pTau Testing for Alzheimer’s Risk: What It Is, Why It Matters, and How Aviv Clinics Can Help
pTau Testing for Alzheimer’s Risk: What It Is, Why It Matters, and How Aviv Clinics Can Help
As the years progress, it’s common for us to become more aware of occasional memory lapses or moments of forgetfulness. But when do these minor gaffes become a cause for concern? At Aviv Clinics, we believe in the power of proactive aging, and we’re proud to introduce walk-in pTau-217 testing for Alzheimer’s risk to our many brain health offerings. This groundbreaking blood test can help assess your risk for developing Alzheimer’s disease, even before symptoms appear.
With Alzheimer’s disease affecting nearly 7 million people in the United States alone, you may be curious if pTau testing is right for you. Here’s what you need to know about pTau testing at Aviv Clinics, and how it can fit into a comprehensive plan to protect your brain health.
What Is pTau?
Phosphorylated tau, or pTau, is a protein found in the brain. In healthy brains, tau proteins can help stabilize the structure of neurons, or nerve cells. But in the early stages of Alzheimer’s disease, tau becomes abnormally phosphorylated, forming tangles that disrupt communication between brain cells.
Although pTau isn’t considered a direct cause of Alzheimer’s disease, high levels of pTau in the blood are now recognized as one of the most accurate indicators of early Alzheimer’s disease. Elevated pTau levels are correlated with brain atrophy, cognitive decline, and accumulation of amyloid plaques.
Importantly, the presence of elevated pTau does not confirm a diagnosis of Alzheimer’s but suggests an increased likelihood of associated brain changes.
Why Aviv Clinics Offers pTau Testing
Until very recently, detecting Alzheimer’s pathology in the brain required invasive spinal taps or expensive PET scans. The recent development of blood-based biomarkers like pTau has transformed early detection, offering a faster, simpler, and more accessible path to answers.
While pTau-217 testing is not yet FDA-approved as a standalone diagnostic tool, emerging research shows its strong potential to aid in early risk assessment for Alzheimer’s-related pathology. At Aviv Clinics, we offer this test as part of a broader approach to brain health for individuals interested in gaining early insights, especially those with risk factors or mild cognitive symptoms.
Research published in January 2024 noted that commercially available pTau-217 testing showed “high diagnostic accuracy.” In their analysis, pTau tests outperformed all other blood-based biomarkers in predicting amyloid and tau status.
How Accurate Is the pTau Test Compared to Other Alzheimer’s Tests?

The pTau blood test offers comparable accuracy to other tests available. Additionally, tests that measure pTau provide an early glimpse into changes in the brain that may be happening silently.
Although traditional cognitive screening tests can reveal signs of dementia or Alzheimer’s disease, these are typically not performed until a patient begins to experience preliminary symptoms. However, our bodies can show elevated levels of pTau-217 more than 20 years prior to the onset of Alzheimer’s disease symptoms.
The pTau blood test has comparable accuracy to spinal fluid analysis and PET scans. Unlike these complex tests, however, it only requires a simple blood draw to perform.
Despite these strengths, it is important to recognize that no test is perfect. Conditions like chronic kidney disease, stroke, and myocardial infarction can also increase pTau levels, potentially leading to false-positive results. For those with high pTau levels, further evaluation and testing are required to confirm their source.
While early results are encouraging, clinical interpretation should always be done in context and in consultation with a trained healthcare professional. At Aviv Clinics, our physicians will carefully review your pTau results with you, provide clear answers, and tailor any recommended follow-up to your specific needs.
Who Should Consider a Walk-in pTau Test?
The pTau-217 test is ideal for individuals who meet one or more of these criteria:
- Are age 60 or older
- Have a family history of Alzheimer’s or dementia
- Are experiencing subtle or unexplained cognitive changes
- Want a baseline assessment of their brain health
This test is not currently approved as a screening tool for the general population and should be interpreted as part of a larger clinical picture.
What to Expect When You Get a pTau Test at Aviv Clinics

The process of pTau testing at Aviv Clinics is simple:
- Pre-Testing: You don’t require an appointment or have to fast before pTau testing at Aviv. However, as with many blood tests, you should not take biotin supplements for a minimum of three days before your blood draw. If you take a daily multivitamin, please check its ingredients to determine if it contains biotin.
- Blood Draw: A simple blood sample is taken during your walk-in testing visit at our clinic at The Center for Advanced Healthcare in The Villages®.
- Analysis: Your sample is sent to a certified laboratory and tested for pTau levels.
- Results: After approximately 10 days, one of our board-certified physicians will review your test results with you and discuss and what steps, including lifestyle interventions, you can take next to preserve your brain health.
What Happens After You Get Your pTau Results?
Our physicians will evaluate your results in the context of your full medical history. Depending on your results, they may recommend further imaging or cognitive testing when indicated.
Your results are just the beginning. Whether your pTau levels are elevated or normal, we’ll help you:
- Understand your current brain health profile
- Identify lifestyle risk factors
- Determine whether additional assessments are appropriate for a more in-depth evaluation
- Explore personalized interventions, including the Aviv Medical Program, which can be tailored to address your cognitive performance.
Why Early Detection Matters: The Aviv Clinics Approach
Blood-based biomarkers like pTau are the next frontier in Alzheimer’s research and prevention. Aviv Clinics is proud to be part of this future by offering cutting-edge tools that empower individuals to take charge of their brain health.
The earlier you understand your cognitive health, and the more options you have for both prevention and treatment. If testing reveals that your pTau levels are elevated, you may be a candidate for more advanced cognitive assessments, targeted brain health therapies, or ongoing monitoring to track changes over time. You may consider lifestyle modifications like dietary changes, physical activity, and stress management. These factors, and others, can have a direct impact on your brain health.
For those looking to take a more proactive approach, Aviv Clinics offers comprehensive, personalized programs designed to enhance brain performance. Our clinical team will create a custom Aviv Medical Program based on your test results, physiology, medical history, and personal goals. Your tailored plan may include a combination of evidence-based interventions such as:
- Our unique hyperbaric oxygen therapy protocol
- Cognitive exercises
- Nutritional counseling
- Physical training
- Other therapies as prescribed
If testing reveals that your pTau levels are within normal range, you’ll have a valuable baseline to compare against in the future.
Either way, this test allows you to take charge of your cognitive health today — when you can work towards making a meaningful difference. Early identification of at-risk individuals, particularly those with mild symptoms or risk factors, can help tailor effective interventions.
At Aviv Clinics, pTau testing is used as part of an integrative approach rather than a standalone diagnosis.
Is pTau Testing Covered by Insurance?
At this time, pTau-217 testing is not covered by Medicare, Medicaid, or private insurance. This means the cost of these tests is typically out-of-pocket. However, patients with a Health Savings Account (HSA) or Flexible Spending Account (FSA) may be covered if deemed medically necessary. If you have an HSA or FSA, we recommend you contact your plan administrator and inquire about coverage.
How Much Does pTau Testing Cost?
Aviv Clinics offers pTau-217 testing for $350 on a walk-in basis, making this advanced biomarker test both accessible and affordable. Unlike testing conducted at clinical laboratory services, this cost also includes physician interpretation of your results.
When certain conditions apply, pTau testing may qualify as a tax-deductible expense in the United States. Consult your tax advisor for more information about deductible medical expenses.
Are you interested in pTau testing as part of a broader evaluation of your cognitive health? Contact our team for details.
Take the Next Step
If you’re an older adult and starting to think more seriously about your brain health, you’re not alone. Fortunately, with cutting-edge tools like pTau testing, Aviv Clinics empowers you to take control of your cognitive health, now and in the future.
Whether you’re concerned about memory changes, have a family history of Alzheimer’s, or want a clearer picture of your brain health, our team is here to help.
Call Aviv Clinics at 352-492-6634 or reach out through our contact form to learn more, or stop by our clinic in The Villages between 8:00 AM and 4:00 PM, Monday through Friday for your walk-in pTau blood test.
Your brain deserves a proactive plan. Aviv Clinics is ready to help you build it.
Could You Have Undiagnosed Mild Cognitive Impairment?
“More Than Seven Million Americans Have Undiagnosed Mild Cognitive Impairment.”
This was the alarming headline from the University of Southern California that unveiled the results of two recent studies on mild cognitive impairment (MCI). The first study, which was published in July 2023 in Alzheimer’s Research and Therapy, revealed that “7.4 of 8 million (92%)” of Americans with MCI, a common precursor to dementia and Alzheimer’s disease, may be unaware that they have the condition.
Even more concerning, the second study, published three months later in The Journal of Prevention of Alzheimer’s Disease, estimated that 99% of physicians are underdiagnosing MCI—“Only 0.1% of clinicians and practices had diagnosis rates within the expected range.”
But what is mild cognitive impairment, and what is the result of typical aging? Join us as we explore the symptoms, causes, and what you can do.
How Fast Does Mild Cognitive Impairment Progress?

