Hyperbaric Oxygen Therapy (HBOT) and Stroke
Hyperbaric Oxygen Therapy (HBOT) and Stroke
When a stroke happens and life as you once knew it changes, the road to recovery can feel impossibly hard. But rest assured, all is not lost. Aviv Clinics uses advanced tools and therapies to treat stroke by unlocking your mind and body’s natural rejuvenation abilities. Learn all about Hyperbaric oxygen therapy and stroke so you can regain physical vibrancy and emotional well-being.
What Is a Stroke?
A stroke happens when part of the brain’s blood supply is cut off due to a clot or a blood vessel rupture. This impact stops the brain from receiving the oxygen it needs, causing brain cells to die.
- Stroke is the second leading cause of mortality.
- Stroke is the third highest cause of disability worldwide.
- The prevalence of post-stroke cognitive impairment ranges from 20-80%.
- Survivors may suffer from some form of motor dysfunction or brain impairment (i.e., memory loss, difficulty focusing and processing information, and the inability to reason).
The Primary Types of Stroke
The primary types of stroke are:
- Ischemic stroke: Blood clots, fatty deposits (plaque), or other particles block the blood vessels to part of the brain.
- Hemorrhagic stroke: A weakened artery in the brain leaks blood or ruptures, putting too much pressure on brain cells and damaging them.
- Transient ischemic attack (TIA): Not a true stroke (often called a mini stroke, silent stroke, or warning stroke). These are often caused by blood clots and symptoms should not be ignored.
Ischemic strokes make up 87% of all strokes (including TIAs), with hemorrhagic comprising the other 13%.
Hope exists for stroke survivors with the Aviv Medical Program—a customized medical approach that can help stroke patients achieve improved performance and health.
If you or a loved one has suffered from an ischemic or hemorrhagic stroke or a transient ischaemic attack (TIA), we may be able to help.

What Are the Signs and Symptoms of a Stroke?
Timely intervention is critical with stroke. Two million brain cells die every minute during a stroke, increasing the risk of permanent brain damage, disability, and death.
One helpful tool for remembering the key signs and symptoms of a stroke is the F.A.S.T. acronym:
- F–Facial drooping. Is the person able to smile normally? Does one side of the face droop?
- A–Arm weakness. Can the person raise both arms to equal height? Does one drift downward?
- S–Speech difficulty. Is the person slurring their words or having trouble communicating?
- T–Time to call 9-1-1 immediately.
What Are the Symptoms and Signs of a Silent Stroke?
Some people experience a stroke without realizing it. This is called a silent stroke. Symptoms may go unnoticed or be blamed on other health conditions.
There are 10 symptoms and signs of a silent stroke.
1. A lapse in or loss of short-term memory
- Asking a friend to repeat instructions they just told you
- Unable to remember a recent activity you engaged in
2. A decreased ability to think or reason
- Games (e.g., Sudoku, crossword puzzles) are more difficult than usual
- Feeling frustrated about not being able to understand someone
3. Mood changes
- Suddenly irritable, anxious, apathetic, or depressed
- Crying or laughing for no obvious reason or at inappropriate times
4. Psychiatric disorders
- Having hallucinations or delusions
- Engaging in unusual motor behavior (e.g., nibbling food at the dinner table or repeatedly banging your head)
5. Trouble with balance
- Experiencing dizziness or feeling like your head is spinning
- Having trouble making quick adjustments to maintain balance
- Stumbling or bumping into things
6. Movement or walking impairment
- Toes catching on the ground when walking
- Difficulty walking a short distance
- Trouble walking and talking at the same time
7. Limb clumsiness
- Difficulty controlling hand motions
- Trouble typing on the computer
- Having a shaky leg
- Decreased hand-eye coordination
8. Incontinence
- Feeling the urge to urinate more often than usual
- Consciously or unconsciously leaking urine or stool during the day or while asleep at night
- Trouble emptying your bladder completely
9. Headaches or migraines
- Having more headaches or migraines than usual
- Getting long-term, persistent headaches
- Having headaches become severe enough to disrupt your daily activities
10. Vision issues
- Only seeing clearly with intense concentration
- Experiencing double vision
- A decline in the field of vision
How Can the Aviv Medical Program Help with Stroke Relief?

Most stroke survivors are told that their recovery will plateau after about six months, with only the potential for minimal gains after this period. Gaining functions and abilities more than six months post stroke requires working with a diverse medical team of physicians, nurses, and therapists.
Aviv Clinics leverages its comprehensive team to offer a high-quality program that meets your needs. Backed by over a decade of research, the Aviv Medical Program can combine the following in a customized program to help treat the body and brain after a stroke:
- Cognitive training
- Physical training and therapy
- Dietary coaching
- Hyperbaric oxygen therapy (HBOT)
How It Works: A 3-Step Process
Aviv Clinics’ approach entails a three-step process:
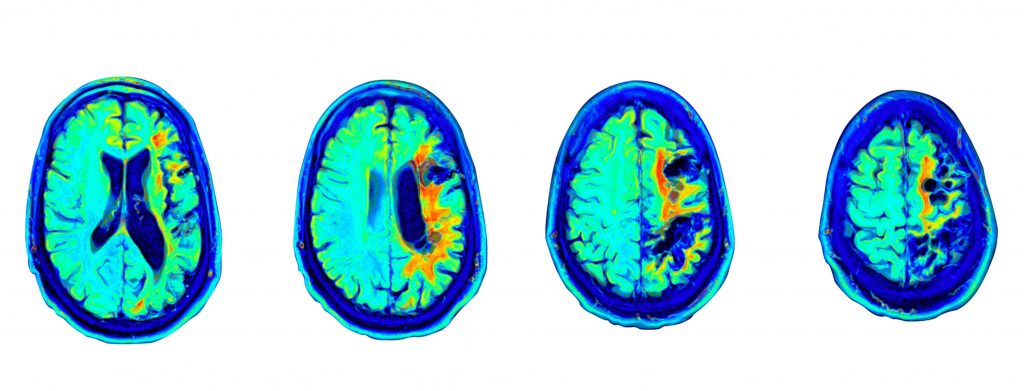
- In-depth medical assessment: We diagnose the severity of the brain injury using the most advanced brain imaging tests suited to your needs—perfusion MRI, fMRI, and/or SPECT. Our medical team also conducts physical, cognitive, and neurological tests to assess the suitability for our program.
- Tailored program: We use your results to develop a personalized, comprehensive therapy plan. This plan can include cognitive and physical training, dietary coaching, and hyperbaric oxygen therapy (HBOT) sessions.
- Post-assessment and evaluation: At the conclusion of your Aviv Medical Program, you’ll receive a detailed report of your results, including any cognitive and physical improvements. We repeat the tests from the initial assessment to measure your progress and make recommendations for ongoing progress.
Watch Cindy’s Remarkable Story
Upon suffering a stroke, Cindy sought the help of the Aviv Medical Program.
Learn what her program was like and how her brain and body benefited.
“Because of Aviv, I’m now walking without a cane. The fog and fear are gone. I got in a golf cart within six weeks from the time I started!”
“It didn’t take long at Aviv before I had the courage to try new things. The therapy I’ve gotten, it’s incredible.”
Speak with an Aviv team member to learn if you’re a candidate for our program.
Stay educated on stroke by joining our on demand webinar.
Recovering After a Stroke: Is it ever too late?
The 5 Stages of Stroke Recovery
There are five support stages to post-stroke recovery. Each stage represents a milestone that gets you closer to optimal health.
- Thinking, memory, and perception training: Neuropsychologists typically step in and assesses measures memory, learning, and processing speed.
- Communication and language training: Stroke patients with aphasia are often referred to speech-language pathologists (SLPs). SLPs help individuals relearn communication and language techniques. One study found when early aphasia therapy is provided, “people have a massive increase in their ability to communicate at 12 to 26 weeks after their stroke.”
- Exercise and mobility training: Physical challenges are common among stroke survivors, meriting a physical therapist (PT) who can help patients relearn and regain physical activity. Consistent PT lowers the risk of hospital readmission among post-stroke patients.
- Nutritional training: Nutritional training can be beneficial, especially for those who are unable to swallow well or experience difficulties using their arms/hands to eat. Dieticians can also address those concerns and provide recommendations.
- Hyperbaric oxygen therapy (HBOT): More than a decade of research illustrates the benefits of using HBOT post stroke. HBOT for stroke patients is a therapy process where patients are prescribed time in an oxygen chamber, breathing in 100% oxygen at fluctuating levels. Researchers have noted significant improvement in stroke patients after treatment with HBOT, even several years after the stroke.
What Role Does HBOT and Stroke Play in Improving Your Post-Stroke Life?
Aviv Clinic’s hyperbaric chambers pressurize air to above atmospheric levels. This environment increases oxygen levels in the body up to 20 times higher than normal, delivering oxygen to damaged cells injured by stroke.
The Aviv unique HBOT protocol for stroke uses a scientifically validated process in which oxygen levels fluctuate throughout the session. This fluctuation triggers the body into cell repair and regeneration mode.
What Benefits Can Stroke Survivors Achieve?
When combined with personalized cognitive, physical, and nutritional plans, HBOT as a part of your stroke regimen may produce impressive outcomes, even years after a stroke:
- Regained speech and ability to read/write
- Restored motor function, even with paresis
- Return to independence in performing daily activities
Many of our clients report the biggest benefit is simply not being “a burden” on their loved ones.
Here is the full breakdown of how our medical program can impact the brain, body, and cells even years after suffering a stroke.
Benefits for your brain*:
- Rejuvenation of injured brain tissue, restoring some impacted functions
- Increased blood flow in the parts of the brain associated with sensation, memory, vision, and attention
- New stem cells and blood vessels in the brain (angiogenesis)
- Improved psychomotor function (the combination of precise motor responses and cognitive problem-solving abilities)
- Triggered neuroplasticity (the brain’s ability to adapt/react in response to injury or disease) in injured parts of the brain
- Triggered neurogenesis (neuronal, or nerve cell) regeneration that occurs in the brain.
- Improved overall quality of life
*Individual patient results may vary.
Benefits for your body*:
- Better physical performance: mobility, fitness, strength, coordination, balance, gait
- Improved NIHSS (neurological motor function score), ADL (activities of daily living score), and EQ-5D (quality of life score)
- Boosted power and stamina
- Reduced pain (strong anti-inflammatory effect)
- Improved sleep quality
- Improved sexual performance
*Individual patient results may vary.
Benefits for your cells*:
- Strengthened immune system
- Encouragement for stem cells (the building blocks of tissue rejuvenation) to multiply and migrate
- Lengthened telomeres (the protective caps at the end of each strand of DNA) associated with extending our biological clock
- Reduced senescent cells (known to contribute to many age-related diseases)
- Increased mitochondrial function (the power center of the cell)
*Individual patient results may vary.
How Soon after a Stroke Can a Patient Participate in the Aviv Medical Program?
We recommend waiting three to six months after the stroke to participate in the Aviv Medical Program. This time allows the brain’s natural-healing progression to take hold, but even years after suffering a stroke, patients can see significant improvements. We’ve seen success in clients who were as many as 10 years into their stroke recovery.
Aviv Clinics Is Changing the Lives of Stroke Victims, One Patient at a Time
Backed by over 15 years of research, the Aviv Medical Program was formed under the scientific leadership of Dr. Shai Efrati—Director of the Sagol Center for Hyperbaric Medicine and Research at the Shamir Medical Center in Israel. Recent clinical studies at the Shamir Medical Center have evaluated the effects of HBOT on stroke patients suffering from neurological deficiencies.
Over 2,000 clients have been successfully treated with the Aviv protocol to date.
Post-Stroke Recovery: 4 Tips to Keep in Mind
To ensure the most successful post-stroke recovery, stay mindful of the following:
- Several factors influence recovery: What recovery looks like and how long it takes is different for everyone because of where in the brain the stroke happened, how much of the brain was affected, and other factors.
- Repetitive practice is key: Just like learning a new musical instrument, repetitive practice is the most important element in any neurorehabilitation program.
- Recurrent stroke prevention should be approached with vigilance: Nearly one in four stroke patients has had a stroke in the past.
- Measuring progress matters: Working with a premier medical staff that captures and tracks data is critical to success. The Aviv Medical Program tracks analytics to provide a detailed report of your health and progress.
Speak with an Aviv team member to learn if you’re a candidate for the program.
Can You Biologically Reverse Your Age? Science Says It’s Possible
With specialized health programs and the right hyperbaric oxygen therapy (HBOT) protocol, it may be possible to reverse your biological age. How? It involves targeting the key biomarkers responsible for the body’s aging process. This quick guide dives into all the details.
Learn more about age-related decline and how Aviv Clinics can help.
What Are the Two Types of Age?
First, it helps to understand the two types of age:
- Chronological age or how many birthdays you have had
- Biological age or “the aging of our body’s functions”
Biological age refers to how old a person’s body and cells actually are. It’s often measured by evaluating a person’s various biological markers, such as:
- Epigenetic changes: Your behavior and environment can impact how your genes function.
- Telomeres: They protect the ends of chromosomes from deterioration. As we age, our telomeres naturally shorten. A yearly decrease of their length by 20–40 bases is associated with serious illnesses.
- Senescent cells: Over time, these cells can accumulate in the body and prevent cells from growing. The increase in senescent cells contributes to age-associated conditions.
- Stem cell exhaustion: The growth of senescent cells with age causes the activity of stem cells to slowly decrease.
Additionally, biological age takes into account a person’s:
- Health
- Lifestyle choices
- Genetics
A healthy adult who has a chronological age of 60 years can be much younger in biological age if they have long and healthy telomeres and a healthy amount of senescent cells—areas that can be achieved with the right lifestyle.
Researchers note “biological age is a better predictor of morbidity risk than chronological age.”

