Study Shows Hyperbaric Oxygen Therapy (HBOT) May Reverse Early Alzheimer’s Symptoms and Amyloid Plaques
Study Shows Hyperbaric Oxygen Therapy (HBOT) May Reverse Early Alzheimer’s Symptoms and Amyloid Plaques
Can science reverse Alzheimer’s disease? A groundbreaking study has brought scientists one step closer to preventing and curing age-related cognitive decline, especially related to the early stages of Alzheimer’s disease and dementia.
This landmark study, published in Aging on September 9, is part of an ongoing program researching age-related cognitive decline. Conducted by the Sagol School of Neuroscience and Tel Aviv University, the study marks the first time that hyperbaric oxygen therapy (HBOT) — a noninvasive and non-pharmaceutical method — has proven effective in reversing the main activators and early symptoms of Alzheimer’s disease.
HBOT is a form of oxygen therapy that involves administering 100% pure oxygen to a patient in a pressurized environment. It has been used for more than half a century to treat conditions such as non-healing wounds and decompression sickness. The study used a specific protocol of hyperbaric oxygen therapy designed to initiate the hyperoxic-hypoxic paradox in cells.
A treatment based on this unique protocol is now available at Aviv Clinics Florida.
How Aging and Blood Flow Contribute to Alzheimer’s Risk
The brain is an incredibly complex organ, home to a vast network of nerve cells (neurons) that rely on oxygen to thrive. As we age, the number of efficient and effective blood vessels in our brain naturally begins to decline. This causes reduced blood flow to the brain, which in turn causes the brain to receive less oxygen. This decreased blood flow is called vascular dysfunction, and it’s a known precursor to Alzheimer’s disease, along with amyloid plaques.
Amyloid Plaques and Their Role in Alzheimer’s Disease
Amyloid plaques are hard, insoluble clusters of proteins formed in the spaces between the neurons in your brain. A healthy brain usually flushes them out without consequence. However, just like plaque can accumulate on your teeth if you don’t clean them regularly, the same thing can happen in your brain.
As the brain ages, it’s more susceptible to forming amyloid plaques in its blood vessel walls. Once an amyloid plaque forms, it can damage the neurons in the brain. These plaques are thought to contribute to the progression of Alzheimer’s disease and the cognitive decline associated with it.
For years, scientists have wondered whether or not it’s even possible to dissolve or shrink amyloid plaques. The groundbreaking new study proves for the first time that a unique protocol of HBOT can reverse amyloid plaques and prevent them from forming in the first place.
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a simple blood test available at Aviv Clinics may be able to answer this question: pTau Testing
Reverse Alzheimer’s? Study Shows HBOT Protocol May Reduce Amyloid Plaques and Boost Cognition
Researchers initially treated laboratory mice with hyperbaric oxygen therapy to understand its effect on amyloid plaques. In this first part of the study, researchers delivered HBOT to a group of mice whose brains contained amyloid plaques. The mice received two 60-minute HBOT sessions a day, five days a week, for four weeks. The researchers discovered that HBOT significantly reduced the amyloid burden in the mice’s brains, decreasing amyloid plaques by over 30% and shrinking plaques by nearly 19%.