While MCI doesn’t automatically lead to dementia, early detection is still crucial. According to the Alzheimer’s Association, within five years of diagnosis, as many as one in three MCI patients will develop dementia. Identifying MCI early allows for exploring potential treatment options and making important legal and financial arrangements for their future care.
At Aviv Clinics, we see people every day who are experiencing mild cognitive impairment. While some are diagnosed beforehand, many come to our clinic because they suspect something is amiss. If you find yourself in either of these groups, I’d like to take this opportunity to delve deeper into mild cognitive impairment treatment.
Mild Cognitive Impairment Symptoms and Diagnosis

Determining if a patient has MCI can be challenging for several reasons. Biological aging causes changes to our brain tissue and cognitive function, so patients may dismiss mild confusion or memory loss as just a consequence of growing older rather than exploring the potential diagnosis of MCI.
Second, mild cognitive impairment symptoms are inconsistent. It may be challenging to determine when symptoms indicate mild cognitive impairment vs. dementia, Alzheimer’s disease, or various other cognitive and mental health conditions. In addition to memory loss, MCI can manifest with the following symptoms:
- Difficulty making decisions
- Attention issues
- Language problems
People with MCI might also have symptoms of depression, irritability, anxiety, or apathy. To learn more about some of the indications of mild cognitive impairment, read our blog, “Signs and Symptoms of Cognitive Decline.”
Third, physicians don’t always closely assess brain health, especially if a patient has arrived for another reason. Researchers found that:
- A typical doctor’s visit lasts only about 17 minutes on average.
- During these appointments, numerous health concerns may be discussed. Of these, “topics each received 1.1 minutes” of total discussion.
For older adults, cognitive health may take a backseat to diabetes, high blood pressure, or other age-related concerns during a visit to the doctor.
Finally, the stigma surrounding cognitive impairment may cause people to hide symptoms. Nobody wants their loved ones to think they’re losing their mental acuity, and many older adults fear losing their independence. Consequently, they may withdraw from social interactions or make excuses for cognitive gaffes.
Measuring Cognitive Changes
How fast does mild cognitive impairment progress and become a diagnosable medical condition? Cognitive decline can manifest slowly. It may begin as occasional forgetfulness or trouble staying focused and start to interfere with one’s day-to-day functioning subtly over time, although it may be dismissed as part of the normal aging process.
For others, the decline can happen more rapidly. It is normal for cognitive processes to slow down when a person is in their 60s and 70s, but there is no standardized rate. The rate of decline varies greatly from person to person.
However, when you start to notice changes, particularly faster or more pronounced than expected, these shifts might signify something more than just age.
Find out more about cognitive performance and aging in our ebook: What’s Happening to My Brain? Understanding and Treating Mild Cognitive Impairment.
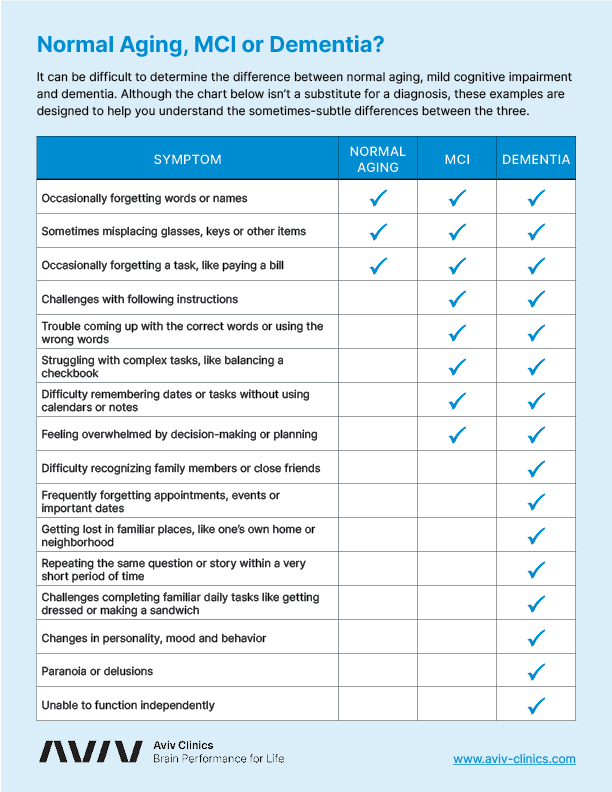
Normal Aging vs. Mild Cognitive Impairment vs. Dementia
Not all cognitive changes point to a diagnosis. Paying attention to these changes can help differentiate what is mild cognitive impairment, what is just the normal aging process, and what may indicate dementia.
Normal Aging
- Occasional memory lapses may occur, and memory loss complaints are infrequent.
- Difficulty finding words may happen, but isn’t a significant source of concern.
- Short-term memory about recent events and conversations is intact.
- The person remains independent, doesn’t get lost in familiar places, and remembers how to perform daily tasks.
Mild Cognitive Impairment
- Memory lapses become a concern for the person or their family members.
- Difficulty finding words occurs frequently and on a somewhat noticeable basis.
- Memory for recent events and conversations becomes impaired.
- The person remains independent but may occasionally have trouble finding their way in familiar places and resist learning new tasks.
Dementia
- Memory lapses are frequent and cause anxiety in the person and close family members.
- Difficulty finding words is noticeable in many conversations.
- Short-term memory, or the ability to maintain conversations, is noticeably impaired.
- The person depends on others for activities of daily living, may get lost in familiar places, and lose the ability to perform tasks that were once routine.
Testing for Mild Cognitive Impairment
If your physician suspects mild cognitive impairment, they’ll likely refer you to a specialist for further examination. However, there’s no single test for MCI. Instead, diagnosis will typically include a combination of assessments.
- Neuropsychological and cognitive function tests are vital as they evaluate cognitive skills like memory, attention, judgment, and planning. These examinations measure the degree of impairment.
- Psychological assessments can also provide a clearer picture of emotional factors that may be impacting cognitive function.
- Specialists will also try to rule out other causes of cognitive dysfunction by reviewing medical and family history, symptoms, and medications.
- Lab tests may reveal vitamin deficiencies, urinary tract infections, thyroid disorders, and other ailments that can mimic MCI symptoms.
- Neurological examinations can detect conditions that impair cognitive function, such as a tumor or stroke.
- Radiological imaging can capture the structure and function of the brain. Diagnostic imaging can reveal brain atrophy or other potential causes of cognitive dysfunction, while functional imaging offers insight into blood flow and metabolic changes in brain tissue. While radiological imaging is often associated with stroke diagnosis, it can be effective in evaluating a number of conditions, including cognitive impairment.
The Aviv Assessment
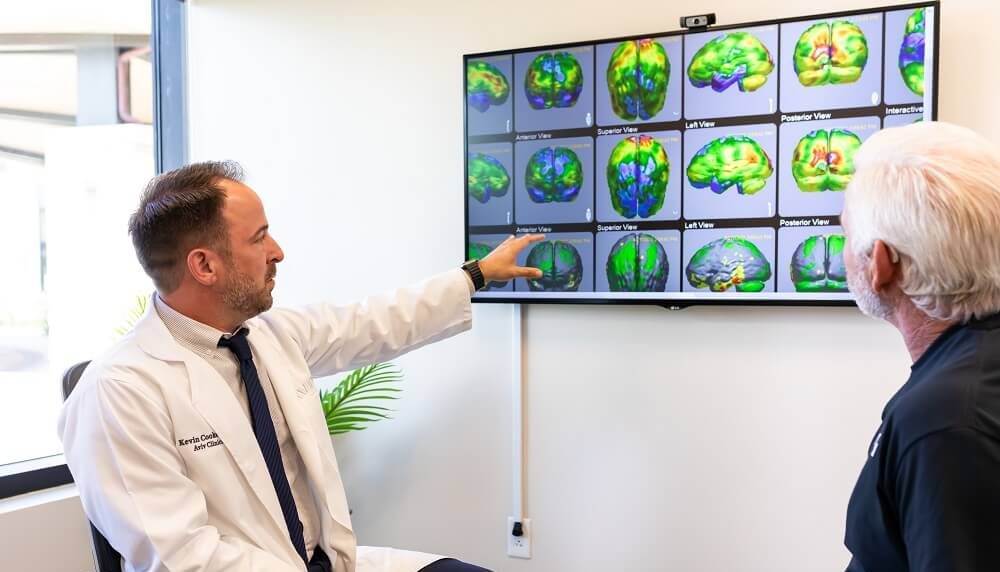
At Aviv Clinics, we use all these tools as part of a comprehensive assessment of both brain and body function. This not only gives our clinical team a full picture of each client’s physical and cognitive health, but it also provides the insight we need to create customized treatment plans.
The Aviv Assessment includes:
- Comprehensive, scientifically validated cognitive tests, including the Montreal Cognitive Assessment, Cambridge Neuropsychological Test Automated Battery, and NeuroTrax
- Neuropsychological evaluation
- Extensive blood tests
- High resolution brain MRI and/or SPECT scans to measure brain activity and structure
- Tests of heart and lung function, including cardiopulmonary exercise testing (CPET), spirometry, and electrocardiogram (ECG)
- Analysis of gait, stance, range of motion, strength, and balance
- Body composition evaluation and dietary assessment
Mild Cognitive Impairment Treatment at Aviv Clinics