Does Hyperbaric Oxygen Therapy (HBOT) Reverse Aging?
A unique protocol of HBOT has been scientifically proven for reversing biological age.
Several studies illustrate HBOT, when administered in a specific protocol:
- Improves cognitive, physical, and psychological performance. These areas ultimately help promote healthspan and longevity.
- May increase telomere length and encourage the “clearance of senescent cells.” This illustrates the potential HBOT has in slowing aging.
Keep in mind, the type of HBOT protocol is important. Not all HBOT programs are created equal. There are different types of oxygen chambers, and each provides a unique process. Reversing biological age has been scientifically proven only in multi-chamber suites, such as those at Aviv.
The Aviv Medical Program
The Aviv Medical Program offers a more robust and extensive treatment program compared to other clinics. The program has been clinically proven to reverse biological aging by:
- Lengthening telomeres
- Reducing senescent cells
- Stem cell proliferation
- Targeting other areas of the brain and body to improve cognitive and physical performance
Our program consists of a treatment plan that begins with:
- In-depth review of health history
- Comprehensive physical and neurological exams
- Highly advanced brain imaging scans
- Neurological and neurocognitive tests
- Body composition analysis
- A detailed report of our assessment findings
Based on the results of the above, as well as your goals, needs, and symptoms, your customized medical program can also include:
- Cognitive training
- Physical training
- Dietary coaching
- Hyperbaric oxygen therapy (HBOT) provided in the specific protocol used in the above studies
All of this is included in Aviv’s physician-designed program tailored to each client’s needs.


4 Ways the Aviv Medical Program and HBOT Can Promote Reverse Aging and Actionable Tips
Let’s dive more into specifics and break down the four main ways HBOT can help reverse aging. You’ll also find additional strategies to give your mind and body the holistic care they need for optimal performance.
Note: Speak to your doctor before you pursue any lifestyle changes.
1. Cognitive Health
Common cognitive decline with age includes memory issues, language processing, and sleep disorders.
Health experts note harnessing oxygen via HBOT along with cognitive training can help. Breathing in a pressurized environment with fluctuating oxygen levels can:
- Turbocharge the body’s self-healing mechanisms.
- Slow down the biological aging process.
Cognitive training inside the HBOT suite can be more effective as well. For example, Aviv Clinics provides each patient with a tablet, so they can engage in brain exercises during their HBOT sessions.
Additional Strategies for Optimal Cognitive Performance
- Find healthy ways to cope with stress: If not managed, chronic stress can take a neurological toll, raising the risk of cognitive issues (e.g., memory and attention problems). Safeguard your cognitive health by engaging in healthy coping mechanisms for stress.
- Engage in brain games: Playing brain games can improve cognitive performance and enhance the overall quality of life. The fact that these games are fun is just the icing on the cake.
2. Physical Health
Our bodies grow less efficient at channeling oxygen when we age. This is one of the reasons why we may feel “slower” in terms of mental and physical performance.
Research shows a specific HBOT protocol may:
- Optimize athletic performance by helping you elevate aerobic stamina, heal faster post-injury and more
- Minimize pain via anti-inflammatory effects
Additional Strategies for Optimal Physical Performance
- Exercise regularly: Commit to at least 30 minutes of exercise three days a week. Make sure your exercise regime involves cardio and strength training.
- Engage in intermittent fasting: Not only does intermittent fasting promote weight loss, but this metabolic switching can also help enhance the brain’s ability to resist injury and disease.
3. Mental Health
Mental health is another vital area to nourish with age. It is estimated that 20% of people age 55 or older experience some type of mental health concern. This may be attributed to life changes or events and injuries (e.g., TBIs, concussions, mini-strokes).
Evidence suggests a proprietary HBOT plan can:
- Improve neuroplasticity, or the brain’s ability to adapt in response to an injury or disease. This means the brain can rewire itself after suffering an injury and strengthen its neural connections—key aspects to improving and maintaining cognitive health.
- Enhance brain functionality in those with PTSD, helping PTSD survivors alleviate their symptoms.
Additional Strategies for Optimal Mental Performance
- Try meditation: Meditation offers many brain health benefits, such as helping to cope with anxiety, depression, and overall mood. Following a simple daily practice will provide moments of groundedness and clarity.
- Lean on your support system: Reach out to family and friends for support. Human connection can be a lifeline to healing.
4. Sexual Health
Various reports state that “frequent sex can improve…our general quality of life and may even extend our life by years.”
“Men tend to marry younger women, die sooner and care more about sex.” But until what age is a man sexually active?
Experts say, “at age 55, men can expect another 15 years of sexual activity.” But this stat isn’t universal—conditions like erectile dysfunction (ED) can minimize the quantity and quality of sexual health.
Luckily, studies illustrate HBOT may be a promising supportive or independent treatment for ED. It can encourage new blood vessel formation and improve blood flow, which can help recover erectile function.
Additional Strategies for Optimal Sexual Performance
- In addition to HBOT, take good care of your physical, mental, and cognitive health with the suggestions we’ve listed above.
- According to researchers, “Modifiable risk factors for ED include smoking, lack of physical activity, wrong diets, overweight or obesity, metabolic syndrome, and excessive alcohol consumption.”
- Therefore, following a healthy diet and exercise regime are key to overcoming ED and promoting better sexual activity in older adults.
Invest in HBOT to Reverse Your Age
Reversing your age may sound fantastical, but with the right medical team by your side, that goal may be possible.
Learn more about the benefits of investing in your health and how Aviv Clinics can help.
3 Critical Takeaways: The Research behind Hyperbaric Oxygen Therapy (HBOT) for Stroke Patients
Numerous research studies have been conducted on hyperbaric oxygen therapy (HBOT) for stroke patients, and the results of many of those studies are available on our site. To help consolidate all the information, we’re highlighting the most relevant research areas regarding stroke to help you stay informed and make smarter decisions as you resume your day-to-day life after your stroke.
Research and data are at the core of the Aviv Medical Program. Our team strives to use the peer-reviewed, evidence based research to improve our clients’ individual health outcomes. So keep reading to glean the latest insights, expertise, and guidance.
Our goal is to help you take ownership of your health—to proactively improve your quality of life.
HBOT for Stroke Patients: 3 Key Research Takeaways
The Sagol Center for Hyperbaric Medicine and Research In Israel and Aviv Clinics’ medical staff have led many HBOT studies on post-stroke patients. These studies have played a significant role in developing our unique HBOT protocol.
Our research and findings uncovered four critical takeaways on HBOT and post-stroke conditions.
1. Improved Motor Function and Quality of Life
Research Study
Objective
The study evaluated whether a specialized HBOT protocol could activate neuroplasticity (the brain’s ability to create new neural connections) and improve motor function and quality of life in post-stroke patients..
Methods
The study involved 74 patients, all of whom “suffered a stroke 6-36 months prior to inclusion and had at least one motor dysfunction.”
Researchers split participants into two groups:
- The first group’s patients were evaluated twice—at baseline and after 40 HBOT sessions.
- Patients in the second group were evaluated three times—at baseline, after a two-month control period, and after 40 HBOT sessions.
Results/Conclusions
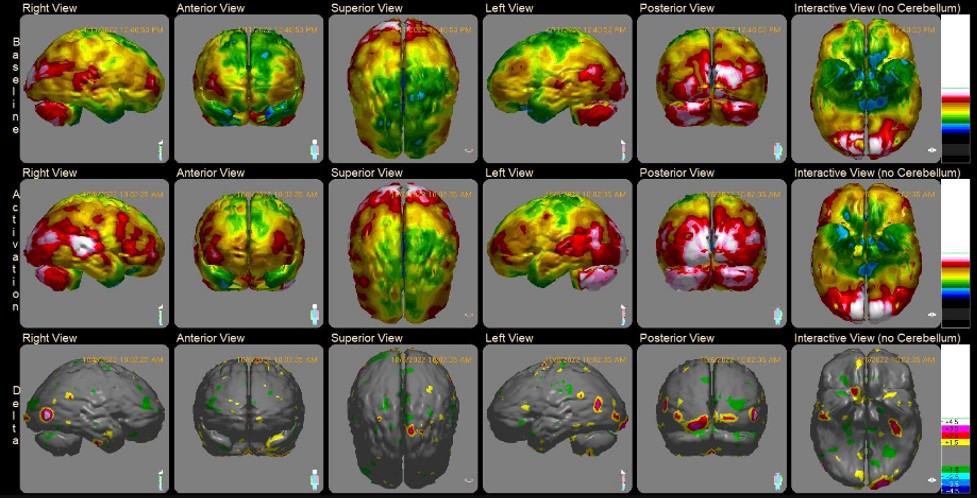
The study found neurological functions and quality of life in both groups were “significantly improved following the HBOT sessions.” However, no improvements were demonstrated during the control period of the patients in the second group. Additionally, the neurological changes correlated with imaging findings: areas with low function/metabolic activity following the stroke were re-activated.
These results have shown “neuroplasticity can be activated” even long after the stroke event.
2. Improvement in Memory Impairments
Research Study
Improvement of Memory Impairments in Poststroke Patients by Hyperbaric Oxygen Therapy
Objective
More than 50% of stroke survivors suffer from cognitive impairments. This study aimed to assess the specific impacts of a specialized HBOT protocol on “memory impairments after a stroke at late chronic stages.”
Methods
Researchers conducted the study on 91 stroke patients who either had ischemic or hemorrhagic strokes within the past “3-190 months prior to treatment with HBOT.”
For reference:
- An ischemic stroke happens when a blood vessel that supplies blood/oxygen to the brain becomes blocked via a blood clot or fatty deposits (plaque).
- A hemorrhagic stroke occurs when an artery in the brain leaks or ruptures.
The HBOT protocol entailed daily HBOT sessions—five days per week, 90 minutes each, for up to 12 weeks.
Patients underwent computerized memory tests before and after the program.
Results/Conclusions
There were significant improvements in “all memory measures after HBOT”, including both immediate and delayed memory domains. These progressions were linked to better brain metabolism, mainly in the temporal areas.
The results illustrate the potential of hyperbaric oxygen therapy in managing memory impairments in post-stroke patients, even years after the incident.
3. Enhancement in Neurocognitive Functions
Research Study
Objective
This study aimed to assess the impact of a specialized hyperbaric oxygen therapy protocol on cognitive functions in those dealing with post-stroke cognitive symptoms at the late chronic stage.
Methods
Participants were treated in a multi-place hyperbaric chamber where they received 40-60 total daily sessions of HBOT, five days a week.
Different factors which may affect the results of the treatment were explored:
- Those who suffered from cortical strokes (i.e. the outer surface of our brain), compared to those who suffered from deep/inner regions strokes.
- Those who suffered from ischemic strokes (see above), compared to those who suffered from hemorrhagic strokes.
- Those who suffered from strokes in their dominant hemisphere (the side responsible for speech, usually the left side in right-handed patients), compared to non-dominant hemisphere (usually the right side in right-handed patients).
Results/Conclusions
HBOT sessions improved “all the cognitive function domains, including memory, attention, processing speed, planning (executive functions) and coordination with 86% of the stroke victims achieving a clinically significant improvement”.
The main predictor for cognitive improvement was a decreased metabolic function on imaging rather than the type of stroke, the side or region of the stroke.
These improvements offer hope that patients can still gain cognitive improvements even at a late, chronic post-stroke stage.
The Aviv Medical Program—A Research-Backed Program
The Aviv Medical Program is founded in part on the research studies outlined above. By making data-driven decisions, our clients have achieved better cognitive and physical performance. We understand every individual is unique, with different post-stroke symptoms and challenges. Thus, not every person will be a candidate for our program. Our rigorous assessment process will determine whether the program is right for you.
Our post-stroke program remains focused on research and leans on a holistic and personalized approach. Depending on your symptoms, needs, and goals, it can include the following:
- In-depth review of medical history
- Comprehensive physical and neurological exam
- Physical therapy evaluation
- Gait analysis, when relevant
- Highly advanced brain imaging scans
- Neurocognitive tests
During the treatment, the program can include a combination of:
- Cognitive training
- Physical training
- Dietary coaching
- Hyperbaric oxygen therapy (HBOT) provided in the specific protocol from the mentioned studies
Dr. Mohammad Elamir, MD, FACP, explains the post-stroke program at Aviv Clinics in more detail:
Stay educated on stroke by joining our on demand webinar.
Recovering After a Stroke: Is it ever too late?
Navigate Your Post-Stroke Journey with Aviv Clinics
Contact Aviv Clinics to learn more about hyperbaric oxygen therapy in Florida. We will take the time to understand your health background, issues, and lifestyle to determine whether the Aviv Medical Program is the right fit.
Ways to Enhance Your Post-Stroke Journey: 10 Brain Exercises for Stroke Recovery
When we think of exercises, we often think about movement. As much as physical activity is essential to post-stroke health, mental exercises are just as important.
Given that “cognitive impairment and memory loss are common after a stroke,” patients are often encouraged to consider brain exercises for stroke recovery along their rehabilitation journey.
The good news is the brain is a powerful organ that can learn at any age. Medical experts note, “The reality is that everyone has the capacity to develop new cells that can help enhance cognitive functions.” The more you engage your brain, the better the chances you will see cognitive improvement.
Brain exercises can unlock this potential. Below, we offer insights into several types of brain exercises for stroke relief. We also discuss the training Aviv Clinic’s post-stroke program can offer, so don’t miss out.
1. Devices and Apps for Stroke Patients