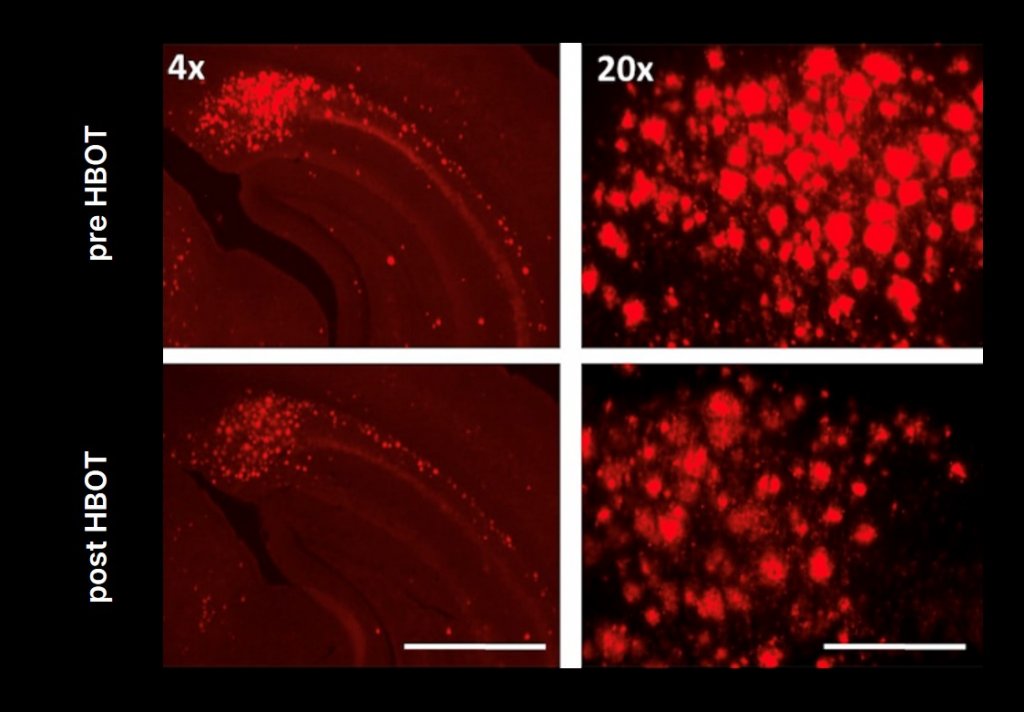
HBOT was also shown to prevent the formation of new amyloid plaques, and the mice exhibited improved performance on cognitive tasks when compared to the control group, providing evidence that HBOT improved their cognitive functions.
The rodent study gave promising new evidence that HBOT can be used as both a treatment and a preventative measure for Alzheimer’s disease. Researchers then sought to use the same protocol with human subjects.
The human test group consisted of six patients around age 70, all suffering from mild cognitive impairment. After receiving 60 daily HBOT sessions over three months, patients saw significant improvements in their cognitive functions. Improvements included better memory recall, concentration, and response times.
The researchers hypothesize that this is due to HBOT’s ability to increase blood flow in the brain. When the brain receives more blood, it receives more oxygen. And when the brain receives more oxygen, it can function at a higher capacity.
The Future of Alzheimer’s Treatment: Hope Through HBOT
The study offers hope that HBOT can one day be a viable drug-free method to prevent, treat, and even potentially reverse Alzheimer’s disease.
“By treating vascular dysfunction, we’re mapping out the path toward Alzheimer’s prevention. More research is underway to further demonstrate how HBOT can improve cognitive function and become an influential tool in the imperative fight against the disease,” affirms Dr. Shai Efrati, one of the investigators conducting the study.
Access the Only U.S. Clinic Offering this Alzheimer’s HBOT Protocol
Dr. Efrati is chair of the Aviv Medical Advisory Board. Aviv Clinics in central Florida is the largest and most advanced civilian HBOT clinic in the United States, and the only one that offers the study’s specific HBOT protocol as part of the Aviv Medical Program. This personalized treatment program uses comprehensive testing and assessments to help craft a treatment plan for each client. As part of the program, HBOT can be supported by other evidence-based therapies, including nutrition counseling, cognitive exercises, and physical training to optimize client outcomes.
For more information about the Aviv Medical Program, HBOT treatment, and how it may help your brain health, please contact us.
To read the study published in Journal Aging – click here.
Last Update: July 3, 2025
How Chronic Stress Rewires Your Brain
Many researchers and doctors would agree that stress can be as dangerous to the brain as drugs, and nobody is immune. We already know that stress over time makes you vulnerable to a number of adverse health conditions, but what about its impact on the brain in particular?
Until relatively recently, we thought that once a brain cell died, that was it — you were born with all of the brain cells you would ever have. Today, however, we know that isn’t the case. That was before we discovered neurogenesis (the formation of new brain cells) and neuroplasticity (the adaptive power of the brain). Our brains continue to grow and change over time, often in response to stressors.
Modern life presents a whole new challenge to the stress management systems of the brain, but there are ways to overcome the negative effects of stress.
What is Stress? Understanding the Body’s Response
While we often consider stress a negative sensation, stress itself is neutral: “your body’s response to anything that requires attention or action.” In other words, it’s how we respond to a stressor that determines its real flavor. Consider the feelings of excitement versus anxiety. One has a positive connotation, the other negative, but overall, they feel very similar. They are two sides of the same coin.