A Columbia University study estimates the prevalence of mild cognitive impairment at “22.2% among those 71 years and older.” However, MCI isn’t necessarily permanent—it can sometimes be improved or even reversed.
The Aviv Medical Program is a safe, non-drug intervention that can slow down cognitive decline, particularly in its early stages. Cognitive benefits of the Aviv Medical Program can include:
- Better brain function and connectivity
- Stronger executive function (decision-making, self-control, cognitive flexibility)
- Improved mental abilities, including memory, attention, and focus
- Increased information processing speed
- Improvements in mood and psychological factors, such as depression or anxiety
Real Stories, Real Progress with the Aviv Medical Program
After watching their parents suffer from dementia, Aviv clients Carl and Vickie feared that they were beginning to show some of the same alarming signs they’d observed in their parents. Worried about what could be mild cognitive impairment vs. dementia symptoms, they decided to take control of their aging process through the Aviv Medical Program. Watch their Aviv Clinics recovery story:
Bob and Laurie were also initially drawn to Aviv Clinics after watching Laurie’s father struggle with dementia and Alzheimer’s. From significant cognitive improvements to enhanced vitality, the program empowered them to lead an active and more memorable life with newfound resilience. Here’s their story:
People like Carl, Vickie, Bob, and Laurie are embracing their futures every day at Aviv Clinics. The results speak for themselves.
- 96% of Aviv clients experience clinically verifiable improvements in brain function
- 95% said they would recommend the Aviv Medical Program to their friends and loved ones
If you fear you or someone you love may be suffering from mild cognitive impairment, please contact us. The earlier we can diagnose the condition, the more likely we can treat it.
The Early Stages of Dementia: Recognizing the Signs and Reducing the Risk
We all experience bouts of forgetfulness occasionally, even at a young age. You might blank on an old acquaintance’s name or walk into the kitchen thinking, “What did I come in here for?”
Neither necessarily indicates dementia is in its early stages. Maybe you didn’t have your morning coffee or slept poorly the night before.
However, considering the growing rate of dementia in the U.S. and worldwide, it’s essential to recognize the early stages of dementia in yourself or your loved one. Education is the first step in taking control of your health. We’re here to help you get started.
What Is Dementia?
Dementia is the progressive loss of cognitive functioning (i.e., thinking, remembering, and reasoning) that impacts a person’s quality of life. It ranges from mild to severe.
“More than 55 million people” in the world live with dementia. In the U.S., “experts report more than 7 million people ages 65 or older had dementia in 2020.”
Remember, dementia isn’t a single disease. Instead, it’s a general term covering a range of specific medical conditions (more on this soon).
What Are the Early Signs of Dementia?
Some of the most common signs and symptoms of dementia include:
- Memory lapses: Someone might be unable to recall events or keep losing items around the home.
- Trouble concentrating or focusing: Struggling to make complex decisions, plan events, or solve problems are a few common ways this can manifest.
- Confusion surrounding typical daily routines: Activities like paying bills or navigating a drive home from the grocery store might be more challenging than usual.
- Mood changes: Depression, anger, or irritability can become more frequent. An individual can feel more withdrawn and lose interest in hobbies and people who used to bring them joy.
- Language/communication roadblocks: A person might have trouble grasping the right word or phrase or have wandering thoughts during conversation.
- Instances of disorientation: An individual can no longer recognize where they are or how they got there.
Read about the signs and symptoms of cognitive decline>>

Diagnosis of Early Onset Dementia
As every individual is different and no specific test confirms dementia, a comprehensive evaluation is required. The assessment might involve various medical exams like cognitive tests and brain imaging.
Early detection is critical to getting the help you need to thoroughly prepare following your diagnosis.

Different Types of Dementia
Multiple diagnoses fall under the dementia umbrella and can produce unique symptoms in the early stages.
Alzheimer’s Disease
While the exact cause of Alzheimer’s disease is still unknown, researchers note that the “build-up of proteins in and around brain cells” is a possibility.
Initially, Alzheimer’s impacts the nerve cells controlling memory, language, and conscious thought. Damage then progresses to parts of the brain that manage reasoning and social behavior.
These changes are not always apparent, especially not in the earliest stages. Alzheimer’s can develop for 15–20 years before symptoms start to appear. Currently, it’s estimated that “6.2 million Americans” live with the disease.

Frontotemporal Dementia
Frontotemporal dementia (FTD) results from damage to neurons in the frontal and temporal lobes—areas of the brain that oversee memory and auditory functioning. You may have heard of FTD when the press announced actor Bruce Willis’ diagnosis in 2022.
Symptoms include the following:
- Unusual behaviors
- Emotional problems
- Trouble communicating
- Difficulty with work
- Challenges with walking
Example: Phineas Gage. A classic example involves a railroad construction worker from the 1800s named Phineas Gage, who is now considered the first patient in the history of neuroscience. Although not an example of dementia, Gage’s case offers insight into the importance of the frontal lobe and the functions it controls. While working on the railroad, Gage suffered an accident in which a large iron rod penetrated his skull and frontal lobe, causing brain damage.
Gage survived the incident, but his demeanor and personality changed completely. Previously known as a pleasant, hard-working “gentle giant,” he became, according to Dr. John Martyn Harlow, “…fitful, irreverent, indulging at times in the grossest profanity, manifesting but little deference for his fellows.”
Unlike Gage’s sudden change due to injury, the impacts of frontotemporal dementia develop gradually. The condition tends to strike individuals at a younger age than other forms of dementia. ”Roughly 60% of people with FTD are 45 to 64 years old.”
Lewy Body Dementia
Many learned about Lewy body dementia (LBD) when it was revealed actor/comedian Robin Williams had suffered from the disease. LBD arises from abnormal deposits of a protein called alpha-synuclein in the brain.
These deposits, named “Lewy bodies,” affect brain chemicals, leading to problems with thinking, movement, behavior, and mood. Williams’ struggle with depression was likely a direct result of the chemical changes instigated by LBD.
LBD worsens over time but impacts certain individuals more severely than others. One challenge in diagnosing LBD is that it mimics indications of other brain diseases or psychiatric disorders.
Vascular Dementia
Vascular dementia results from conditions affecting the blood vessels in the brain.
When blood and oxygen flow to the brain is interrupted, it can cause changes in memory, thinking, and behavior. The size, location, and number of vascular changes dictate how severe vascular dementia is on a person’s cognitive function.
For example, someone who has suffered a major stroke may experience damage—but so might someone who has had multiple small strokes over time.
Growing research investigates the connection between cardiovascular disease (heart attack, stroke) and cerebrovascular disease (blood flow/vessel conditions)—and its impact on cognitive impairment and dementia.
That said, not everyone who experiences a heart attack or stroke will develop dementia. The aging process can also contribute to the development of vascular dementia. The body simply loses its ability to deliver blood as efficiently as it once could.
Mixed Dementia & Related Diseases
If someone has characteristics of two or more types of dementia, they may receive a diagnosis of “mixed dementia.” Other neurological conditions can lead to symptoms of dementia, such as:
- Creutzfeldt-Jakob Disease (CJD): This rare, degenerative, fatal brain disorder causes problems with muscle coordination, personality changes (including progressive and impaired thinking and judgment), and vision problems that may lead to blindness and involuntary muscle jerks. Individuals with CJD lose their ability to speak and move, eventually slipping into a coma.
- HIV-Associated Dementia: While less of a problem now that the medical community has curbed the AIDS epidemic, HIV-associated dementia can cause behavioral changes and a gradual decline in cognitive function.
- Huntington’s Disease: This inherited disease eventually leads to brain cell death and resulting complications. HD may cause changes in behavior, emotion, judgment, and cognitive function.
What Else Might Cause Early Signs of Dementia?
If you or a loved one experiences dementia-like symptoms, it doesn’t necessarily mean a dementia diagnosis is forthcoming.
Other factors may lead to dementia-like symptoms. For example:
- Even a minor medical issue, like a urinary tract infection (UTI), can lead to confusion or delirium in older adults.
- If someone doesn’t adhere to their blood sugar medication and their glucose levels drop, they may experience similar symptoms.
- Medication interactions (or medication/supplement interactions) may mimic symptoms of dementia.
That’s why it’s essential for anyone taking medications or supplements to inform their doctor and pharmacist.

The Importance of Early Detection and Reducing Risk
Unfortunately, there’s currently no cure for dementia. Medications have been employed to slow the progression of dementia but with little success.
While there’s no standard early dementia onset treatment, there are steps you can take to optimize your health and reduce dementia risk:
- Engage in cognitive stimulation activities: Just like any other muscle in the body, your brain needs regular exercise to function at optimal levels. Learn something new or dive into brain games like crossword puzzles or sudoku.
- Maintain an active lifestyle and a healthy weight: This includes sticking to a balanced diet like the MIND diet, engaging in physical activity you enjoy, and abstaining from smoking, drug use, and excessive alcohol consumption. Healthy habits can also help manage diabetes, blood pressure, cholesterol, and other chronic conditions.
- Social engagement: Social activities may “reduce the risk of dementia due to mental and intellectual stimulation.” Take time to see loved ones and engage in leisurely activities with them.
- Art and music therapy: Art and music therapy can elicit emotions, memories, and a sense of calm—all of which may “reduce cognitive decline” and enhance the quality of life.
- Pet therapy: The link between individuals and animals holds powerful benefits like increased self-esteem and can “[improve] cognitive performance such as memory or concentration, motor skills and quality of life.”
- Reminiscence therapy: By using all senses (sight, touch, taste, smell, and sound), reminiscence therapy encourages people to remember specific events, individuals, and places. This therapy can help people gain confidence in their cognitive abilities and allows them to reflect upon what holds meaning for them.