Certain devices and apps provide access to speech and cognitive activities. Though most apps are not specifically for stroke patients, they can still help with neurological rehabilitation—recent studies have found that “mobile apps can be used to improve stroke rehabilitation” by supporting physical and cognitive skills.
One tip is to look for “psychomotor skill” apps that calibrate themselves to an individual’s motion range. These can be especially useful for stroke patients.
Here are examples of helpful devices and apps for stroke patients:
- BrainHQ is a cognitive training app. The app offers several games that help Aviv Clinics’ clients improve skills that stroke survivors may struggle with—such as memory, attention, brain speed, and navigation. You can even design your own program, choosing exercises and workouts that meet your personal interests.
- MindMaze has a helpful game-based digital therapy called MindMotion™ GO. It offers full-body motion capture, allowing patients to practice physical and cognitive exercises at the same time. This is exclusively used in clinical settings; you will need a physician or therapist to help you sign up for this app.
- Lumosity offers exercises for your mind with a fresh set of games daily to keep your brain consistently challenged. The app also provides reports that track your progress.
- VAST is a virtual reality rehabilitation system we use at Aviv Clinics. It offers the flexibility to work in any physiotherapy practice and helps our patients engage in moto-cognitive activities. This is exclusively used in clinical settings, and you will need a physician or therapist to help you sign up for this app.
- CogniFit features brain training that includes psychologist-developed games and a personalized program for each user, adapted to your specific needs.
Using Tech to Practice Psychomotor Skills

Because they involve both cognitive prompts and physical movement, apps and devices are great ways to improve psychomotor skills such as:
- Coordination
- Balance
- Fine motor skills
- Reaction time
Psychomotor skills are vital for everyday activities, making these particular brain exercises for stroke recovery especially beneficial for supporting independence in dressing, cooking, driving, and practicing self-care.
Keep in mind that while some free apps feature psychomotor exercises, many of these apps and devices require the involvement of a healthcare professional, such as a physician or therapist. When used in clinical settings, these technologies can have impressive results:
- In one study, post-stroke patients demonstrated significant improvements in motor function after using MindMaze’s VR-based rehabilitation programs—an average improvement of “15.4% at [their] one-month follow-up.”
- Another study found that between one and three months of “medium-high intensity computerized cognitive training showed significant improvement on global cognition for stroke patients.”
2. Games for Stroke Patients

Games are not only fun, but they can also improve cognitive performance.
Puzzles
Games like crossword puzzles, Sudoku, and word searches are excellent activities to stimulate the brain.
The most impactful? Crossword puzzles. Researchers specify crossword puzzles are “superior to other brain games in improving memory.”
Let’s not forget the accessibility crossword puzzles offer: You can find them anywhere—online, in newspapers, and on smartphone apps—and they can easily be taken on the go.
Jigsaw Puzzles
Jigsaw puzzles are another excellent form of brain exercise for stroke recovery, as they help to support and improve:
- Concentration and focus
- Visual-spatial skills
- Fine motor skills
- Problem-solving
- Memory
For post-stroke patients, it’s been shown that jigsaw puzzles “can improve upper extremity fine motor skills” and increase finger strength and range of motion.
Completing a puzzle can also provide a much-needed sense of accomplishment, boosting your mood and well-being during your recovery.
Board Games
Board games often require critical thinking and teamwork.
Playing board games—like Scrabble, Connect Four, and Battleship—stimulates brain areas that oversee memory formation and thought processes. Games do this by:
- Encouraging high-level thinking. Board games can improve brain skills like strategic thinking, logic, attention, memory, and comparison. Researchers report that “playing non-digital games may be a positive behavior in terms of reducing cognitive decline.”
- Enhancing creativity and self-confidence. The collective nature of board games can help post-stroke patients with creative problem–solving while connecting with their friends and family.
Some of the most popular games can help improve brain cognitive health, including checkers, memory matching games, dominoes, and card games. However, the list is endless.
Chess
Chess, a game already associated with brain-boosting benefits, is another way to use play to support brain health.
According to Roger Miller, PhD, lead neuropsychologist at Aviv Clinics, chess can strengthen your executive function by exercising your prefrontal cortex, the “CEO of the brain.”
Regular chess games can also sharpen your decision-making skills, improve concentration, and foster creativity through strategy.
Video Games

In a study where post-stroke patients played Wii Sports Resort—a collection of sports simulation mini-games:
- The group who played video games “achieved better results than the control group.”
- Among attention, processing speed, and working memory, “the attention and processing speed improved” the most.
These results illustrate the potential video games have in supporting cognitive rehabilitation after a stroke. Like board games and puzzles, video games can offer the stimulation the brain needs to enhance critical thinking and memory.
One study even notes that motor-sensor video games could offer physical benefits. When working with a therapist, the games “allow patients recovering from a stroke to improve their motor skills and affected arm movements.”
3. Lifestyle Activities for Stroke Patients

Here are some lifestyle activities for stroke patients that shake things up by offering more diverse, non-digital options that can create balance in your life.
Reading
Many brain exercises for stroke recovery focus on treating aphasia, a frustrating post-stroke symptom that interferes with your ability to read, write, and understand language. Offering more than a way to exercise language skills, reading can serve as a form of enjoyment or an escape to new worlds.
In addition to novels, the benefits of reading can be enjoyed through:
- Magazines
- Newspapers
- Online articles
- Audiobooks
Because persistent language impairments affect as many as “one in five stroke survivors in the United States,” it’s essential to read at your own pace with respect to wherever you are in recovery.
Music
Listening to music offers an emotive experience that enhances mood and improves memory. Frequently, a specific song elicits certain memories or forms new ones.
Studies note that music therapy can be a good “motor function rehabilitation” method. Listening to music or singing songs can help “promote neural plasticity”—the ability of the nervous system to adjust itself—and improve “patients’ motor function.”
Have you been interested in learning to play a musical instrument? This activity may offer additional benefits, as “listening to and performing music reactivates areas of the brain associated with memory, reasoning, speech, emotion, and reward.”
Spending Time Outdoors
Getting outside offers numerous benefits for stroke survivors, including brain health.
Just spending time in nature can help—researchers have found plenty of evidence for the “protective effects of exposure to natural environments on mental health outcomes and cognitive function.”
While outside, there are many activities you can engage in, including:
- Gardening
- Birdwatching
- Picnicking
- Nature walks
- Beachcombing
Time spent outside in scenic areas can also reduce stress as you enjoy the calming effects of nature.
4. Art Therapy

Engaging in various art mediums is a wonderful outlet for non-verbal, creative expression and a powerful brain exercise for stroke recovery that encompasses several skills.
Post-stroke patients report that art therapy can “significantly decrease depression, improve physical functions, and increase quality of life compared with physical therapy alone.”
Painting
Picking up a paintbrush can be a therapeutic and enriching way to practice fine motor skills and sharpen cognitive skills at the same time. The American Congress of Rehabilitation Medicine (ACRM) recommends painting for stroke survivors to strengthen memory, foster creative growth, practice problem-solving, and rebuild motor skills.
Photography
The Stroke Association recommends photography as a leisure activity. Take a walk around a nearby park or nature sanctuary and take some photos. Photography can be a therapeutic activity that offers a healthy and peaceful distraction. You’ll also get a chance to move your body while snapping pictures.
Dance
Does dance fit in as a brain exercise? This one requires more movement than most items on this list, but it fits in with art therapy, and there’s no need to break a sweat to reap the cognitive benefits.
Even if you’ve never been much of a dancer, it’s never too late to start. For post-stroke patients, “dance and rhythmic movements guided by music facilitate the whole-body connection and coordination.” This challenges both the brain and body at once to coordinate your movements to the music, which can also be an enjoyable exercise. Consulting with your physician before starting a physical exercise program is always a wise decision, especially considering potential risks like falls.

5. Breathing Exercises
While dedicated breathing exercises can help you slow down and take time to relax, it’s also a surprisingly effective brain exercise for your stroke recovery journey.
Methodical breathing techniques optimize oxygen delivery throughout the body. In post-stroke patients, regular breathing exercises were found to calm the nervous system, prompting “psychological changes and improved cognitive functions.”
Several different exercises may be beneficial for stroke relief, including:
- Diaphragmatic breathing
- Box breathing
- Alternate nostril breathing
- Pursed-lip breathing
There are also several videos, podcasts, and apps that can guide you through a regimen and incorporate regular breathing practice into your routine.
6. Visualization Exercises

In a study where post-stroke patients used visualization techniques to picture themselves successfully completing motor tasks, participants experienced enhanced “functional rehabilitation of both upper and lower limbs, as well as for the recovery of daily activities and skills.”
This is because visualization can stimulate the same neural pathways associated with movement, coordination, and memory. To practice visualization throughout your rehabilitation journey, set aside quiet time each day to visualize yourself overcoming challenges and regaining mobility according to your goals.
Alternatively, guided visualizations led by your healthcare provider or counselor can offer personalized support and encouragement throughout the process.
7. Socialization
Being with others can help improve feelings of depression and isolation, which are common experiences for stroke survivors. Here are some ways you can socialize during your recovery:
- Join a support group.
- Spend time with friends and family.
- Participate in community activities.
- Connect with online forums and communities.
- Locate volunteer opportunities.
Engaging with others is not only important for brain health, but research shows that “social interaction improves quality of life and decreases mortality after stroke.”
8. Mindfulness Meditation

There is a large body of research connecting mindfulness practices to neuroplasticity, or the brain’s ability to adapt and recover from damage. For stroke survivors, this is a crucial consideration. The link between mindfulness meditation and neuroplasticity has implications for stroke outcomes:
- Numerous studies have found that “meditation practices have various health benefits, including the possibility of preserving cognition.”
- The practice offers post-stroke patients support, as “mindfulness skills may also raise concentration levels and support restorative, brain-healing rest in recovery from stroke.”
It may seem counterintuitive that practiced stillness could be considered a brain exercise for stroke recovery and rehabilitation, but this powerful practice can help the brain reorganize and regain important functions. Harnessing the brain’s capacity for neuroplasticity can facilitate recovery by rewiring neural pathways and compensating for damaged regions of the brain.
9. Speech Therapy
For those living with aphasia or other communication challenges, speech therapy can provide support for the physical and cognitive aspects of communication.
Speech therapy can improve overall well-being for a large number of post-stroke patients—“communication impairment occurs in 30–60% of stroke survivors.” This is largely accomplished through:
- Articulation exercises
- Language drills
- Strengthening facial muscles
- Augmentative and alternative communication devices
- Building confidence and self-assurance
Because it’s most effective when initiated quickly after a stroke, it’s important to start speech therapy, if needed, as soon as possible.
10. Learning New Skills