Most of the time, our bodies understand how to respond to a stimulus. In the interest of efficiency, the brain automates almost everything that it can. If you perform the same activities the same way every day, you probably don’t need to think about it much. That’s why you can get all the way home from work without any actual memory of the drive — your brain is essentially on autopilot.
The brain switches to a more active mode when it experiences something new and different. That’s when its problem solver, your cerebral cortex, gets involved. For example, if while you were on that drive home, a deer ran across the road in front of your car. Since that’s not “normal,” your brain immediately alerts your cortex, which instantly tells your foot to slam on the brakes.
It should be noted that not everything unusual is going to cause stress. Dropping your keys on the way out of the door might get your attention, but it doesn’t necessarily cause stress. According to Lazarus and Folkman, a stressful situation is one in which the demands on you exceed your current available resources. Stress occurs when you’re pushed past your limit, and you literally cannot handle more.
Luckily, the body has a response for that.
How the Human Brain Evolved to Handle Stress
Because stress is completely natural and expected, our bodies and brains have evolved accordingly to deal with threats.
For our hunter-gatherer ancestors, stress might have meant an immediate threat to their survival, like stepping on a poisonous snake. Their brains would have kicked the body into high gear to meet that threat.
Upon encountering a stressor, this ancient human’s brain would have immediately engaged the adrenal and autonomic nervous systems, which release adrenaline and cortisol into the bloodstream, which quickly floods the body and prepares it to do what it needs to do to survive.
Specifically, here’s how the brain and body respond:
- Increased heartbeat and respiration. You breathe quickly and shallowly into your lungs and the heart pounds, helping to oxygenate your blood and quickly supplying vital organs with nutrients.
- Increased energy. Your liver starts pumping glucose out to the bloodstream, instantaneously providing you with enough physical energy to do what’s needed.
- Systems prioritized. The brain coordinates a response that diverts the most energy and resources to the areas that need it, like your muscles. It also and tones down activity in less-than-essential systems, such as your digestive system.
- Tunnel-vision. Your pupils dilate, allowing more light in; this serves to improve your central vision, which is presumably focused on the current threat. Hearing and peripheral vision actually worsen in an effort to focus attention on the central threat.
You may have heard this referred to as the “fight or flight” response. It means that we’re highly adapted to deal with acute stress because stress management is wired into our DNA. Ostensibly, that’s a very good thing: We’re still here, so it seems it worked out for our ancestors fairly well.
When Stress Overloads the Brain’s Natural Defenses

While our brains haven’t changed much in the last 40-50 thousand years (a blink of the eye in terms of evolution), our lifestyles have changed drastically. Threats from wild animals have become threats of deadlines, traffic, bills, family conflict, and more. These modern stresses aren’t actually going to eat you alive, but your brain doesn’t necessarily understand that.
And so we’re faced with stressors almost constantly. While we’re wired well for acute stress, our brains haven’t caught up to cope with the onslaught of our present-day mental attacks.
Chronic Stress and the Breakdown of Brain Regulation
Stress management is mostly about how well you’re able to regulate your nervous system. The autonomic nervous system, the one that controls all of your involuntary functions, has two components. The sympathetic nervous system is designed solely for the fight-or-flight response mentioned above. It engages whenever a threat, real or perceived, is presented.
But you also have a parasympathetic nervous system, which is often called the “rest and digest” system. As you might guess, this system takes over when we’re not under stress. Its main job is to undo all of the changes the body undergoes when responding to stress; in other words, it helps you calm back down and “reset.”
The mismatch between our genetics and our environment means our alarm systems don’t work as intended. If the alarm system stays on all the time, or if something repeatedly triggers it, the end result is chronic stress.
How Long-Term Stress Impacts Brain Health
Stress and trauma are well known by now as contributing to a number of serious health conditions, including heart disease, stroke, and cancer. But how specifically does stress affect the brain?
Stress and Brain Rewiring in Mental Health Conditions
This probably isn’t surprising: Chronic stress can lead to mental health concerns. Doctors and researchers know, for example, that patients with PTSD have a pathological imbalance of grey and white matter in the brain. Researchers at UC Berkeley showed that chronic stress leads to a similar imbalance by creating more white matter that may lead to communication disruptions in the brain.