The Bottom Line
If dementia is at the root of your or a loved one’s symptoms, the best step you can take is to act quickly.
Groundbreaking research is bringing scientists one step closer to minimizing age-related cognitive decline, especially related to the early stages of dementia. In a test group, patients in this landmark study experienced improved cognitive functions, including memory recall, concentration, and response times.
A health plan based on this unique protocol is now available at Aviv Clinics Florida.
Contact us to learn more about this study and the Aviv Medical Program’s approach to cognitive decline.
How the Link Between Exercise and Brain Health Can Boost Cognitive Function
The science is pretty clear: exercising and maintaining good health are some of the best things you can do to keep the body at peak performance. But there are more than a few options out there when it comes to exercising.
Exercise and brain health are closely linked. Researchers have found that regular physical activity can “delay the effects of both physiological aging and pathological neurodegeneration on brain health.”
To take advantage of the interplay between brain health and exercise, it’s important to understand how exercise is good for the brain—and why. Are some forms of exercise better than others when it comes to the brain? Are there right—or wrong—ways to exercise when maximizing brain power? And how does exercise affect the aging brain?
The answers to these questions can help unlock the power of exercise for brain health.

How Cognitive Abilities Change with Age
As we age, a slight level of cognitive decline is inevitable due to the normal aging process. Issues with memory and slower thinking are to be expected. But older adults are also increasingly at risk for mild cognitive impairment, including “conceptual reasoning, memory, and processing speed,” as well as dementia, which includes conditions like Alzheimer’s disease.
While some of the risk factors for these conditions are out of your control, such as age, genetics, and family history, your overall health plays a role, too. In the event of an unexpected incident, such as a stroke, your general health and wellness become focal points for your recovery.
The more proactive you are with your health, no matter your risk factors or circumstances, the greater your investment in your long-term health potential. Basically, staying healthy and active can help protect your brain.
How Is Exercise Good for the Brain as We Age?
Healthy habits, including a nourishing diet and regular physical activity, are critical players in the healthy aging process. Emerging research discovered that exercise is linked to “improved cognitive performance in older adults with and without cognitive impairment.”
These results are promising for anyone concerned about maintaining cognitive and brain health as they age, especially considering the aforementioned risk factors beyond their control. This occurs primarily because exercise impacts the brain on both a short- and long-term basis—with measurable benefits occurring in both instances.
How Are Exercise and Brain Health Linked?
Anytime you exercise, you’re pumping more blood to your brain tissues. Increased blood flow means more oxygen and other nutrients vital for the brain’s functioning.
In response, the brain also cranks out some helpful molecules, many of which “improve cognitive processes and memory.”
Here are just a few benefits of exercise for the brain:
- Neurotransmitters (NTs) like serotonin, norepinephrine, and dopamine are released, improving mood, motivation, focus, attention, and learning.
- Brain-derived neurotrophic factor (BDNF) helps your brain repair and rebuild, creating new neurons and connections.
- Hormones work with BDNF and can boost your mood and mental clarity.
- Endorphins and other molecules are released, helping relieve pain.
- Increased blood flow delivers nutrients and carries away waste products.
- The hippocampus increases in volume.
Two areas of the brain are particularly important when it comes to cognitive decline: the hippocampus and prefrontal cortex (PFC). These areas are the most susceptible to cognitive degeneration or impairment.
1. Hippocampus
The hippocampus, which is responsible for memory and learning, is affected by exercise in a few ways. Studies show that with aerobic exercise, brain matter shows “an increase in volume of the left and right hippocampus,” an area that often declines in volume as we age. The hippocampal decline also occurs significantly with Alzheimer’s disease, which can be “reduced by 25%” for those with the condition. The hippocampus is also where much neurogenesis (creating new brain cells) occurs—at least if you exercise enough!
2. Prefrontal Cortex (PFC)
The other area benefiting directly from exercise is the prefrontal cortex or PFC—the brain’s “CEO,” responsible for most of our executive functions, including decision-making, attention, problem-solving, and goal-setting. Studies show that older adults, in particular, can benefit from exercise due to increased “executive functions mediated by the PFC.”
A Holistic Approach to Exercise and Brain Health
Exercise benefits brain health significantly because it involves so many bodily processes simultaneously.
Exercise, for both your body and mind, is a powerful practice that can help build confidence, aid in recovery, and even help to stimulate processes “related to cell survival and neuroplasticity” (the brain’s ability to change and adapt).
Aviv Clinics clients receiving the innovative Aviv Medical Program optimize their brain health. Their personalized treatment plan can combine cognitive exercises and physical training, nutritional coaching, and Aviv’s unique research-backed hyperbaric oxygen therapy (HBOT) protocol. As part of the program, clients perform dual-task exercises on the cutting-edge h/p/cosmos medical treadmill at the clinic. The combination of physical and cognitive effort maximizes the benefits of the treatment protocol which include: improved memory, attention, focus, information processing and mental clarity.
Lifestyle Matters
Our brains haven’t changed much in the last 50,000 years or so, but our lifestyle certainly has.
In the days of our nomadic, hunter-gatherer ancestors, life was a little more physically demanding—our bodies are designed to move and be active. Sitting, it seems, could be making us sick.
According to LifeSpan Fitness, the average American these days sits for “11 hours a day,” and an estimated 20% of all deaths over age 35 can be attributed to a sedentary lifestyle. Lack of exercise, poor diet, and use of alcohol, tobacco, or drugs are often a starting point. Falling into this sedentary lifestyle can quickly lead to a downward spiral.
What’s the Best Kind of Exercise?
Rest assured, as long as you’re moving your body regularly, you’ll likely see benefits. While all types of exercise have advantages, most studies favor those that elevate your heart rate and maintain it for a time.
Getting oxygen-rich blood pumping to the brain seems to be the best way to reap the benefits of exercise. Therefore, aerobic exercise (or cardio) and weight training are excellent starting places.
Moderate Intensity
The “prescription” for most older adults is to aim to exercise at a moderate intensity for 30-45 minutes, 3-4 times per week. An easy way to keep track of your progress is with a fitness tracker. Find out if a fitness tracker is right for you.
You can measure moderate intensity by keeping your heart going at the optimal rate, in this case, 70-80% of your maximum heart rate. To determine your max heart rate, subtract your age from 220. For example, a 70-year-old woman’s maximum heart rate would be 150. That means that to exercise at the right intensity, she should maintain a heart rate between 105-120.
You should warm up and cool down for aerobic exercise but don’t count that as part of your total. The 30-45 minutes (as prescribed) should all be while your heart rate is at the target rate.
Strength Training
Strength training can also be incredibly beneficial. Sarcopenia, or the loss of muscle mass as you get older, and osteoporosis, a reduction in bone mass over time, are increasingly common in older adults. Muscle-building exercises can help you retain this muscle mass and build strength in both areas of the body.
To get started, stick to a simple program that activates as many muscle groups as possible throughout the week. With strength training, it’s important to choose activities that are not too easy nor too complex and to give yourself at least one day of rest between sessions.
Avoid injuries by focusing on excellent form, whether lifting weights or performing body weight exercises. Always give yourself time to warm up your muscles with five to ten minutes of heart-pumping cardio or warm up sets before diving into any challenging reps or sets.
6 Tips for Getting Started
If you’re like many (if not most) adults, you might be leaning more toward the sedentary end of the activity scale as you grow older. The exercise prescription above is an ideal goal, and it’s used primarily because that’s what they did in studies showing the best outcomes for cognitive health.
However, other studies showed that lower-intensity activities like walking “roughly 6-9 miles per week” and yoga could be beneficial, too.
Even if you’re aiming for that peak exercise intensity, there are many ways to make exercising for brain health fun, easier, and less stressful.

1. Find Movement That You Love
Exercise is about movement, so find a way to move your body that you enjoy. If that’s running laps, great. If you love to dance, then dance! And there are always sports and leisure activities—gardening, golfing, and bowling are excellent ways to move. Even window shopping or hula hooping can count as exercise. Need more ideas? Try any of these non-boring exercises!
Finding enjoyable movement can also help change your perspective and shift away from goals like weight loss that may feel like a chore. Focus on how exercise makes you feel and the enjoyment you get from moving.
2. Slowly Build Stamina
If you’re already pretty active, or you’ve exercised a lot in the past, it will probably be easier for you to start. If you’re not as active as you could be, that’s okay, too. It’s never too late to begin a new exercise practice. Start small and build from there.
You’re more likely to stick with it if you’re realistic about your goals and abilities.
3. Examine Barriers to Habit
Building any habit takes time and planning. Give yourself the best chance at success by looking at exercise through a positive lens. For example:
- If it’s challenging to find time in your schedule, start with shorter movement durations whenever you can.
- If you dislike the gym, identify ways to stay active by doing things you enjoy, whether being outside, working out with friends, participating in low-impact activities, or exercising right at home.
The best plan accounts for daily routine hiccups that could potentially throw your goals off course. By remaining connected to the positive benefits you get right after you engage in physical activity, such as an improved mood, a sense of accomplishment, or a boost of energy, it’s easier to stay on track even when life gets chaotic.
Remember that every day is a new day, and you can always switch things up or make adjustments as you go without throwing in the towel altogether. Slow and steady progress is more sustainable.