After a stroke, it’s normal to not feel up to doing the things you used to do. Many post-stroke patients find it difficult, with a return to normal hobbies and activities “reduced between 10% and 40%” in survivors.
While you may not want to resume your old leisure activities, now is a great time to try something new—developing unfamiliar skills helps stimulate the brain and foster cognitive recovery.
Learning something new can challenge your brain while offering a sense of achievement with every new skill you acquire. Examples of new activities to try include:
- Playing an instrument
- Painting or drawing
- Learning a new language
- Cooking
- Trying a new exercise
- Participating in a group activity or class
Neurobics
Like aerobics for your neurons, neurobics refers to any task or activity that challenges your brain in new ways. Used as a novel brain exercise for stroke recovery, “neurobic exercise intervention could improve subjective and objective memory.”
Neurobics can be as simple as performing familiar tasks in novel or unconventional ways to stimulate different areas of the brain. For example:
- Brush your teeth with your non-dominant hand.
- Take a new route when walking or driving.
- Try a new game or puzzle.
- Change the order of a daily routine.
The goal is to stretch and strengthen your memory, concentration, and overall cognitive function.
Aviv Clinics: Post-Stroke Program

The Aviv Medical Program offers a comprehensive post-stroke program targeted to those in the chronic post-stroke phase, typically six or more months after the incident. This program may entail cognitive exercises in addition to physical and nutritional training.
The Aviv Medical Program consists of a plan that can include the following:
- Cognitive training
- Physical training
- Dietary coaching
- Hyperbaric oxygen therapy (HBOT)
To determine the best course for you according to your goals, we create a personalized program to support your well-being based on the results of a comprehensive evaluation:
- In-depth review of health history
- Comprehensive physical exam
- Highly advanced brain imaging scans
- Neurological and neurocognitive tests
- Body composition analysis
- A detailed report of our assessment findings
- A post-program report of your improvements and recommendations for future progress
All components of this plan are included in a physician-designed program tailored to the needs and goals of each patient.
Cognitive Training Program

The cognitive training portion of the Aviv Medical Program is performed both inside and outside our hyperbaric oxygen suites. During HBOT sessions, your brain and body unlock their regenerative mechanisms through the use of cognitive games like BrainHQ. This helps you become more receptive to other forms of therapy.
As part of your treatment, you may also complete our unique cognitive training regime while exerting yourself physically on the cutting-edge h/p/cosmos medical treadmill. Research shows this combination of physical and cognitive effort, also known as dual task training, maximizes the benefits of the Aviv Medical Program, taking your brain and body to the next level.
Post-stroke patients benefit from this combination. In one study, “dual task training effectively improved upper extremity function and the performance of daily activities in chronic stroke patients.”
During the assessment process, each client receives a thorough evaluation to identify specific areas of strength and areas for improvement. Tailored cognitive exercises are then used to target areas of need, such as:
- Memory
- Information processing
- Attention and focus
- Executive functioning
Combining our unique HBOT protocol with a combination of body and brain exercises for stroke recovery brings significant benefits for stroke survivors at various stages: “HBOT can lead to significant neurological improvements in post-stroke patients even at chronic late stages.”
After Cindy, a stroke survivor, learned about the Aviv Medical Program, she underwent a transformation that now allows her to lead an independent life.
Watch Cindy’s story:
Find Hope with Aviv Clinics
Life after a stroke can be challenging. A stroke can suddenly strip away the capabilities we take for granted. Support, trust, and consistency are vital to getting back to optimal health. The medical team at Aviv Clinics offers all three elements while crafting a personalized rehabilitation plan specifically for you.
There is hope after a stroke. Learn more about the Aviv Medical Program for stroke relief, including the unique hyperbaric oxygen protocol at Aviv Clinics.

FAQ
Are there any potential risks or limitations associated with brain exercises for post-stroke recovery?
Brain exercises for stroke recovery are a non-invasive, low-risk option for post-stroke rehabilitation. It’s important to follow your doctor’s guidelines, especially in the early stages of recovery. Keep in mind that the effectiveness of brain exercises may depend on individual differences and access to specific resources.
How frequently should brain exercises be practiced for optimal results?
How often you perform brain exercises for stroke recovery depends on your needs and the specific exercises performed. Because the brain responds well to consistency and regular stimulation, many experts recommend practicing exercises frequently, as often as daily, but ideally several times per week. Always consult your physician for the ideal frequency.
Why are brain exercises important for post-stroke recovery?
Brain exercises are important for post-stroke recovery for several reasons, including:
- The potential for neuroplasticity
- Cognitive rehabilitation
- A sense of engagement and accomplishment
- Reduced risk of cognitive decline
The use of brain exercises for stroke recovery can also provide an enjoyable way to approach rehabilitation in addition to other treatments, exercises, and therapies.
Can brain exercises be integrated into post-stroke rehabilitation programs?
Yes, brain exercises can and should be incorporated into post-stroke rehabilitation programs. This can provide a structured approach to cognitive rehabilitation, including various brain exercises and training activities tailored to each person’s needs and goals. Healthcare professionals can provide valuable guidance and feedback for brain exercise programs to help stroke survivors achieve success through their rehabilitation journey.
6 Trends in Healthcare in 2023
Healthcare is rapidly evolving, and it’s important to stay aware of these shifts to activate your role in driving better health outcomes for yourself and your loved ones. Patients have higher expectations and want to take more ownership of their health through the convenience of personalized, educational, and digital care.
Alongside these growing expectations, here are six other trends in healthcare to help you know what you might expect this year.
1. Remote Patient Monitoring (RPM)
The COVID-19 pandemic showed how critical technology could benefit patients and elevate care. One way to achieve this has come through remote patient monitoring (RPM).
In 2022, RPM tools (e.g., wearable devices, pulse oximeters, blood glucose meters, and heart monitors) had a value of $53.6 billion. The value of this market is projected to reach $175.2 billion by 2027.
When 6 in ten people live with at least one chronic disease, the ability to manage a condition remotely is one key element in preventing or reducing hospitalizations. Another critical area to achieving this goal is education, bringing up our next point.
2. Health Literacy
With more doctors remotely managing patients’ health, healthcare organizations are providing digital, personalized educational experiences. These experiences address each patient’s health literacy level in their preferred language and reading level.
More providers anticipate higher patient volume in the coming year, as 41% of individuals delayed or avoided medical care during the pandemic. When seeking treatment or care, you’ll likely receive additional educational materials at each touchpoint of your journey. Discuss literacy levels with your doctor throughout the process to ensure you feel confident and comfortable navigating your health needs.
3. Mindfulness Products
Wellness has taken center stage since 2020, and mindfulness is one of the most in-demand aspects of this concept.
- McKinsey reports mindfulness has gained mainstream acceptance among healthcare patients. Half of the survey respondents wished more mindfulness products and services were available.
- Medical research points toward brain health benefits of mindfulness exercises such as meditation.
You may see a rise in providers offering more holistic care. For example, healthcare organizations may consider partnering with mindfulness apps or providing products that offer you mental health benefits.

4. Data Analytics
Objective data is critical. It illustrates your progress and determines what steps you and your physician need to take to help you reach your health goals.
More providers are tracking and sharing data that reports:
- Patient interaction with educational materials
- Gaps to address for better outcomes
- Patient progress
- Personalized treatment plans
- Actionable steps taken by patients to manage their health (remotely or in-clinic)
Data transparency helps the provider and the patient understand how a condition is progressing and what options can elevate treatment.
5. Advanced Imaging
The development of new technologies has brought on better ways to treat patients. Imaging and neuroscience stand as prime examples of medical trends to pay attention to this year.
Advancements in radiography give medical professionals tools to perform in-depth assessments of the brain after a stroke. Advanced imaging may include:
- 3T MRI
- SPECT scan
- Diffusion tensor imaging (DTI)
These imaging technologies help providers map out a personalized recovery plan and track recovery in post-treatment assessments.
Comprehensive medical programs, such as the Aviv Medical Program, rely on advanced imaging and neuroscience tools like these to improve long-term results for patients.
6. Hyperbaric Oxygen Therapy (HBOT)
Oxygen is the lifeblood of our health. As we age, body oxygen levels decrease, leading to the infamous age-related decline. While many believe these shifts are irreversible, research and clinical trials say otherwise.
Studies indicate hyperbaric oxygen therapy (HBOT), along with other physical and cognitive therapies, can help in the following areas:
At Aviv Clinics, our medical program can include a research-backed HBOT protocol that uses fluctuating oxygen levels, helping to trigger the body’s self-regeneration capabilities.
“By treating vascular dysfunction, we’re mapping out the path toward Alzheimer’s prevention. More research is underway to further demonstrate how HBOT can improve cognitive function and become an influential tool in the imperative fight against the disease.” –Dr. Shai Efrati, Aviv Clinics.

Learn More about the Science of HBOT
We encourage you to lean on Aviv Clinics to learn more about HBOT and other treatment options that can benefit your health.
Our diverse community of patients continues to achieve significant health milestones thanks to a multidisciplinary approach that may include:
- Hyperbaric oxygen therapy
- Cognitive training
- Physical training
- Nutritional coaching
We take a unique approach centered on research, providing high-quality care that produces lasting outcomes.
Health is Wealth: 9 Actionable Ways to Invest in Your Health
The daily choices we make and the activities we engage in all impact our quality of life. Here’s the reality—the average person spends nearly $170,000 on medical expenses in their lifetime. Costs tend to stack up, especially after the age of 65.
While we might consider health problems and expenses the norm as we age, there are ways you can minimize them or even avoid them altogether. Why not start today?
At Aviv, we believe making more conscious decisions today will give you the longevity you deserve. We’re here to get you started on the right foot. Consider these nine ways to start investing in your health today and accruing a healthy ROI immediately!
Note: Speak to your doctor before you pursue any lifestyle changes.
1. Consider the MIND Diet
Eating healthy has always been the mantra over the years, and for good reason—it’s the foundation of feeling good. While there are numerous diet trends out there, there is one truly worth your time and investment—the MIND diet.
Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet is a blend of two highly effective diets:
- Mediterranean: Consists of a heart-healthy eating plan
- DASH: Aims to address hypertension or high blood pressure
Sticking to this diet that entails a variety of fruits and vegetables provides anti-inflammatory and cognitive benefits—it can strengthen brain cell structure and help regulate anxiety and mood.

2. Engage in Intermittent Fasting
We know—fasting doesn’t sound like the most exciting thing. But consider intermittent fasting. Not only can you achieve a healthy body composition, but you can also improve your brain health—all without strict dietary restrictions.
Intermittent fasting is a dietary lifestyle that comprises alternating periods of eating and fasting and limiting the number of hours you consume calories during the day or week.
This metabolic switching:
- Enhances the brain’s ability to resist injury and disease
- Slows down the aging and disease process
- Promotes weight loss
3. Stay Educated on Fall Prevention Tactics
Falls in older adults are common. Conditions that become prevalent as we age (e.g., muscle weakness, osteoporosis, and balance and gait problems) make us more susceptible to falls.
The key ingredient to prevention? Exercise. We’re talking about:
- Strength training
- Cardio training
- Balance training
- Flexibility training
Other fall prevention tactics are just as important. They are:
- Keep your home clear of clutter and trip hazards such as cords, books, shoes, etc.).
- Install grab bars in the bathroom and handrails in the hallways and stairways.
- Avoid wearing clothing that drags on the ground.
- Wear non-slip socks or shoes around the house.
- Take a pause after standing up and before beginning to walk.
4. Find Helpful Ways to Cope with Stress
Stress is inevitable in life, and the body and mind are biologically equipped to handle it. But sometimes, when the stress gets overwhelming, it can negatively impact the brain.
Chronic stress can:
- Kill brain cells
- Cause memory decline
- Negatively impact mental health
Whether you are grieving or dealing with a major change in your life, it’s essential to find healthy coping mechanisms for stress:
- Make time for physical activity: At Aviv, we recommend 30 minutes of exercise three days a week at a minimum. Exercise benefits the brain by releasing endorphins, helping relieve pain, and improving mood. The key is to find an activity you enjoy—this will make exercise fun and feel less like a chore.
- Be conscientious about screen time. Regarding technology and brain health, experts say it’s all about quality vs. quantity. When used wisely, technology offers worthy benefits. But using it improperly can cause more harm than good. Thus, stay aware and focus on balancing screen time with other activities.
- Meditate. Not only is meditation a great activity to do instead of “doom scrolling” on your screen, but meditation may also slow the progression of Alzheimer’s and improve brain focus. Consider meditation apps like Headspace and Calm to get started.
5. Focus on Body Composition Instead of Weight
A low number on the bathroom scale doesn’t necessarily mean all is well. Indeed, society’s obsession with the scale can lead to problems like declining muscle mass—a condition that will do more harm than good later in life.
So toss that unhealthy relationship with the bathroom scale. Instead, look at your overall body composition.
For example, Aviv Clinics uses the seca scale to get a precise rundown of the meaning behind a person’s weight. This scale helps us develop an accurate and customized treatment plan—losing body fat, gaining muscle, or a combination of both.
Speak to your doctor to gain a comprehensive assessment of your body composition so you can make appropriate, personalized goals.
6. Stick to a Consistent Sleep Schedule
Since the sleep hormone melatonin naturally decreases with age, it’s vital to set up healthy sleeping habits. This entails turning off all electronics an hour before bedtime and getting in bed at the same time each night.
Doing so will promote natural circadian rhythms and maintain cognitive health.
7. Engage in Games
Investing in your health doesn’t have to be boring, it can include games!
That’s right, researchers report playing brain games can improve cognitive performance. It’s a fun and active way to shake things up for your brain.
Much like muscles build muscle fibers after exercising, the brain functions similarly—it promotes new neurons and neuronal connections after participating in games.
8. Listen to Music
When was the last time you truly listened to music? What kinds of images and memories did it elicit?
Music offers far more advantages than helping you get through a grueling drive or setting the tone for a party. The best part is these benefits are backed by research.
Studies illustrate music can:
- Have a positive impact on those with memory loss conditions (i.e., Alzheimer’s disease, dementia)
- Reduce anxiety, pain, and blood pressure
- Improve sleep quality and mental alertness
9. Find a Research-Backed HBOT Program
Hyperbaric oxygen therapy (HBOT) is a therapy that has a patient breathe 100% pure oxygen in a pressurized chamber.
Several studies illustrate the potential of HBOT, when administered in a specific protocol, in improving cognitive, physical, and psychological performance. In this protocol, oxygen levels are fluctuated during each hyperbaric session. This system increases oxygen levels in the body up to 20 times higher than normal and boosts your brain’s ability to heal itself.
The unique medical program at Aviv consists of a treatment program that can include this same research-backed HBOT protocol along with cognitive training, dietary coaching, and physical performance training, in a physician-designed program tailored to each client’s needs.
This holistic approach gives each patient the personalized care they deserve for their unique health conditions. Our clients have optimized their athletic performance with HBOT and have found relief from debilitating medical conditions such as stroke and traumatic brain injury.