The study also showed how the brain may be literally rewired in some mental health conditions. Stronger neuronal and communication pathways between the hippocampus and the amygdala, for example, may lead to a quicker and stronger fear response. Conversely, less connectivity to the prefrontal cortex, where logical thinking and decision-making occur, can mean your emotional brain becomes the “louder” voice in your head that drowns out the thinking brain.
Can Stress Kill Brain Cells? What the Science Says
As mentioned before, neurogenesis, or the formation of new brain cells, can occur in the hippocampus, responsible in part for mood, memory, and learning. Chronic stress has been shown to slow down or impair neurogenesis. A recent study also confirmed that even acute stress affected not the formation of, but the survival of new neurons in the hippocampus.
How Stress Affects Memory and Learning
Think that getting older is having an effect on your memory? More than likely, it’s related to stress, not just age. Research has shown that even acute stress can affect your memory. Stress appears to affect both the formation of new memories as well as the retrieval of previously formed ones.
Interestingly, stress even appeared to affect your cognitive flexibility. Under stress, you’re less likely to “update” your memories or knowledge in light of new information, meaning stress could make you stubbornly stick to errant information.
3 Ways to Reset Your Stress Response and Protect the Brain

Stress is a fact of life. You can’t change it, but you can change how you react to stress. Here are three ways you can practice training your body to reset its stress response:
-
-
- Step 1: Recognize the Signs of Stress in the Moment
- Step 1: Recognize the Signs of Stress in the Moment
The first, and often hardest part of dealing with stress is simply recognizing that it’s there. Often, we unconsciously (or consciously) run from stress before we even have a chance to deal with it, often in less than healthy ways. But instead of running away or avoiding it, what about just looking at it? By stopping and just recognizing “oh, this is stressful” can go a long way towards diffusing the situation.
-
- Step 2: Notice How Stress Shows Up in the Body
- Step 2: Notice How Stress Shows Up in the Body
When we feel stress, we often carry it in our bodies. If you could do a mental inventory the moment you’re under stress, you’re likely to notice tense, raised shoulders, a tight belly and jaw, or various aches and pains. Everyone is different, and stress presents differently for each of us. But paying attention to where you actually physically feel stress in the body can help release it.
-
- Step 3: Shift Your Mindset Toward Resilience
Remember that stress is really neutral. It’s up to you to decide how you choose to deal with it. Modupe Akinola of Columbia Business School talks about a “contracted” stress response versus a “flow state” response. A contracted response would be to pull back, avoid, and withdraw. A more open state is like that of athletes or musicians during a game or performance. Both are heightened states of arousal and attention, but with different attitudes held towards them.
-
Yes, Stress Changes the Brain — But So Can You
Both acute and chronic stress can affect the brain as well as the body. Even though we know now that brain cells can be restored, it’s important to learn to deal with the ever-present stress that inevitably affects our lives. By learning to respond more positively to stress, we can help the body and brain recover and heal.
Keep going! Learn about cortisol (the stress hormone), stress management, and the connection between nutrition and stress.
Last Updated July 2, 2025
Understanding Chronic Pain: Causes, Treatment Options and Non-Opioid Relief Strategies
Chronic pain is one of the most common reasons why people seek medical care today. It’s also a leading cause of disability. Chronic pain can be debilitating when it’s severe enough. Many people who suffer from it experience a loss of mobility, leaving them unable to leave their homes or even their beds. While chronic pain this intense is rare, even less severe pain can leave you unable to enjoy activities you once loved, potentially leading to isolation and mental health problems like depression.
According to the CDC, nearly 1 in 5 adults in the United States suffers from chronic pain. The older population is hit especially hard because the risk of chronic pain increases with age. Adults aged 65 and older experience the most chronic pain of any demographic. Older adults are also more likely to experience high-impact chronic pain, or pain that affects a person’s daily life, work, socializing, and self-care.
Fortunately, there is hope. While the medical community is still learning about chronic pain, scientists are gaining more knowledge every day. Physicians are learning how to treat it effectively, so that those who suffer from it can live full lives.
What Is Pain? Understanding the Body’s Natural Response

In its most basic sense, pain is a sensation of discomfort created by the brain in response to unpleasant stimuli. If you stub your toe on a table leg, the nerve endings in your toe will send a signal to your brain, telling the brain that it’s been hurt. The brain then emits a signal back through your body, which you experience as pain.