4. Work with Your Schedule
Depending on your exercise goals and your current level of physical activity, it’s a good idea to examine how you can build exercise into your routine naturally. From there, you can make goals to build around the momentum you’ve gained with every small step.
When you start to make goals, the SMART goal-setting method can make it easy to visualize where you’d like to go with your exercise routine.
SMART goals are:
- Specific: Break down precisely what you want to achieve. Rather than make a goal to simply walk more, aim for a specific number of steps or a weekly distance threshold you wish to reach.
- Measurable: Find a way to track your goal with metrics. You might use a pedometer to count your steps or a designated app to count the miles you’ve walked.
- Attainable: It’s enticing to think big. Still, you’re more likely to stick to a movement goal if it feels like an achievable first step. Your plan should push your limits just enough to be effective but not too challenging that you feel discouraged.
- Relevant: Consider the benefits you’d like to gain from your goal. If building muscle is your intention, physical activity focusing on endurance training rather than strength training may make progress slower than if you focus on muscle-building exercises.
- Time-bound: Without putting unreasonable pressure on your results, choose a time frame within which you would like to achieve your goal. This can be a particular date or a certain duration. Scheduling can help you take actionable steps every day.
5. Add It Up
Ultimately, it’s about moving more and being more active. There are many ways to sneak in more exercise and break up the sedentary periods. For example, if you sit a lot, you can try setting a timer to get up and walk around every hour. Or start counting your steps and aim to increase them daily.
Many traditional ways to get more activity are still great, like taking the stairs, parking farther away, playing with kids, or doing housework and cleaning. Make it a goal to find a new way to squeeze in some daily activity.
6. Results Take Time—Be Patient
So how long does it take before exercising starts to pay off? While you may feel many exercise benefits immediately afterward, like improvements in mood and energy, lasting results will take longer. Plan on giving it at least six months to assess your brain’s progress.
Regarding cognitive abilities, measuring and assessing can be challenging. You may not notice a substantial increase in cognitive ability. As some cognitive decline will occur due to normal aging, it’s often about slowing it down rather than a full reversal. It’s also common for family and friends to notice a change before you do.
The Bottom Line on Exercise and Brain Health
Find movement that you enjoy, and you’ll have a much easier time making time to exercise. No matter what shape you’re in or what activities you enjoy, you can find a way to optimize both your physical and cognitive health.
Aviv Clinics delivers a highly effective, science-based treatment program to enhance brain performance and improve the cognitive and physical symptoms of conditions such as traumatic brain injuries, fibromyalgia, Lyme, and dementia. Our intensive protocol uses Hyperbaric Oxygen Therapy, physical training, and nutrition management for better brain health. The medical program closely tracks clients’ progress before, during, and after the treatment protocol, using customized tablets and other technology. Based on over a decade of research and development, the Aviv Medical Program is holistic and customized to your needs.
Age-Related Cognitive Decline: The Science That Slows It Down
Cognitive health — the ability to think clearly, learn, and remember — is essential in helping us live happy and fulfilling lives.
Maintaining our cognitive health can become a challenge as we get older. Like the physical changes that occur in our bodies (e.g., stiff joints, wrinkles, etc.), our brain’s cognition also changes slowly and subtly over time.
You may notice you’re struggling to pay attention, for example, or find you’re having trouble recalling conversations or people’s names. These experiences are a natural part of aging and manifest as a condition coined age-related cognitive decline.
Cognitive Decline, the Earliest Symptom of Dementia and Alzheimer’s Disease
According to the Centers for Disease Control and Prevention (CDC), cognitive decline is a self-reported experience of “worsening or more frequent confusion or memory loss.” It’s considered one of the earliest symptoms of Alzheimer’s disease and other related dementias.
There are different forms of cognitive decline. One type of cognitive decline is mild cognitive impairment (MCI)—the early stage of memory or cognitive ability loss. It’s the phase between natural cognitive decline (due to aging) and the more serious decline.
While experiences may be different person-to-person and can vary daily in scope and severity, common age-related cognitive decline symptoms include the following areas:
- Memory: Forgetting names, dates, and places becomes more frequent. You may place items in odd locations (e.g., car keys in the refrigerator).
- Language: Forming words, phrases, or sentences becomes increasingly more challenging.
- Thinking or judgment: You may lose track of time or your train of thought. Making decisions also becomes more difficult or overwhelming.
- Apathy: An oft-overlooked symptom, suddenly losing interest in your favorite activities and people or giving up when something feels difficult can signal a mental withdrawal during the decline process.
- Incessant rumination: People experiencing cognitive decline can feel chronic stress or get stuck in a fight-or-flight response.
- Other Conditions: Many illnesses and chronic conditions are associated with cognitive decline. They include influenza, gastroenteritis, sleep disorders, diabetes, and cardiovascular issues.
If you are experiencing any of these symptoms, take the opportunity to have a conversation with an Aviv Clinics physician to assess their severity and what you can do to improve your cognitive health.
Why Age-Related Cognitive Decline Occurs
There are four main reasons age-related cognitive decline may occur:
- Hormonal imbalance: As we age, it’s natural for hormonal imbalances to happen. Research indicates these changes are a key factor in the decline of cognitive function.
- Stroke and head injuries: Head injuries and stroke can damage blood vessels in the brain, which may incite cognitive impairment and even vascular dementia. Even a minor head injury sustained many years in the past increases your chances of developing dementia.
- Psychiatric disorders: Disorders like depression and anxiety have been connected to cognitive and functional decline. They are commonly experienced by MCI patients and can either be a contributing factor or a symptom.
- Heart conditions: Research shows that those in their 40s to early 60s with high blood pressure have a higher risk of experiencing cognitive decline later in life. Lowering blood pressure decreases the risk for MCI.

Disorders Related to Age-Related Cognitive Decline
Approximately 12% to 18% of individuals over age 60 live with mild cognitive impairment. If left untreated, MCI can bring on various disorders related to more significant age-related cognitive decline.
Approximately 10% to 15% of people with MCI develop dementia every year. Dementia is an umbrella term that encompasses a variety of neurological conditions. These conditions negatively affect the brain—nerve cells stop functioning normally and eventually die, causing cognitive decline.
There are different types of dementia, such as:
- Alzheimer’s disease: Those with MCI are at greater risk of developing Alzheimer’s disease—the most common dementia diagnosis. In addition to cognitive decline, those with Alzheimer’s may experience shifts in behavior and personality. Read about the risk factors for Alzheimer’s disease.
- Frontotemporal dementia (FTD): FTD can occur when there is damage to the frontal and temporal lobes of the brain. Someone with FTD can show unusual behaviors, emotional problems, and difficulty communicating.
- Lewy body dementia (LBD): LBD happens when protein builds up in the brain. Common symptoms of LBD include movement issues (e.g., slowed movements, stiffness, tremors), cognitive issues, and mood shifts.
- Vascular dementia: Vascular dementia occurs due to a lack of blood flow to the brain. People typically experience issues with reasoning, planning, judgment, and memory.
How Science Slows Down Cognitive Decline
Your brain is a superpower, but energy (in the form of oxygen and proper nutrition) is needed to make it so.
If you give your brain energy, especially as you age, you can effectively slow down the aging process.
Aviv has developed a way to harness the power of oxygen using Nobel Prize-winning research. The Aviv Medical Program includes a variety of therapies, including Hyperbaric Oxygen Therapy (HBOT). What is HBOT? It involves sending 100% pure, pressurized (10-15 times higher than normal) oxygen to your deprived brain cells and body tissues, turbocharging your body’s own regenerative mechanisms. The result is faster healing of damaged tissues and higher regeneration of stem cells.
If you’re concerned about your (or a loved one’s) age-related cognitive decline, be sure to contact Aviv soon.
Role of Genetics in Alzheimer’s
Alzheimer’s is currently the most widely diagnosed form of dementia in the United States.
It is a progressive disease that worsens over time, often to the point of interfering with daily activities.
While doctors have begun to understand more about what causes Alzheimer’s, we are still discovering exactly what sets off the disease process.
Are some people predisposed to the Alzheimer’s disease? Is there any action we can do to delay, or even prevent it?
Read on to learn more about Alzheimer’s disease and the role genetics and lifestyle play in it.
What is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia most commonly affecting people over the age of 65, though younger people can be impacted as well.
It is a progressive disease— symptoms are usually mild at onset and get worse over time, eventually becoming severe enough to interfere with daily living.
In the early stages, people with Alzheimer’s tend to experience minor memory loss—for example, forgetting a person’s name or details of a recent event. As the disease progresses, cognitive functioning declines, causing more significant memory loss and other symptoms including:
- Difficulty making decisions
- Confusion and disorientation in places that were once familiar
- Speech and language challenges
- Personality changes
- Problems performing self-care tasks
- Ambulatory issues
- Hallucinations
- Low mood
- Anxiety
People with Alzheimer’s won’t necessarily exhibit all of these symptoms every day, and some days may be better than others.
What Causes Alzheimer’s?
Scientists have researched the disease process of Alzheimer’s for years. While we are still identifying what can cause a person to develop Alzheimer’s, we have made some discoveries about how the brain works in Alzheimer’s disease patients.
Today we know that there are two different protein structures in the brain associated with Alzheimer’s disease: Neurofibrillary tangles and amyloid plaques. It’s not currently known whether the presence of these structures causes Alzheimer’s disease, or if they are simply byproducts of it. We do know that both can impair cognitive function and can worsen as the disease progresses.
Neurofibrillary tangles are accumulations of a harmful protein called tau in the brain’s neurons. These tangles can inhibit the neuron’s ability to communicate, causing cognitive decline. Some studies reveal that a lack of oxygen in the brain is associated with neurofibrillary tangles.
Amyloid plaques are hard, insoluble clumps of beta-amyloid proteins that build up between neurons. Like neurofibrillary tangles, these plaques are toxic to brain cells and disrupt cell-to-cell communication. They can eventually result in cellular death, inhibiting cognitive abilities even further.
Brain scans can reveal the presence of both protein structures, which can alert your doctor to the presence of Alzheimer’s disease or indicate that you’re at risk for it.
This information can be used to help you adopt lifestyle changes and seek treatment to help maintain your health and prolong your cognitive function.
Who Gets Alzheimer’s Disease?