Invest in Your Health at Aviv
The Aviv Medical Program stands by a holistic treatment program that targets all areas discussed above. A series of independent clinical trials illustrate how our program helps treat the symptoms of different health conditions.
Beyond the Impact: Your Comprehensive Guide to Navigating Delayed Concussion Symptoms
The CDC estimates that “1.5 million Americans survive a traumatic brain injury” every year. However, not all concussion symptoms show up right away. While the brain is a marvelous organ and usually amazes us with its healing capabilities, there are times when our brains need a bit more time and treatment to heal fully.
Post-concussion syndrome is a relatively common complication during concussion recovery. Fortunately, recovery from delayed concussion symptoms is possible even years after a traumatic brain incident.
If you or your loved one believes they have post-concussion syndrome, rest assured the Aviv Clinics team is here to help. We understand how debilitating living with PCS symptoms can be. We also understand how challenging it can be to find answers and solutions.
In this comprehensive guide, you’ll find essential research-backed details to help you better comprehend your condition and the treatment options available to you.
Understanding Post-Concussion Syndrome

At one time, a mild traumatic brain injury (mTBI), which many know simply as a concussion, was thought to be a benign event. With much research, experts now know that even minor injuries to the brain can have significant effects, especially with multiple incidents. These injuries can contribute to adverse neuropsychological outcomes—both acutely and long-term.
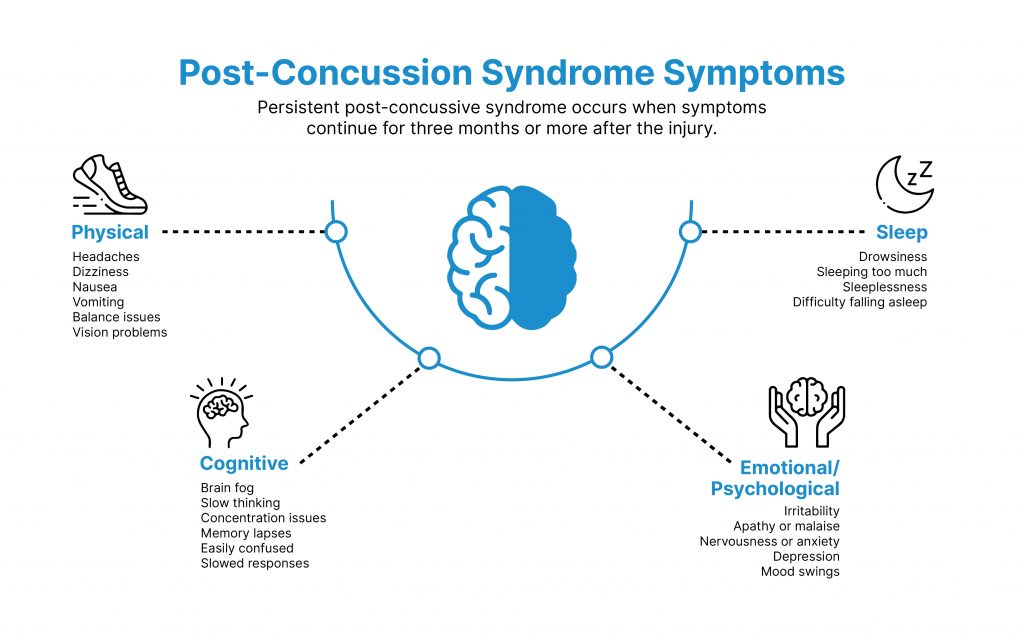
According to Aviv Clinics’ medical team, most concussion symptoms alleviate within about two weeks. When concussion symptoms last or continue to develop over a much longer period, these persistent post-concussive symptoms are known as post-concussion syndrome.
What Is Post-Concussion Syndrome (PCS)?
Post-concussion syndrome (PCS) is a condition where concussion symptoms continue beyond the expected recovery period, often months or even years. PCS occurs from traumatic brain injury (TBI)—a blow or jolt to the head from accidents such as falls, car accidents, and sports injuries. Even a whiplash injury can cause damage to the delicate brain tissue. Mild to severe cases of TBI can lead to PCS.

Symptoms of post-concussion syndrome include a variety of physical, cognitive, emotional, and sleep indicators such as:
- Headaches that won’t go away
- Feeling more exhausted than usual
- Having trouble concentrating and remembering
- Having difficulty falling or staying asleep
A concussion lasting more than three months may result in changes in cognition—whether physical and/or emotional—or sleep.
It is possible to have a traumatic brain injury and not know it. There are over 2.8 million people who sustain a TBI each year in the United States. When a TBI isn’t treated properly or the recovery isn’t complete, post–concussion syndrome can manifest.
What Causes Post-Concussion Syndrome?

When someone experiences a traumatic brain injury, this blow or jolt to the head makes the brain rattle back and forth rapidly within the skull. This can cause shear force trauma to connective blood vessels and cells in the brain. This sudden movement can:
- Disrupt blood flow to specific brain regions
- Trigger chemical changes in the brain
- Stretch and damage brain cells
These activities put stress on your brain and prevent it from functioning normally.
A concussion might cause dizziness, ringing in the ears, blurred or double vision, fatigue, and vomiting in the short term. But over time, that same injury or repeated injuries may contribute to ongoing symptoms. Some people may not even connect an injury that happened years ago with their current symptoms, which can make it difficult to properly diagnose a TBI or post-concussion syndrome.
Can Concussion Symptoms Be Delayed?

While some symptoms surface immediately after a head injury, delayed concussion symptoms are possible due to the complex way the brain responds to trauma. The severity of the injury and the specific areas of the brain affected can influence the timing of symptoms.
Although there isn’t a quick test for PCS, there is ample research and understanding of this condition to help explain the signs and symptoms. A clinical evaluation is warranted for symptoms that linger past the typical timeframe for recovery.
Post-Concussion Syndrome Symptoms
Individuals experience a spectrum of symptoms associated with post-concussion recovery. From persistent pain to cognitive challenges, we can divide the symptoms of post-concussion syndrome into four categories:
1. Physical
Physical PCS symptoms are the most commonly recognized signs. Individuals with PCS may experience debilitating pain and discomfort, such as:
- Headaches
- Dizziness
- Nausea
- Vomiting
- Trouble balancing
- Vision problems
2. Cognitive
Cognitive issues are often the PCS symptoms that compel patients to seek medical advice. Cognitive PCS symptoms include:
- Feeling mentally foggy
- Feeling slowed down
- Having difficulty concentrating
- Having trouble remembering
- Being forgetful of recent information and conversations
- Experiencing confusion about recent events
- Answering questions slowly
3. Psychological/Emotional
Psychological and emotional symptoms can often be difficult to identify and associate with head injuries. Many people tend to overlook these emotional changes when, in reality, these changes can be a manifestation of PCS. These psychological/emotional changes include:
- Irritability
- Sadness
- Nervousness
- Anxiety
- Depression
- More emotional in general
4. Sleep
Last but not least, PCS symptoms can manifest in your sleeping patterns. For example, those with PCS may:
- Feel drowsier than normal
- Sleep more than usual
- Sleep less than usual
- Have trouble falling asleep
Where the damage occurs in the brain also plays a relevant role in the type of PCS symptoms.
For example, when head trauma inflicts damage to the frontal lobe of your brain—the area that manages emotional expression, focus, attention, and memory—this may stimulate emotional/behavioral changes, including “impaired basic and social emotion processing” and cognitive shifts.
While individuals may initially feel relatively okay after a head injury, symptoms can evolve in unexpected ways and even become more pronounced over time. Experiencing delayed concussion symptoms may signal that changes in the brain triggered by the injury just took time to fully manifest noticeable effects.
Why Concussion Symptoms May Be Delayed

Delayed concussion symptoms can occur for several reasons. In an ideal world, you would know what’s happening inside yourself and why. But the reality is the body and mind are complex.
When someone experiences a traumatic brain injury (TBI), this causes physical, metabolic, and chemical changes to the brain. Even if you feel okay and only experience mild effects, this can change later.
Here’s why.
The brain has pathways—think of them as different routes you may take to work. Some roads have more traffic than others. Sometimes, you have to take the long way to get home. Brain pathways work the same way.
Let’s say you get into an accident that causes a head injury. Some brain pathways are damaged and can’t deliver the blood and oxygen supply the brain needs. Fortunately, other pathways and cells can take over to do the job. However, the healthy brain pathways might overcompensate over time for the lack of operating pathways. Your brain grows tired of the extra effort, and delayed concussion symptoms emerge. The evolution of concussion symptoms over time emphasizes the importance of ongoing monitoring and seeking adequate treatment.
Post-Concussion Syndrome: Answers to Common Questions

If you have been relentlessly searching for answers about possible post-concussion syndrome symptoms, we see and hear you. It can be incredibly challenging to not understand what is going on in your body and mind. You can rest assured that the Aviv Clinics’ medical team has answers for you.
How Soon Can Symptoms of PCS Start?
Symptoms of PCS may be an extension of your acute injury or they can start to show weeks after concussion when a concussion or TBI survivor just isn’t getting better. Over time, symptoms may not go away or may exacerbate. Symptoms can also appear later on in life.
How Long Can Symptoms of PCS Last?
PCS symptoms can last anywhere from weeks to years. The sooner you address your symptoms and get help, the more likely you’ll be able to get back to your normal activities and, for some people, return to your typical personality traits. There are risks to waiting too long to treat your post-concussion syndrome, which brings us to our next point.
What Are the Consequences of Waiting Too Long to Treat PCS Symptoms?
PCS symptoms can turn permanent if not addressed soon enough. According to Aviv Clinics’ team of certified physicians, usually, after three months, PCS turns into persistent PCS. And after a year, symptoms of post-concussion syndrome can turn chronic. Keep in mind that it doesn’t matter where or how you receive your head injury—these factors do not necessarily impact the severity of your PCS.
How Does the Brain Recover from a Concussion?
The brain is a powerful organ with incredible self-healing mechanisms. Even if you experienced an accident years ago, there’s still hope for recovery decades later. The key is finding the right treatment program to give the brain a delicate push for unleashing that potential.
Proper medical expertise and protocol can help:
- Encourage neuroplasticity, or the brain’s ability to adapt or react in response to injury or disease.
- Drive neurogenesis or nerve cell regeneration that occurs in the brain.
- Increase blood flow and oxygen in parts of the brain associated with executive function, vision, sensation, and more.
Most patients at Aviv Clinics see tangible progress roughly 8-12 weeks after starting their treatment plan. However, the recovery period varies depending on the severity of your condition, health background, lifestyle, and other factors.
How Long Can You Leave Post-Concussion Syndrome Untreated?
The longer you wait to heal PCS, the more likely your symptoms could become permanent. Dr. Mohammed Elamir, MD, FACP, further explains: “Damaged or injured tissues due to PCS carries a limited window for full recovery.”
Thus, the time to take action is now. If you have experienced an accident or head injury and have not been feeling the same, trust your instinct—take back control of your health by seeking PCS treatment.
What Are the Consequences of Waiting Too Long to Treat PCS Symptoms?
PCS symptoms can turn permanent if not addressed soon enough. According to Aviv Clinics’ team of certified physicians, usually, after three months, PCS turns into persistent PCS. And after a year, symptoms of post-concussion syndrome can turn chronic. Keep in mind that it doesn’t matter where or how you receive your head injury—these factors do not necessarily impact the severity of your PCS.
Thus, staying aware of your body is essential. Speak with a doctor if you feel anything out of the ordinary. As we noted earlier, when concussion symptoms last for over two weeks, that’s your cue to begin seeking a medical consultation.
Diagnosing Post-Concussion Syndrome

