also have a role to play. Caloric restriction diets promote neurogenesis, and so do eating methods like intermittent fasting. Try a simple 16:8 fasting schedule and see if your cognitive functions improve.
Move to Improve: How Exercise Enhances Brain Performance
The brain and the body are intimately connected. When one is out of shape, the other can suffer. To give your brain an extra boost, try getting up and moving your body. Studies have shown that physical activity can promote neuroplasticity.
The skills you learn from playing sports like pickleball or golf can stimulate neural connections in your brain. Plus, the physical activity can improve your heart health and help you reach your recommended exercise. You don’t have to run a marathon to see results. The key is to find a physical activity you enjoy doing and to do it regularly. Your body and brain will both reap the benefits.
Learn Something New: Stimulate Neuroplasticity With Mental Challenges
Of course, you can also exercise your brain directly. Just like any other organ or muscle in your body, the brain needs regular stimulation to remain strong. Learning new skills is one of the key aspects of stimulating neuroplasticity in the brain. The possibilities for promoting new neural pathways are endless. You could learn to play a musical instrument, practice speaking different languages, try out a new recipe in the kitchen, or even take a class online.
Playing specialized brain games is one of the best ways to give your brain a good workout. Even solving a crossword puzzle or a challenging Sudoku game can provide extra stimulation. So long as your brain is facing a challenge, then you’re promoting the growth of new neural connections.
Calm the Mind: How Meditation Supports Cognitive Health
Meditation is more than just a way to calm down. It’s an activity you can use to hone your brain’s focus and concentration. Meditating can improve your ability to focus on cognitive tasks by training you to stay present in the current moment. Practicing mindfulness meditation can also ward off stress and anxiety, which can improve mental health. A calm brain is a healthy brain.
Meditation can even slow the progression of Alzheimer’s disease and increase memory recall. You can start seeing positive results in as little as a few weeks of regular practice. The next time you’re having a hard time concentrating, try meditating for a few minutes and see if your cognitive functions improve.

Sleep Smarter: The Role of Rest in Brain Repair
Just like every other age range, older adults need plenty of sleep. Sleep is the vital period when our bodies take the time to recharge after a hard day’s work. It’s when the brain consolidates memories, solidifies learned experiences, and cleanses itself of harmful waste. If you’re not getting enough sleep, you could be sabotaging your efforts to create new neural connections in your brain.
Practicing healthy sleep habits can promote neuroplasticity and improve your overall cognitive health. Try to fall asleep at roughly the same time every night to establish a routine. Avoid consuming caffeine too close to bedtime to prevent sleep disturbances. If you need a nighttime snack that can help boost your sleep, try reaching for a handful of almonds to spark your melatonin production!
The Aviv Clinics Advantage: Taking Brain Health to the Next Level
Cognitive decline doesn’t need to be inevitable as we age. With these consistent lifestyle interventions that promote neuroplasticity and neurogenesis, you can take control of your brain health at any stage of life.
For those seeking to go the extra mile to remain cognitively fit, the Aviv Medical Program offers an evidence-based personalized treatment protocol for brain and body health. The Aviv Medical Program harnesses the power of a unique hyperbaric oxygen therapy protocol and complementary therapies like cognitive exercises, physical training, and nutritional coaching to enhance brain performance. Backed by nearly two decades of published scientific research, this program is designed to help you regain mental sharpness and increase energy using a program personalized specifically for you. If you’re ready to take a proactive approach to brain health and aging, contact us to learn if the Aviv Medical Program can help you unlock your brain’s full potential.
Last Update: July 3, 2025