Alzheimer’s is most common among people over the age of 65. In fact, an estimated 1 in 14 people over the age of 65 and 1 in 6 people over the age of 80 have Alzheimer’s.
While age is the biggest risk factor for the disease, Alzheimer’s can also happen to people who are younger. This is known as early-onset Alzheimer’s.
Women also make up a disproportionate number of Alzheimer’s cases, possibly because women tend to live longer than men. It also may be linked to the reduction of the hormone estrogen that women experience when they go through menopause.
Lifestyle, as well as other diseases, like diabetes, stroke, and heart disease, are also thought to play a role in the development of Alzheimer’s. Working to live a healthy life and control the onset of other chronic illnesses can help reduce your risk of acquiring Alzheimer’s as you age.
One major risk factor that we can’t control is genetics. Understanding how heredity influences the disease process and what we can do to mitigate it are important for making sense of the disease, as well as exploring timely options for prevention and treatment.
Alzheimer’s and Your Genes
We all know that genetic factors can impact our health in a variety of ways. Brain health and dementia are not immune to this connection. The link between Alzheimer’s disease, specifically early-onset Alzheimer’s, and genetics is apparent.
Scientists have found that genetics are often a contributing factor among those who develop early-onset Alzheimer’s, meaning they are likely to have an immediate family member who also developed the disease before age 65.
For those who develop the disease later in life, the impact of genetics is less defined, though family history still seems to be an important risk factor.
Another potential genetic indicator comes in the form of certain mutations of the APOE gene. Mutation in this gene is associated with higher levels of amyloid plaques and is often found in people who suffer from Alzheimer’s disease.
Your doctor can conduct tests to determine if you have this gene mutation and are at greater risk of developing Alzheimer’s because of it.
However, people who are genetically predisposed to develop Alzheimer’s disease may never develop it. But knowing your genetic composition can be powerful, especially if the information helps motivate you to make lifestyle choices that can help postpone or prevent your development of the disease.
What You Can Do to Help Prevent or Delay Alzheimer’s Disease?

There’s not much you can do about your genes—you didn’t select them or your parents. However, you can choose to live in a way that minimizes the impact your genes have on you and your health.
It’s important to focus on what you can control.
- Take care of your mental health,
- Practice mindfulness
- Challenge your brain
- Maintain strong social connections and relationships
- Get quality sleep
- Eat a healthy and nutritious diet
- Exercise to help prevent the development of other chronic conditions, like diabetes and heart disease
- Avoid smoking and drinking to excess
- Be careful not to expose your brain to harmful substances or to the risks of sustaining traumatic brain injuries
These behaviors can impact your cognitive function and may act as controlling factors for Alzheimer’s and other forms of dementia.
Recent research has also shown that Hyperbaric Oxygen Therapy (HBOT), like the specialized protocol used at Aviv Clinics, can be effective for preventing and addressing cognitive decline, especially as it relates to the early stages of Alzheimer’s and dementia.
A unique protocol of HBOT can work to increase blood flow to the brain and reverse amyloid plaques and even prevent them from forming in the first place. It may be a viable option to help prevent and treat Alzheimer’s disease in the near future.
Remember, it’s not just about how long you live, but also how well. Making an effort to care for yourself now will help you enjoy a longer, more full and active life while minimizing chronic health issues and cognitive decline.
Bottom Line
Genetics is just one of the risk factors for Alzheimer’s. While it’s not something you can control, it is something you can impact through your behaviors.
People often underestimate the power that lifestyle choices can have on their future health, but they are an integral part of the overall equation. The way you care for your body today, or fail to, can have a major impact on not only your lifespan but your healthspan as well.
The Effect of Coffee on Brain Health
Last Updated July 22, 2025
Pour-over, solo, drip, French-pressed—however you enjoy your coffee, it may do more than just help you get going in the morning. Research suggests that drinking coffee may protect against a variety of health conditions, as long as it’s consumed in moderation.
For decades, coffee had a poor reputation due to early studies that labeled it a carcinogen and linked it to an increased risk of heart disease. But recent research shows that drinking coffee, including decaffeinated coffee, may provide a variety of health benefits when enjoyed in moderation.
The Benefits of Coffee on Brain Health
Some of coffee’s health benefits are commonly known, including that it boosts metabolism and increases energy levels. But coffee may also deliver lesser-known, but potentially more important advantages for the brain. These include:
- Enhancing brain function
- Lowering the risk of developing dementia and Alzheimer’s disease
- Decreasing the risk of stroke and depression.
Beyond brain health, moderate coffee consumption has been linked to reduced risk of some cancers, type 2 diabetes, and heart disease.
Coffee’s Key Ingredients
Caffeine is just one of about 1,000 chemicals found in coffee beans, but it is the best known. As a stimulant, caffeine delivers a boost of energy and helps provide focus. It locks into the adenosine receptors in the brain, which cause drowsiness, and counteracts the sleepiness response by blocking the function of the receptors. Instead of feeling drowsy, caffeine stimulates the brain’s production of norepinephrine and dopamine, which is what leads to increased focus and alertness.
But caffeine isn’t the only beneficial component. Coffee also contains beneficial polyphenols and antioxidants, which fight inflammation and protect against some diseases.
Polyphenols are organic compounds with anti-inflammatory properties that have the potential to prevent or reduce the risk of certain cancers and other chronic health conditions. Some polyphenols may protect against neurodegenerative diseases, including Alzheimer’s, Parkinson’s, and Huntington’s. Additionally, polyphenols also may help regulate metabolism, weight, and cellular function.
Other beneficial components in coffee include:
- Vitamins B1 (thiamine), B2 (riboflavin), B3 (niacin) and B5 (pantothenic acid)
- Folate
- Manganese
- Potassium
- Magnesium
- Phosphorus.
Coffee beans may also support gut health by offering prebiotic and probiotic properties once ground and brewed.

The Cons of Drinking Coffee
While coffee has many health benefits, it can also have some negative effects. For example, it can:
- Disrupt sleep
- Cause anxiety or agitation
- Lead to caffeine dependence
- Trigger withdrawal symptoms (headache, fatigue, brain fog, and irritability) when abstaining
Moderating consumption is key to enjoying its benefits.
How Much Coffee Should You Drink?
Like most things in nutrition, balance matters. Coffee is a healthy beverage when consumed in moderation. The Dietary Guidelines for Americans recommends no more than about 400 mg of caffeine, or about 2-3 12-ounce cups. Too much, especially in the afternoon or evening, can interfere with sleep quality and may create feelings of anxiety.
Optimizing the Benefits of Coffee
While coffee has many health benefits, its value can be undermined by added sugars, creamers, or flavored syrups.
“The extra calories, sugar, and saturated fat in a coffee house beverage loaded with whipped cream and flavored syrup might offset any health benefits found in a basic black coffee.” – Harvard School of Public Health

Brewing methods also matter when it comes to your health. Using a paper filter or selecting coffee pods with built-in filters helps prevent the passage of unhealthy chemicals present in your brew. Some of these chemicals can raise levels of LDL, also known as the “bad” cholesterol.
Supporting Brain Health with More Than Just Coffee
A daily cup of coffee may support brain function, but it’s one small part of a much bigger picture. At Aviv Clinics, we take a comprehensive, science-backed approach to brain health and performance. Our personalized treatment plans address cognitive and physical health with a cutting-edge hyperbaric oxygen therapy that can be combined with other evidence-based therapies. These include cognitive training, nutritional guidance, and physical performance coaching to help optimize your mind and body.
Whether you’re experiencing early signs of cognitive decline or simply want to stay sharp and energized as you age, our team is here to help.
Discover how the Aviv Medical Program can support your brain health goals—today and in the years to come. Contact us to learn more.
The Powerful Link Between Music and Memory: What the Science Shows
Last Updated July 9, 2025
Music has a special way of interacting with our brains. For a person with Alzheimer’s disease or other cognitive impairment, hearing a familiar song can trigger a memory, evoke an emotion, and enhance brain performance.
Studies have shown that music can have a profound effect on people with memory loss conditions, including Alzheimer’s disease and dementia. That growing body of evidence has led some long-term care facilities and caregivers to use music therapy to entertain, soothe, and help socialize residents with dementia and similar issues.
Music is a part of nearly everyone’s life. Many parents use music to soothe a fussy baby, and even for adults, music often serves as a soothing distraction, to elevate mood, as a motivator while exercising, or as a relaxation technique at bedtime. Still others use music as background noise as they go about their daily lives. Music may be such an ever-present fixture in everyday life that it becomes woven into the fabric of the brain. Music stirs our emotions and embeds itself in our memory, creating a link that ultimately becomes associated with a time, a person, or a place.
Why does music unlock memories? It activates those areas of the brain that are associated with memory and emotions: the hippocampus and the frontal cortex. When these areas of the brain are stimulated, they trigger the release of stored memories at the sound of a song.