Diagnosing post-concussion syndrome involves a comprehensive assessment that examines multiple factors to get a clear picture of the patient’s experience. Obtaining a PCS diagnosis can be complex. Post-concussion syndrome symptoms and severity can vary daily, making the experience sometimes confusing. If you feel anything is off, we recommend reaching out to the experienced team of physicians at Aviv Clinics.
To diagnose PCS, your doctor will carry out a series of exams that may entail:
- Discussing your health and concussion history
- Conducting a physical examination
- Advanced MRI that maps out specific parts of your brain
- SPECT scan that points out blood flow in negatively affected brain areas
- Neurocognitive testing that examines your motor, verbal communication, and memory skills
- Neurological exams that may involve using lights and reflex hammers to assess your nervous system
It’s important to note that post-concussion syndrome is often a diagnosis of exclusion, meaning we must rule out other potential causes of PCS symptoms. The diagnosis can also evolve as symptoms persist or change.
Is There a Specific PCS Test?
While there isn’t one specific test you can take for a PCS diagnosis, and you certainly can’t get a conclusive diagnosis from online information, there are a variety of assessments that physicians can use to determine if you’re dealing with chronic post–concussion symptoms.
The goal of using a variety of evaluations is to ensure your mind and body are being thoroughly evaluated and to rule out any other cause for your symptoms. In addition to reviewing your injury history and monitoring your symptoms, your doctor may perform a combination of any of the above exams to determine if you have PCS.
Even without an easy test, PCS can be diagnosed by a medical professional. Diagnosis is based on a history of head injuries and reported symptoms, as well as a thorough assessment of brain health and function.
Once a physician has thoroughly evaluated you, you’ll be presented with a variety of treatment options for your symptoms.
Treatment for PCS

The good news is various treatments are available to help mitigate your PCS symptoms.
Some facilities depend primarily on cognitive behavioral therapies, which have shown strong results in improving sleep for those suffering from PCS. Others may focus on vestibular therapies for improved balance, psychological interventions for symptoms like depression or anxiety, or neuro-optical therapy for blurred or double vision.
However, in most cases, these treatments only address the symptoms of post-concussion syndrome and not the underlying cause.
Take time to learn more about your treatment options for post–concussion syndrome. Here are treatment protocols you should learn about if you’ve experienced any type of brain trauma. Each method holds unique strengths that may target the specific symptoms you are experiencing.
Vision Therapy
Vision therapy involves a variety of techniques that train your visual system. Those who may benefit from this are people who experience eye pain, vision problems, dizziness, and headaches.
Clinical studies in patients with post-concussion vision issues show that “the vast majority of cases” notice improvement after participating in vision therapy.
Neuro-Optometric Rehabilitation (NOR)
Neuro-optometric rehabilitation (NOR) therapy uses therapeutic prisms, lenses, and filters to stimulate parts of the brain that are not functioning properly. Those suffering from visual injuries and complications may find relief through NOR.
There is growing evidence NOR can enhance “visual skills and reduce visual symptoms” in patients with post-concussion syndrome.
Physical Therapy (PT)
Physical therapy (PT) is a form of care that aims to ease pain and help you move and live better. This may include massage, range of motion stretching, exercises, and heat treatments.
PT may “facilitate recovery and improve function” for those who struggle with physical symptoms of PCS. One small study where participants averaged 7 PT sessions reported that their physical symptoms became more manageable after treatment.
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy (CBT) is a psychological treatment that addresses problems such as depression and anxiety. CBT generally strives to change thinking and behavioral patterns. Studies indicate CBT may be an effective treatment method for “improving depression, anxiety, and social integration” in those with TBI.
Neuropsychology
Neuropsychology is a subset of psychology that focuses on how the brain and nervous system influence your thoughts and behaviors. It takes an educational approach, teaching patients about their minds and engaging in unique exercises.
Neuropsychology may be ideal for those with memory and concentration issues, as well as anxiety and depression. Research notes neuropsychology may play a vital role in helping better understand the link between the area of injury in the brain and their PCS condition and the “severity of concussion and who develops” the syndrome.
Hyperbaric Oxygen Therapy (HBOT)

Hyperbaric oxygen therapy (HBOT) is a treatment method that increases oxygen levels in the brain and body. Here’s how HBOT works:
- Patients enter a room called a hyperbaric oxygen chamber, or suite, and receive treatment for one to two hours.
- In this suite, the air is pressurized higher than normal air levels, allowing 10-15 times more oxygen to be transported through the body
- Patients breathe in 100% pure oxygen via a mask while in the suite.
- Patients keep the oxygen mask on for 20 minutes and then spend five minutes with the oxygen mask off to fluctuate oxygen levels and encourage the body to release its natural healing mechanisms
Studies illustrate that HBOT delivered in this particular, unique protocol “can induce neuroplasticity”—the ability of the brain to modify and adapt based on environmental interactions—essentially rewiring itself, which may:
- Repair chronically damaged brain functions and tissues
- Improve the overall quality of life for patients with PCS
Additional research shows HBOT can significantly improve “memory, executive functions, information processing speed, and global cognitive scores.”
Research in the last two decades notes hyperbaric oxygen therapy (HBOT), in combination with cognitive, physiological, and nutritional training, can lead to significant neurological improvement after a concussion. The Aviv Medical Program is based on this research.
Aviv Clinics Treatment for PCS Symptoms

Many people go to multiple doctors before getting their post-concussion syndrome diagnosis. Due to the complexity of treating PCS, far too many patients receive minimally effective treatments. The results? Often, short-term fixes that don’t provide what you need.
If you’re looking for PCS relief, the Aviv Medical Program can be your answer.
With the Aviv Medical Program, our team of diverse clinical professionals (medical, cognitive, physical, and nutritional specialties) will perform advanced testing to identify exactly what is going on and craft a customized, long-term treatment plan.
- Our program features a group of certified medical professionals focused on your recovery. They will track data on your health and offer individualized solutions to elevate your quality of life.
- Treatment may include a combination of cognitive and physical training, dietary coaching, and HBOT protocols. HBOT can yield multiple positive shifts in the brain, such as new blood vessel formation and stem cell proliferation and differentiation.
The Aviv Medical Program takes a holistic approach that encompasses several of the areas we discussed above. We leverage the expertise of a diverse team of medical professionals based on your health assessment.
Aviv Clinics takes a three-step approach:
- In-depth medical assessment: We start with a comprehensive health assessment with advanced brain imaging exams (perfusion MRI, fMRI, SPECT, etc.). The goal is to attain a holistic and accurate understanding of your mind and body and map a treatment plan to maximize the program’s results.
- Tailored treatment program: The Aviv medical team will craft a personalized treatment program based on your medical assessments. This may entail cognitive and physical training, hyperbaric oxygen therapy (HBOT) sessions, and a nutritional regimen. The goal is to maximize your body’s healing process.
- Post-treatment assessment: The Aviv team will repeat the tests performed in your pre-assessment to measure your progress and make relevant recommendations.
Benefits of our program can include improved:
- Cognitive and motor functioning
- Physical performance (fitness, strength, coordination, balance)
- Immune system
- Stem cell growth (the building blocks of tissue rejuvenation)
At Aviv Clinics, our multidisciplinary medical team of physicians, neuropsychologists, physiologists, physical therapists, dieticians, and more ensures you receive the thorough medical treatment you deserve.
What Is HBOT’s Role in Relieving TBI Symptoms?