How Music Impacts the Brain
Music can have a powerful effect on the psyche. For a person with dementia or in late-stage Alzheimer’s disease, music reduces agitation, soothes the spirit, and improves behavior and focus, research shows.
Music’s Effects on the Mind
- Music stimulates the brain by evoking an emotion that triggers a memory. For someone with memory loss, hearing a familiar song has the potential to transport them back to a more pleasurable time.
- It provides comfort. A person with cognitive decline can become easily agitated. Music has a way of reducing agitation and instilling a sense of calm.
- Music elevates mood and reduces stress. Playing music activates a part of the brain that can improve mood and reduce anxiety, especially if the music is familiar and well-liked. Studies have shown that different types of music may have different effects. Soothing music at less than 100 beats per minute, such as classical music, is associated with a positive effect on memory and cognition.
- It creates a connection without verbal communication. For someone in the late stages of Alzheimer’s disease, communicating may be difficult if not impossible. Expose a person with severe memory loss to a song from childhood, and they may break out in song or dance.
Music’s Role in Alzheimer’s and Stroke Recovery
Famed musician Tony Bennett was diagnosed with Alzheimer’s disease many years before his death. However, he was still able to perform and remember the lyrics despite memory impairment.
Music has also been used as a therapeutic method to help stroke patients with aphasia relearn speech. While they may not be able to converse, they can often sing a familiar tune. Using music can stimulate different parts of the brain to relearn and improve speech.
Tips for Using Music as a Caregiver
To use music to soothe a loved one with memory-loss issues, try these tips from the Alzheimer’s Association:
- Choose music your loved one is familiar with and once enjoyed. If they’re able, encourage them to offer suggestions for their customized playlist.
- Play commercial-free music, as interruptions can be disruptive and confusing for them.
- Base your choice of music on the emotion you’re trying to invoke. A tranquil song may induce a calm and serene feeling. A faster-paced tune from their youth might help elevate mood and evoke happy memories.
- Enhance their experience by encouraging them to tap to the beat, clap, or dance.
- Keep distractions to a minimum. Avoid other background sounds, and keep the music volume at a comfortable level. If it’s too loud, it could lead to aggression or agitation.
Supporting Brain Health at Aviv Clinics
The link between music and memory is significant. Studies show that hearing music from our past can trigger strong emotions and a nostalgic connection. Not only can music spark memories, it may also boost mood, calm anxiety, and reduce confusion.
At Aviv Clinics, we understand the deep connection between the brain, memory, and emotion. We designed our comprehensive Aviv Medical Program to address changes in the brain associated with aging, stroke, and conditions like Alzheimer’s and dementia. While music therapy is not a formal part of our program, it aligns with our philosophy: that targeted interventions can help unlock cognitive potential and improve quality of life.
If you or a loved one is experiencing early signs of cognitive decline, our team is here to help guide you.
Diagnosed with Cognitive Decline? Here’s What to Do Next to Protect Brain Health
Last Updated July 9, 2025
You’ve Been Diagnosed With Cognitive Decline. Now What?
Whether your cognitive decline diagnosis indicates mild cognitive impairment (MCI), dementia, or Alzheimer’s disease, exploring the possible causes is the first step in moving forward.
Symptoms, like forgetting where you placed your glasses, frequently asking the same questions, or failing to recognize familiar people, may have led you to seek medical attention. Perhaps your family noticed changes in your mood or personality and urged you to see a doctor. While your diagnosis is likely frustrating and disconcerting, the most important thing is how you proceed from here.
Sometimes, cognitive issues are caused by something treatable like high blood pressure, high blood sugar, stress, anxiety, medications, or drug and alcohol use. No matter the cause of your decline, the key is to address those factors that can be controlled and treated, then choose a healthier lifestyle moving forward.
Understanding Cognitive Decline and How It Affects Daily Life
Cognitive impairment occurs when a person experiences difficulty remembering, learning new things, concentrating, or making decisions that impact their everyday life. It can range from mild to severe, escalating to the point where the person loses the ability to comprehend, write, or speak. At that stage, a person can no longer live independently.
Age is the greatest risk factor for cognitive impairment.
According to the CDC, cognitive disabilities affect 13.9 million Americans, making it the most common type of disability in the U.S. The Alzheimer’s Association estimates that 7.2 million Americans aged 65 and older currently have Alzheimer’s disease. That number translates to roughly 1 in 9 older adults.
Six Actions to Take After a Cognitive Decline Diagnosis
Stress and anxiety will most certainly follow on the heels of a diagnosis. Learning to cope in healthy ways will be crucial because stress and anxiety can worsen symptoms of cognitive decline. You may be tempted to isolate because you fear being embarrassed by your condition or want to hide your frustration when you are challenged to remember. However, do not shy away from being challenged. Do just the opposite. Interact even more and engage in things that bring you joy. How you proceed after diagnosis could slow the progression or alter the trajectory of the disease.
Here are six things to do immediately, no matter the diagnosis:
- Eat a balanced diet with plenty of brain-beneficial foods, including blueberries, nuts, leafy vegetables, and fatty fish like salmon, tuna, and sardines. Fatty fish contain omega-3 fatty acids, which the brain uses to build neurons, and are essential for learning and storing memories.
- Exercise for at least 30 minutes, five times a week. When you exercise, you feed your brain with oxygen and other nutrients vital for its functioning.
- Challenge your brain daily with activities that keep it stimulated. They help exercise the brain, enhance creativity, improve problem-solving, and may slow memory decline.
- Get adequate sleep. Stay away from things that may overstimulate your brain or body before bedtime. Sleep allows your body to cleanse the brain of toxins and waste. Getting enough is essential.
- Find a good support system. It will be critical to build a good support system now that you have received a diagnosis. Whether it is a spouse, a friend, a family member, or a support group, having social connections can keep you from feeling alone.
- Manage stress. Self-medicating with drugs and alcohol will only worsen the symptoms of cognitive decline. Instead, try journaling, prayer, meditation, exercise, or similar activities to reduce your stress load.

Is Cognitive Decline Reversible?
In some people, mild cognitive impairment can be reversed or remain stable, especially if it is linked to a medication. For others with a diagnosis of dementia or Alzheimer’s disease, the outlook can be more challenging. Both Alzheimer’s and dementia are progressive conditions, meaning symptoms will eventually worsen. However, making lifestyle changes like healthy eating and exercising may slow the rate of decline.
Maintaining healthy lifestyle choices, including proper nutrition, exercise, social and cognitive activities, and adequate sleep, may help prevent or delay the onset of cognitive challenges.
Hope After Diagnosis: How Aviv Clinics Can Treat Early Cognitive Decline
At Aviv Clinics, we understand how overwhelming a diagnosis of cognitive decline, dementia, or Alzheimer’s can feel. But we also believe that hope doesn’t end with a diagnosis — it starts with a plan.
Our board-certified team of clinical experts specializes in helping people take control of their cognitive future. The Aviv Medical Program is an evidence-based, personalized treatment approach that goes far beyond symptom management. This comprehensive program uses a unique hyperbaric oxygen therapy (HBOT) protocol and advanced diagnostics to prescribe interventions tailored specifically to your concerns. These may include physical training, nutritional guidance, and cognitive exercises to target the causes of your cognitive decline.
Clinical research has shown that the unique HBOT protocol used in the Aviv Medical Program can improve memory, attention, and processing speed in older adults. Studies show it may even reverse key biomarkers associated with Alzheimer’s disease. For individuals looking to protect and optimize brain performance, this program offers a proactive path forward.
Whether your symptoms are mild or more advanced, our goal is the same. We want to help you preserve what matters most — your independence, your memories, and your quality of life.
Contact us to schedule a free consultation and learn how the Aviv Medical Program can help you or your loved one maintain long-term cognitive health.
Understanding Alzheimer’s Risk: Causes, Prevention, and the Promise of Hyperbaric Oxygen
Last Updated July 8, 2025
We all experience occasional memory lapses, especially as we age. For most of us, these minor cognitive issues are usually just annoyances. But if your cognitive issues interfere with your daily life, they could be the beginning of something much more serious.
Read on to learn more about the risk factors for Alzheimer’s disease and how you can preserve your cognitive health.
What Is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia that impacts a person’s ability to think, reason, and remember. As it progresses, Alzheimer’s can severely affect quality of life, eventually becoming completely debilitating.
The most common type of Alzheimer’s disease is the late-onset form, when symptoms usually “become apparent in [a person’s] mid-60s or later.”
10 Early Signs and Symptoms of Alzheimer’s Disease:

According to the Alzheimer’s Association, ten early warning signs of late-onset Alzheimer’s disease include:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks
- Confusion with time or place
- Trouble understanding visual images and spatial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgment
- Withdrawal from work or social activities
- Changes in mood and personality
If you experience a cognitive problem that impacts your daily life, don’t ignore it. Dementia is not a normal part of the aging process. The sooner you seek help, the sooner you can take action against cognitive decline.
Get in touch with our care team>>
What Are the Risk Factors for Alzheimer’s Disease?
Science is still learning how Alzheimer’s disease develops and why some people are at greater risk of developing it than others. It’s an active area of study, and researchers are making new discoveries every day.
The consensus among scientists is that a combination of age, sex, genetic, environmental, and lifestyle factors all contribute to the development of Alzheimer’s disease.
Let’s take a closer look at some of the greatest risk factors for Alzheimer’s:
- Although old age does not directly cause Alzheimer’s disease, the risk of developing Alzheimer’s “doubles about every 5 years” after age 65.
- More women than men develop Alzheimer’s disease, although this may be because women live longer than men on average.
- Suffering from a traumatic brain injury (TBI) can increase the long-term risk of developing Alzheimer’s or another type of dementia.
- Acute and chronic inflammation are both associated with an increase in cognitive decline. Eating a diet full of inflammatory foods like processed sugar may exacerbate the risk of developing inflammation in the brain.
- Exposure to environmental pollutants has been linked to an increased risk of dementia. Some researchers believe that nearly half of the individual differences in Alzheimer’s risk may be because of environmental factors.
- Being a smoker carries a significantly increased risk of developing Alzheimer’s disease. This risk factor offers another compelling reason to quit.
- People with Down syndrome also have a greater risk of developing Alzheimer’s disease. About 30% of people with Down syndrome develop Alzheimer’s disease by their 50s. The risk reaches closer to 50% in their 60s.
The Role of Brain Proteins in Alzheimer’s: Amyloid Plaques and Tau Tangles
Scientists typically focus on two different protein structures in the brain associated with Alzheimer’s disease: Neurofibrillary tangles and amyloid plaques.
It’s not currently known whether the presence of these structures causes Alzheimer’s disease or if they’re simply byproducts of it. But both can impair cognitive function and can worsen as the disease progresses.
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a simple blood test available at Aviv Clinics may be able to answer this question: pTau Testing
Neurofibrillary Tangles
Neurofibrillary tangles are accumulations of a harmful protein called tau in the brain’s neurons. These tangles can inhibit the neurons’ ability to communicate, causing cognitive decline. Some studies reveal that a lack of oxygen to the brain is associated with neurofibrillary tangles.
Amyloid Plaques
Amyloid plaques are hard, insoluble clumps of beta-amyloid proteins that build up between neurons. Like neurofibrillary tangles, these plaques are toxic to brain cells and disrupt cell-to-cell communication. They can eventually result in cellular death, harming cognitive abilities even further.
Brain scans can reveal the presence of both protein structures, so your doctor can alert you to the presence of Alzheimer’s disease or if you’re at risk for developing it.
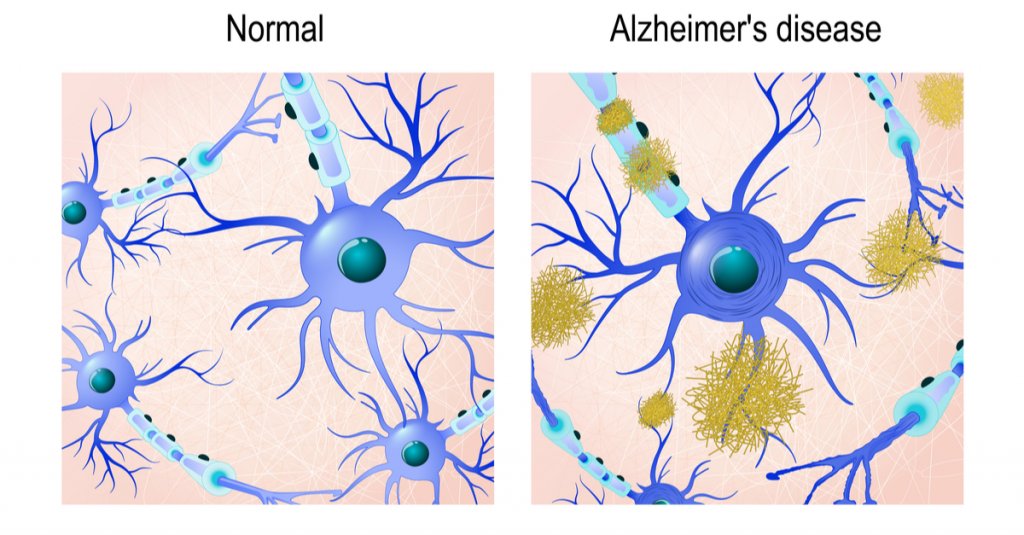
Is Alzheimer’s Disease Genetic?
Both early-onset and late-onset Alzheimer’s disease have a genetic component, meaning if you have a family history of Alzheimer’s, you carry a greater risk for developing the disease. The risk factor is greater if an immediate family member suffers from the disease, such as a parent or sibling.
Genetics are almost always the primary contributing factor of early-onset Alzheimer’s disease, which can affect people as young as their 30s or 40s.
Gene Mutations
Researchers have yet to identify any specific genes directly responsible for the development of late-onset Alzheimer’s. However, certain mutations of the APOE gene, which are found in chromosome 19, are currently considered the strongest genetic risk factor for Alzheimer’s disease.
For example, the specific gene mutation APOE ε4 is linked to higher levels of amyloid plaques and is often found in people with Alzheimer’s disease.
Your doctor may order genetic testing if you have a family history of cognitive problems or early-onset dementia.
Remember, this doesn’t mean you’re destined to develop Alzheimer’s if a parent or sibling has had it. Some people who possess the APOE ε4 gene never develop Alzheimer’s disease, and some people with Alzheimer’s don’t have any gene mutations at all.
Genetics is just one of many Alzheimer’s risk factors. We still need more research to develop a complete picture of what the largest risk factor for Alzheimer’s disease is.
Can Hyperbaric Oxygen Therapy Help Prevent Alzheimer’s Disease?

A specific hyperbaric oxygen therapy (HBOT) protocol shows promise as a potential preventative measure for Alzheimer’s disease. HBOT is a treatment that involves breathing 100% oxygen in a pressurized chamber to increase oxygen levels in the body and brain. A unique HBOT protocol used at Aviv Clinics has shown several benefits in individuals at risk for or experiencing early cognitive decline:
Benefits of HBOT for Alzheimer’s Disease:
- Improves brain tissue oxygenation
- Lowers neuroinflammation (inflammation in the brain)
- Shrinks beta-amyloid plaques (in laboratory animals)
- Reduces pTau protein levels (in laboratory animals)
- Improves memory recall and cognitive performance
- May slow or reverse early signs of cognitive decline
These benefits have been documented in peer-reviewed studies. This specialized HBOT protocol is available exclusively at Aviv Clinics in Central Florida.
In one study, repeated HBOT sessions showed reduced brain hypoxia, reduced amyloid plaques and pTau, and improvements in cognitive performance. Another study found improvements in memory recall in people with mild cognitive impairment (MCI), a potential early stage of Alzheimer’s. Researchers concluded that HBOT “should be considered as a therapeutic approach to slow the progression or even improve the pathophysiology responsible for [Alzheimer’s] disease.”
Lifestyle Habits That May Lower Your Alzheimer’s Risk
While none of us can change our genetic makeup, we can change our lifestyle. Healthy habits can help lower your risk factor for nearly any disease, not just cognitive conditions. Lowering inflammation levels in your body can also help lower inflammation in the brain. To help preserve your cognitive health:
- Eating a healthy diet full of fruits and vegetables
- Exercising regularly
- Maintaining healthy blood pressure
- Keeping your mind active
- Maintaining a healthy weight
- Practicing mindfulness and meditation
- Avoiding excess alcohol
- Avoiding smoking
- Getting plenty of restful sleep
- Taking care of your mental health
How the Aviv Medical Program Can Support Brain Health
The Aviv Medical Program is a personalized intervention designed to improve brain and body health. Using the unique HBOT protocol discussed earlier, alongside other evidence-based interventions, this program can treat both physical and cognitive performance in older adults. In clinical trials, this protocol has also reversed key biomarkers of the aging process.
Depending on your symptoms, needs, and goals, our clinical team will perform an assessment that may include:
- In-depth medical history review
- Comprehensive physical and neurological exam
- Physical therapy evaluation
- Highly advanced brain imaging scans
- Neurocognitive tests
Once our board-certified physicians review your results, they’ll prescribe a customized treatment program designed to treat your concerns. This program may include:
- A specialized hyperbaric oxygen therapy protocol
- Physical training
- Dietary coaching
- Cognitive exercises
- Other interventions as prescribed
Real Client Results: Carl and Vickie’s Cognitive Improvements
Married couple Carl and Vickie both had parents with dementia and cognitive decline. They soon realized they were beginning to experience the same cognitive issues that they saw in their parents.
The couple’s quality of life was not where it should have been, so they took action with the Aviv Medical Program. They use one word to describe their improvements in cognitive performance: “remarkable.”
I’m dancing, I’m hiking, I’m running again. It’s just remarkable. I don’t know how else to say it.” –Vickie Eckert, Aviv Medical Program Alumna
Take Control of Your Brain Health With Aviv Clinics
While science is still investigating all of the risk factors for Alzheimer’s disease, anyone can lower their likelihood by taking charge of their lifestyle.
Preserving your cognitive health starts with the choices you make every day. Partnering with Aviv Clinics is just one of them. Contact our medical team to learn how we can help you.