Dedicated research into brain healing reveals a therapy that has produced positive results in cases of TBI and post-concussion syndrome. Hyperbaric oxygen therapy (HBOT) has historically been accepted as an effective treatment for medical issues like wound healing, severe burns, and decompression sickness.
However, research in the last two decades reveals that HBOT, can repair areas of the brain that have been damaged due to TBI and concussion, as well as stroke, post-traumatic stress disorder, fibromyalgia, Lyme disease, and other neurological conditions.
What Results Can Individuals Expect?
To understand how studies show HBOT works as a treatment tool intended to address TBI and post-concussion damage, it’s important to know what changes occur in the brain during those injuries. Structural damage indicates a physical impact on the brain, such as bleeding. Metabolic damage is present when the brain’s cells are affected.
Traditional scans like CT and MRI may not be able to detect metabolic damage, especially if an injury occurred years ago. More advanced scans—like functional MRI and SPECT—are better able to identify areas of the brain that may be producing chronic post-concussion symptoms.
Research shows that HBOT and the nutritional, cognitive, and physiological therapies that can be included in the Aviv Medical Program may yield multiple changes in the brain:
- New blood vessel formation (angiogenesis)
- New and stronger neural connections
- Stem cell proliferation and differentiation
These neural, vascular, and cellular changes contribute to cognitive improvements in memory, executive function, attention, processing speed, and spatial memory. Individuals with brain-based motor skill challenges also benefit from this comprehensive therapy.
“HBOT can be successful because it addresses the cause of the symptoms, not just the symptoms alone. In combination with cognitive, physical, and nutritional coaching, some HBOT protocols can be very effective.” —Dr. Mohammed Elamir, MD, FACP
The physiological and nutritional aspects of the customized Aviv Medical Program elicit enhancements such as greater aerobic fitness, higher energy levels, improved sleep, and reduced pain. Overall, individuals report a significant improvement in their quality of life after completing the program.
For more research insights, explore the data and studies conducted by The Sagol Center, the world’s largest hyperbaric research and treatment facility.
Finding Relief: Aviv Clinics Success Stories
It’s easy to feel alone when living through PCS. Hope is here at Aviv Clinics. See how our team of certified medical professionals has helped a variety of individuals with unique health backgrounds get back to optimal health.
Here are two PCS patients who have leveraged Aviv Clinics’ comprehensive treatment program. Both received access to our multidisciplinary team of healthcare specialists and in-depth assessments:
Linden Perry: At just 15 years old, Linden suffered concussions from playing basketball and soccer. Her lingering PCS symptoms left her having balance issues, nausea, headaches, and blurred vision. Upon her customized treatment plan at Aviv Clinics, Linden returned to where she had started, academically and athletically.
Rodger Penley: Rodger suffered from a severe head injury after falling backward and hitting his head. He suffered from persistent and intense headaches and couldn’t walk without any support. After joining the Aviv Medical Program, his headaches disappeared after three days! By the conclusion of the program, Rodger fully restored his autonomy and independence.
Before you pursue any treatment plan, keep three things in mind:
- Speak with a physician first about your symptoms and health history. This can help them gain a comprehensive assessment and provide a personalized treatment plan.
You can speak to an Aviv Clinics physician at the clinic or over a virtual meeting for free.
- Be patient. Finding the right combination of therapies that work for you may take some time, but don’t give up. With the right medical program, you can receive the holistic treatment you deserve and find some relief.
- TBI and concussion can affect everyone of all ages. Thus, there is no standard/solid timeline for recovery. It may take several weeks or more to see improvement.
Aviv’s clinical team helps individuals of all ages and backgrounds win lasting health—the foundation of a good life. Our unique protocol has proven to give patients the vitality, health, and confidence they need to move forward.
Feel Your Best with Aviv Clinics
Post-concussion syndrome is a common complication during concussion recovery. Most individuals with PCS can recover even years after their accident, but finding a comprehensive treatment plan can be challenging. We’re here to get you on the right path.
Good health allows you to focus on the essential and enjoyable areas of your life. The time to invest in your health is now, and the Aviv Medical Program will be with you every step of the way.
If you feel you’ve been experiencing delayed concussion symptoms, contact Aviv Clinics. We’ll put you in touch with our certified team of physicians who can help craft a customized plan to aid in your healing process. Focused on service, safety, and comfort, Aviv Clinics is your first stop in getting back to optimal health and back to life.
Post-Concussion Syndrome Treatment That Works
So you had a concussion. Weeks pass, yet you’re still not feeling quite right. You might even feel your condition has worsened—headaches have become chronic, you feel more tired than usual, and you have difficulty following conversations with friends. The list goes on…
You’re not alone if you’re feeling lingering symptoms of your concussion, after all, it is a traumatic brain injury. While the brain is a marvelous organ and usually amazes us with its healing capabilities, there are times when our brains need a bit more time and treatment to fully heal.
Post-concussion syndrome (PCS) is a common complication during concussion recovery. Most individuals with PCS can recover even years after their accident, but finding a comprehensive treatment plan can be challenging. We’re here to get you on the right path.
Learn what the right post-concussion syndrome treatment entails and how the Aviv Medical Program can help.
What Is Post-Concussion Syndrome?
Post-concussion syndrome (PCS) is a condition where concussion symptoms last longer than normal. PCS occurs from traumatic brain injury (TBI)—a blow or jolt to the head from accidents such as falls, car accidents, and sports injuries. Mild to severe cases of TBI can lead to PCS.
Symptoms of PCS include a variety of physical, cognitive, emotional, and sleep indicators such as:
- Headaches that won’t go away
- Feeling more exhausted than usual
- Having trouble concentrating and remembering
- Having difficulty falling or staying asleep
How Do You Diagnose Post-Concussion Syndrome?
Post-concussion syndrome symptoms and severity can vary daily, making the experience quite confusing. If you feel anything is off, we recommend reaching out to a physician at Aviv Clinics.
To diagnose PCS, your doctor will carry out a series of exams that may entail:
- Discussing your health and concussion history
- Conducting a physical examination
- Advanced MRI that maps out specific parts of your brain
- SPECT scan that points out negatively affected brain areas
- Neurocognitive testing that examines your motor, verbal communication, and memory skills
- Neurological exams that may involve using lights and reflex hammers to assess your nervous system
How Is Post-Concussion Syndrome Treated?
We understand obtaining a PCS diagnosis can be stressful. Rest assured, there are treatment options available. These options may be combined to maximize your recovery.
- Cognitive behavioral therapy (CBT): CBT is a psychological treatment that aims to change your thinking and behavioral patterns.
- Studies report PCS patients (who have had mild/moderate TBI) experience improvements from their CBT program.
- Additional studies show a combination of CBT and SSRIs has the potential to improve symptoms in PCS patients.
- Cognitive rehabilitation therapy (CRT): CRT encompasses a group of therapies that strive to restore cognitive (attention, memory, speech, etc.) balance after a brain injury. CRT includes therapies such as neurofeedback and attention processing training (APT).
- Research indicates CRT can teach patients long-term skills that help restore their cognitive abilities.
- Hyperbaric oxygen therapy (HBOT): HBOT is a therapy process that increases oxygen levels in the body. Patients breathe in 100% pure oxygen via a mask in a suite. The air in the suite is pressurized 10–15 times higher than normal oxygen levels.
- Clinical studies illustrate that HBOT may encourage the brain to change and adapt in a way that improves PCS even years after sustaining the TBI.
- Other research reports patients suffering from PCS symptoms showed better thinking/cognitive performance after HBOT.
According to Dr. Mohammed Elamir, MD, FACP: “HBOT can be successful because it addresses the cause of the symptoms, not just the symptoms alone. In combination with cognitive, physical, and nutritional coaching, some HBOT protocols can be very effective.”
The Aviv Medical Program for PCS
Many people go to one or more doctors before getting their diagnosis. Due to the complexity of treating PCS, far too many patients receive minimally effective treatments. The results? Short-term results that don’t provide what you actually need.
With the Aviv Medical Program, we assure you that our team of diverse medical professionals (cognitive, physical, and nutritional specialties) will carry out advanced testing to identify exactly what is going on and craft a customized, long-term treatment plan.
- Our program entails a group of certified medical professionals focused on your recovery. They will track data on your health and offer individualized solutions to elevate your quality of life.
- Treatment may include a combination of cognitive and physical training, dietary coaching, and HBOT protocols. HBOT yields multiple positive shifts in the brain, such as new blood vessel formation and stem cell production.
Case Studies
Here are two PCS patients who have leveraged Aviv’s comprehensive treatment program. Both received access to our multidisciplinary team of healthcare specialists and in-depth assessments:
- Linden Perry: At just 15 years old, Linden suffered concussions from playing basketball and soccer. Her lingering PCS symptoms left her having balance issues, nausea, headaches, and blurred vision. Upon her customized treatment plan at Aviv, Linden got back to where she was academically and athletically.
- Clarissa Rainey: This horseback riding champion experienced a concussion in a car accident. Clarissa experienced memory issues, which made her job challenging and frustrating. After her state-of-the-art treatment at Aviv, she reports that she is much more focused, has clearer thinking, and sleeps better. Not to mention, she is still riding horses and engaging in daily activities to the best of her ability.
How Long Can You Leave Post-Concussion Syndrome Untreated?
The longer you wait to heal PCS, the more likely your symptoms will become permanent. Dr. Mohammed Elamir, MD, FACP, further explains: “Damaged or injured tissues due to PCS carries a limited window for full recovery.”
Thus, the time to take action is now. If you have undergone an accident and have not been feeling the same, trust your instinct—take back control of your health by seeking PCS treatment.
Learn More about the Aviv Medical Program
It’s easy to feel alone when living through PCS. Hope is here at Aviv Clinics.
Backed by over a decade of research, the Aviv Medical Program will be with you every step of the way during your PCS recovery journey. We’ll introduce you to our team of medical professionals who will ensure your recovery is around for the long haul.
How Hyperbaric Oxygen Therapy for TBI Can Help Ease Psychological Changes After a Brain Injury
Every year, 1.5 million Americans suffer from a traumatic brain injury (TBI), which can include mild TBIs or concussions.
A TBI can trigger various changes beyond the physical effects. Several “invisible” or emotional symptoms often lie beneath the surface, causing significant struggles among those suffering from TBIs.
These psychological impacts are harder to pinpoint. Thoughts, feelings, and emotions are complex, intangible processes. There isn’t necessarily one remedy that will resolve long-lasting psychological effects.
If you have sustained a TBI and have been experiencing behavioral and emotional shifts like depression, anxiety, or irritability, you are not alone. The good news is that hyperbaric oxygen therapy (HBOT) can provide genuine results when used with other treatments. And the Aviv Medical Program carries the data to prove it.
Keep reading for all the key details on using hyperbaric oxygen therapy for TBI and how it can help ease psychological changes after a brain injury.
What Happens to the Brain When You Have a TBI?
Psychological changes can occur when the brain’s frontal lobe sustains damage, whether caused by a sports injury, a fall, or an accident. This region of the brain manages emotions and personality traits. After a TBI, an individual might begin acting differently, have uncharacteristic emotional outbursts, and other side effects.
Since blows to the head often cause more severe TBIs, another side effect may be amnesia, which can spare the patient the traumatic memories of the incident.
6 Common Psychological Effects Associated with a TBI
Often, patients and their loved ones don’t realize their behavioral and emotional shifts are the result of a brain injury. Symptoms can materialize days or weeks after the original trauma. Blows to the head may also cause amnesia of the event, which can also make it difficult to connect a head injury with psychological effects.
A lack of understanding makes navigating psychological changes even more difficult. However, there are six common signs you can watch for.
1. Anxiety
Anxiety is common in those with moderate-to-severe TBI. It manifests differently for everyone, but most people experience worry and fear.
Anxiety can also show in physical ways, causing symptoms like:
- A racing heart
- Rapid breathing
- Sweating
- Shaking
Certain events/activities might also trigger anxiety, including:
- Large social situations (e.g., being in a crowd)
- Sudden or unexpected changes in plans
- Feeling rushed
- Situations that merit fast thinking or a lot of attention
2. Depression
Depression involves feelings of sadness, grief, and worthlessness. These emotions might make you:
- Feel tired or frustrated more than usual.
- Experience changes in sleep and eating patterns.
- Withdraw from friends and family.
- Feel less joy from favorite activities.
- Show aggressive behavior (67% of first-time TBI patients sought treatment within three months for aggression).
3. Mood Shifts
Emotions can be difficult to manage after a TBI. Depending on the impact, TBIs can change how you feel or express emotions. For example:
- You might be full of excitement or joy one moment, followed by feelings of devastation or sadness the next.
- You might have unpredictable moments of laughing or crying—emotional expressions that have nothing to do with what you’re feeling or what’s happening around you.
- You might exhibit childlike or aggressive behaviors after a brain injury, potentially having emotional outbursts or feelings of impulsiveness.
4. Paranoia
The average onset of paranoia occurs four to five years after a TBI. Paranoia causes people to become unusually defensive, often believing they’re under threat when little to no evidence of an actual threat exists.
Other signs of paranoia include:
- Trouble admitting faults
- Detachment or social isolation
- Doubting the loyalty of others
- Holding grudges
5. Personality Disorders
Some people may develop personality disorders after TBIs. A personality disorder is a mental health condition involving disruptive thinking and behavior patterns.
Someone with a brain injury and narcissistic personality disorder may have an inflated sense of self-importance and an excessive need for admiration. Roughly one in 10 patients with TBI show symptoms of a personality disorder.
6. Executive Dysfunction
Executive dysfunction is a behavioral symptom that makes it challenging to manage thoughts, emotions, and actions. Symptoms might include:
- Having trouble paying attention
- An inability to prioritize tasks
- An inability to plan for and remember future events (i.e., always being late to events/activities)
- Having difficulty analyzing and/or processing information
- Exhibiting poor judgment
- Struggling to make decisions
These symptoms can cause frustration, adding to the mental health challenges outlined above.
7. PTSD and ADHD
Overlap between TBI and the effects of PTSD and ADHD exists, with studies showing that:
- Children with severe TBI carry a higher risk for ADHD.
- Those with a mild TBI are more likely to develop PTSD than patients experiencing moderate-to-severe TBI.
Developing PTSD from an accident can complicate the TBI recovery process. The injury may inhibit their ability to experience emotional closure after the traumatic event.
Could I Have a TBI and Not Know It?
Yes, it’s possible to have a TBI and not know it. Brain injuries are more common than people realize, and some cases of TBI are never accurately diagnosed. Some of the reasons behind missed diagnoses include:
- Mild, random, or generic symptoms that don’t accurately manifest the severity of the injury
- Remaining conscious after an injury, resulting in the patient feeling like the injury wasn’t severe enough to seek medical treatment
These points cause many to dismiss the notion of getting a CT scan or MRI, which is the first and most vital step in detecting structural damage to the brain. More advanced assessment tools, such as functional MRIs or SPECT scans, can also detect:
- Metabolic damage in the brain tissue
- Brain cells that don’t function properly
Elevate the Quality of Your Life with TBI Rehabilitation
Your TBI and its effects do not have to be permanent fixtures in your everyday life. TBI rehabilitation programs have proven effective, offering relief for those who have struggled with the impact of this type of injury.
An effective TBI rehab plan often involves hyperbaric oxygen therapy (HBOT) in combination with cognitive, nutritional, and physiological protocols. Research illustrates these collective methods work well in repairing areas of the brain after a traumatic brain injury or concussion.
Aviv Clinics’ HBOT protocol involves an oxygen suite where multiple patients can sit in comfort and breathe 100% pure oxygen through a mask. Medical staff members adjust the oxygen fluctuation levels to trigger the self-regenerative mechanisms of the brain and body.
The Aviv Medical Program, which can include this unique protocol, can yield multiple changes in the brain, including:
- Blood vessel formation (angiogenesis)
- New and stronger neural connections (shows promise in healing anoxic brain damage)
- Stem cell proliferation
TBI Survivor Stories
Studies illustrate TBIs are detectable and treatable even years after they occur. With Aviv’s personalized therapy programs that can include effective HBOT protocols, patients have experienced structural brain improvements that enhance their psychological health and overall quality of life.
These TBI survivor stories speak for themselves:
- Clarissa Rainey – Avid horseback rider and champion Clarissa had memory issues after a car accident. Learn how Aviv helped her get back to optimal health and back in the saddle.
- Linden Perry – Having undergone multiple sports concussions, 15-year-old Linden turned to Aviv to regain her health and performance. Find out how her customized treatment plan gave her more confidence to thrive academically and athletically again.
Our Florida Traumatic Brain Injury Program Offers Hope
If you or your loved one has experienced psychological changes from a TBI, reach out to a TBI rehab clinic. Aviv Clinics has a diverse medical team to help individuals enhance and nurture their brains and bodies. The results? Fewer limitations and a happy and healthy life. Contact our team today.
The Stroke Recovery Timeline: 5 Support Stages of Recovery
Last Update: 21 February 2024
The brain is a powerful yet delicate organ we often take for granted. Every thought, movement, and feeling we experience is thanks to the brain. So when these significant capabilities are suddenly stripped away by a stroke, the emotional and physical turmoil runs deep.
Each year, over 795,000 people in the U.S. have a stroke. And up to 50% of stroke survivors suffer motor dysfunction or brain impairment, which may include memory loss and challenges in focusing and processing information.
The stroke recovery timeline is unique for each individual. If these experiences emulate what you have been going through, the Aviv Clinics team is here to offer research-backed guidance on your road to recovery. Health is the most crucial element in your life. The time to commit to it is now.
Below you’ll find information on the impact a stroke has on your body and the five stages of stroke recovery. The intention? Ensuring you find a customized medical program to help you get back to optimal health.
What Happens to the Brain During a Stroke?
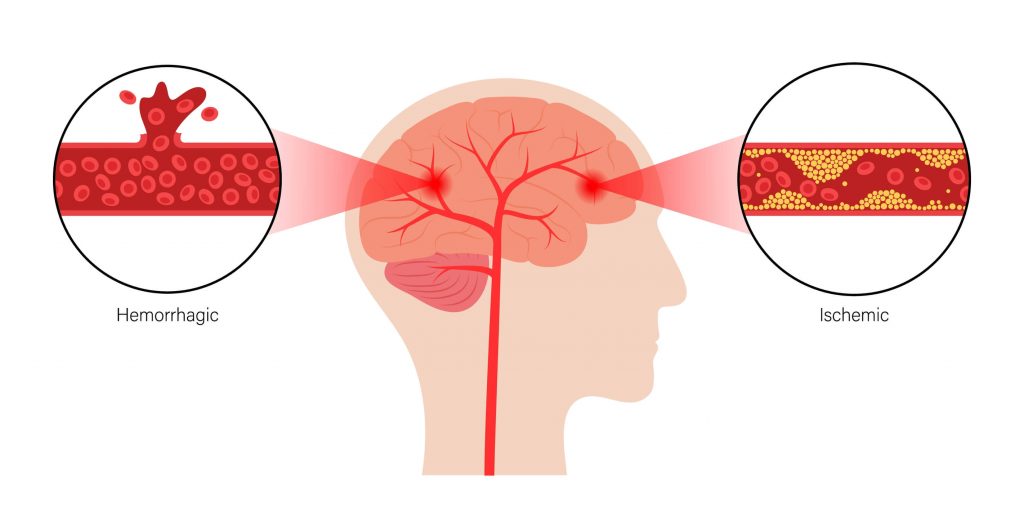
When a stroke occurs, blood cannot get to parts of the brain, meaning oxygen and nutrients cannot adequately nourish brain cells. This can happen in two ways:
- Arteries become blocked (an ischemic stroke)
- Arteries break/rupture (a hemorrhagic stroke)
In either case, a stroke damages areas of the brain. These impacts can manifest in cognitive, physical, and even emotional symptoms.
The Brain After a Stroke – The 5 Support Stages of Stroke Recovery
Studies illustrate the brain can reorganize and adapt in response to injury. But this process isn’t as clear-cut as you’d hope.
The reality is each person carries unique symptoms and medical histories. The timeline for stroke recovery is inherently diverse. So finding a clinic that can offer a customized post-stroke recovery plan is key. The right treatment plan will include one or a combination of these post-stroke rehab therapies.
The good news: The Aviv Medical Program provides a post-stroke recovery treatment program that can combine cognitive, physical training, dietary coaching, and Hyperbaric Oxygen Therapy sessions, even years after the incident. It is never too late to enhance your recovery.
Stroke Recovery Timeline
Though the journey is different for every survivor, each step along the stroke recovery stages timeline represents progress.
You or your loved one will progress through the stroke recovery timeline at an individual rate. While there is no fixed, standard timeline, the stages for improvement generally follow a sequence. Here is an overview of the stages of stroke recovery.
1. Acute Stroke Stage (0-72 Hours)
Immediately after a stroke, the patient receives urgent medical care focused on identifying the cause, stabilizing the patient, and preventing further damage. Medications and procedures to address the cause may be needed. If the stroke is severe, the patient may require emergency intervention.
At this stage, a rehabilitation plan is typically set in motion. This involves meeting with several different providers to make up a comprehensive care team, including neurologists, physical therapists, speech-language pathologists, and occupational therapists.
2. Subacute Stroke Stage (The First 3 Months)
During this stage, care is focused on regaining function and preventing complications. After the patient is discharged from the hospital, their stroke recovery plan at home or a rehabilitation center begins.
It’s during this period that patients often see the most improvement. Patients may receive physical, occupational, speech, and cognitive rehabilitation therapy and training. Depending on their needs, these therapies continue in outpatient centers or through home-based care. It’s typical for a stroke survivor to engage in multiple therapy programs one at a time or simultaneously as their support needs require.
The “risks of recurrent stroke are highest early after the first stroke.” Because of this, this stage also includes risk mitigation and regular monitoring for signs of a second stroke.
3. Early Stroke Recovery Stage (3-6 Months)
Rehabilitation efforts continue. During this period, patients can make significant progress with noticeable improvements. Some patients complete one or more programs, or may focus on home-based therapies rather than outpatient programs.
However, keeping up with a rehabilitation program is key in this stroke recovery stage and beyond due to the increased risk of another stroke. Ongoing care and support can help with the restoration of cognitive, emotional, physical, and behavioral functioning. Rehabilitation programs may be adapted as the patient relearns skills and their rehab needs change.
4. Intermediate Stroke Recovery Stage (6 Months to 1 Year)
Depending on the patient’s needs and challenges, some stroke survivors may complete therapy programs and experience a return to independence in one or more areas. Others will continue with rehabilitation programs on their road to recovery. In either case, stroke recovery is an ongoing process.
During this stage, progress may slow down, which can be frustrating for the survivor and their loved ones. However, improvement is still possible after these plateaus, particularly if rehabilitation efforts continue. Setting new goals and adding variety to a therapy program may help overcome these plateaus.
5. Ongoing Stroke Recovery Stage (1 Year and Beyond)
Post-stroke recovery can continue for years. It’s difficult to predict the success of therapies and how soon a patient can see improvements. Recovery takes time, and ongoing care is crucial for any stroke survivor.
However, major gains in function and independence can occur even years after a stroke. With ongoing therapy and lifestyle support, some individuals see improvements well beyond the one-year mark, especially with proper stroke-supportive therapies.
Ultimately, the rate of recovery depends on the severity of the stroke, the individual’s health, and the effectiveness of rehabilitation programs. Improvement may take longer for some patients, but remember: every positive milestone is one more step along the journey.

5 Support Stages of Stroke Recovery
1. Thinking, Memory, and Perception Training
Thinking, memory, and perception are vital in day-to-day communication and activities. Not to mention, they are what makes each of us creative and unique. So when up to half of stroke survivors experience cognitive impairments, addressing them is critical.
This is where a neuropsychologist can step in. Neuropsychologists assess the connection between someone’s brain and their potential to participate in daily activities.
Neuropsychologists typically begin with an assessment that measures memory, learning, and processing speed. They then use this data to craft a rehabilitation plan.
As one of the most vital stroke recovery stages, this process not only identifies areas for improvement but also paves the way for a personalized journey to cognitive recovery.
2. Communication and Language Training
Human connection plays a vital role in happiness and good health. It’s what helps us build empathy and relationships. So when this is taken away via aphasia—a disorder that affects your ability to understand or express speech—communicating and connecting with loved ones becomes challenging.
Stroke patients with aphasia are often referred to speech-language pathologists (SLPs). SLPs help individuals relearn communication and language techniques such as:
- Controlling mouth/throat muscles
- Engaging in cognitive language exercises
- Pronouncing specific words
- Formulating sentences or expressing information
Studies illustrate early speech intervention often leads to improved communication skills within a 12- and 26-week timeframe. These findings offer hope and reinforce the transformative impact of prompt intervention in the earlier stages of stroke recovery.
3. Exercise and Mobility Training
Those undergoing physical challenges may work with a physical therapist (PT) who helps them relearn and regain physical activities.
Exercise and mobility training with a PT may include:
- Movement exercises such as walking, sitting, standing, lying down, and switching from one type of movement to another
- Balance and breathing techniques
These help patients reacquire motor skills and return to their daily routines. Studies show consistent PT minimizes the risk of hospital readmission among post-stroke patients. As stroke survivors work with a PT to reacquire motor skills, they can reclaim their physical abilities and rebuild their sense of autonomy and independence.
4. Nutritional Training

Research notes that “of the factors that increase the risk of stroke, the worst is diet.” Guided support in this area enables stroke survivors to navigate the unique concerns they may experience. Nutritional training can be beneficial in post-stroke recovery for the following reasons:
- Some patients are unable to swallow well after a stroke. Their appetite might also diminish. These conditions can impact patients’ weight and nutritional intake.
- Patients may have physical issues (for example, being unable to control their arms and/or hands) that make eating and drinking difficult.
Dieticians can address those concerns and provide recommendations based on your needs to:
- Improve your health
- Minimize the risk of having another stroke
5. Hyperbaric Oxygen Therapy (HBOT)
Decades of research prove the benefits of using HBOT in post-stroke recovery. HBOT is a therapy process where patients are prescribed time in an oxygen chamber, breathing in 100% oxygen.
HBOT boosts oxygen in the body and promotes brain cell rehabilitation, which can result in:
- Regained speech
- Recovered ability to read and/or write
- Restored motor function
- Return to independence in performing daily activities
HBOT offers a profound pathway toward regaining important functions by supporting cellular rejuvenation. By tapping into the body’s natural healing potential, HBOT (as part of the Aviv Medical Program) harnesses the body’s capacity for recovery.
Post-Stroke Recovery: 4 Tips to Keep in Mind
To ensure the most successful post-stroke recovery, stay mindful of the following:
1. Consider that Recovery Is Different for Everyone
What recovery looks like and how long it takes is different for everyone due to reasons such as:
- Where in the brain the stroke happened
- How much of the brain was affected
- The survivor’s will and motivation to get better
- The level of caregiver support
- The quantity and quality of the recovery program
2. Repetitive Practice Is Key
“Carefully directed, well-focused, repetitive practice” is key to any neurorehabilitation program. It’s the same concept as if you were to learn a new skill like a musical instrument. Repetitive practice effectively retrains your brain.
3. Recurrent Stroke Prevention Should be Approached with Vigilance
Patients and healthcare professionals should be especially vigilant in preventing another stroke—roughly one in four stroke patients have had a stroke in the past.
Stroke prevention requires:
- Starting treatment right away
- Keeping the following conditions under control, as they can put you at higher risk for another stroke:
- High blood pressure
- Heart disease
- High cholesterol
- Diabetes
4. Measuring Progress Matters
The type of therapy and frequency are important factors to consider during recovery. Working with a medical staff that captures and tracks data is critical to your success.
For example, the Aviv Medical Program tracks analytics to provide a detailed report of your health and progress.
The information gathered from a variety of scientifically-advanced analytical tools (including an in-depth high resolution MRI of your brain stroke) allows our clinical team to make customized adjustments and give you precisely what you need to elevate the quality of your life.
Post-Stroke Recovery: 2 Key Signs of Healing
If you find your post-stroke recovery journey is slightly different, don’t stress about it. Everyone is different; thus, timelines and progress will vary. Regardless, there are two signs of recovery you can expect:
- There is improvement within three months and beyond: Although everyone recovers at a different pace, the first three months are generally when patients see and feel the most improvement. That’s why it’s more effective to begin a stroke recovery program quickly.
- Independence is improving: After a stroke, you may depend on others to help you carry out daily tasks such as getting dressed, bathing, or eating. With the right post-stroke treatment plan, you’ll start to rely less on others and perform those tasks independently again.
Stroke Recovery Story: Keren Trabelsi
A holistic treatment plan that addresses the mind and body is key to successful recovery. It offers a more effective and long-term recovery plan. Former Aviv Clinics patient Keren Trabelsi is a true testament to this.
Keren underwent an ischemic stroke, causing paralysis on the left side of her body. Also, cognitive issues made daily tasks difficult, which did not make her feel as capable as she had been before. Fortunately, Keren found the Aviv Medical Program. Aviv provided a personalized treatment plan that encompassed many of the phases discussed above. Thirteen months later, she can walk comfortably, type with her left hand again, and engage in cognitive activities (i.e., crossword puzzles, Sudoku, etc.).
“[The Aviv Medical Program is] like driving a Ferrari on the road to recovery versus driving like an old beaten-up car….”
Watch Keren’s post-stroke recovery story:
Stay educated on stroke by joining our on demand webinar.
Recovering After a Stroke: Is it ever too late?
Seek Stroke Treatment in Florida
Our team proudly assists a variety of clients, crafting an individualized plan for each patient.
If you or your loved one has undergone a stroke, contact Aviv Clinics. We’ll put you in touch with our medical team, who conducts the best stroke rehab center in Florida.