This particular type of pain is known as acute pain.
Acute pain is a survival mechanism. If you never felt pain, then you would not know that your body was injured. For example, if you were to get a cut to the back of the thigh, you couldn’t visibly see your injury. Without pain signals from the brain, how would you know that your body had suffered an injury? You could die of an infection before you realized anything was wrong.
Acute pain is nature’s way of making us pay attention to our injuries. It alerts us to stop and take care of ourselves before we suffer further harm. Fortunately, acute pain like this usually disappears once the injury has healed. Chronic pain, on the other hand, is a different story.
What Is Chronic Pain and Why Doesn’t it Go Away?
Unlike acute pain, chronic pain persists after an injury or illness heals. By definition, chronic pain lasts for at least three months, but outbreaks can last for months or years, with no signs of disappearing. The sensation can vary from sharp and stabbing, like a migraine, to dull and throbbing, like an ache in your bones.
Everyone experiences chronic pain in different ways. There is no standard sensation or unifying characteristic.
This is why the classic 1-10 “pain scale” isn’t always an effective tool to gauge how much pain a person is suffering. Pain is a subjective experience, and we all have different pain thresholds. To complicate matters, chronic pain can come from multiple sources, as well.
Common Causes of Chronic Pain in Adults

-
Chronic Pain After Injury: When Acute Pain Becomes Long-Term
Chronic pain may be caused in response to acute pain, like a lingering ache in your back after rupturing or pulling a disc. Doctors and patients alike often mistake chronic pain for acute pain at first, because it may appear that chronic pain is simply the re-emergence of an old injury. But chronic pain is a pain that has taken on a life of its own.
Researchers are making progress towards understanding why acute pain sometimes shifts into chronic pain. In chronic back pain, for example, studies have identified risk factors like “…higher pain intensity, higher body weight, carrying heavy loads at work, difficult working positions, and depression.”
-
Chronic Pain From Illnesses Like Arthritis and Fibromyalgia
Just like with acute pain, chronic pain may be brought on by a condition like Lyme disease, fibromyalgia, sciatica, or arthritis. Older adults are more likely to suffer from chronic illnesses than younger adults. Common side effects of chronic illnesses include fatigue, aches, migraine, and nerve pain.
Certain types of cancer can also cause chronic pain. Tumors can put pressure on nerves or release chemicals that irritate nerves. Cancer treatments, like chemotherapy or surgery, can also produce a chronic pain response.
-
The Link Between Chronic Pain, Depression and Anxiety
Chronic pain is also common in people who suffer from mental health conditions like depression and anxiety. It’s not currently clear whether depression itself causes chronic pain or if chronic pain causes depression. Given what we know about the mind-body connection, however, it’s likely that having one condition can worsen the other.
If you feel depressed, then you’re more likely to experience chronic pain more intensely. If your pain is so intense that you can no longer leave your home, then your depression can worsen from the isolation, creating a vicious cycle.
-
When Chronic Pain Has No Clear Cause
Sometimes, there’s no clear cause for chronic pain at all, which can be all the more frustrating for someone who suffers from it. It’s easy for someone with chronic pain to feel powerless in the world around them. However, that doesn’t have to be the case. There are plenty of different ways to manage chronic pain without addictive medications like opioids.
Non-Opioid Treatment Options for Chronic Pain Relief

In the past, it was common for doctors to prescribe opioids as a solution for patients with chronic pain. These medications can be effective against short-term acute pain, but using opioids alone is unlikely to give you the relief that you want. Even more concerning, however, is that opioids are extremely addictive. Using them for too long can create a dependence that can put users at risk for dangerous side effects and deadly overdoses.
Holistic Pain Management: A New Path to Relief
The most effective way to manage chronic pain is through a multi-pronged approach of proper nutrition, physical activity, and psychological aid.
Studies also indicate that hyperbaric oxygen therapy (HBOT) can benefit patients experiencing chronic pain from fibromyalgia and myofascial pain syndrome. In these studies, patients experienced improvements in pain threshold and quality of life, as well as decreased disability, after an HBOT treatment program. Patients of the Aviv Medical Program, which can include an evidence-based HBOT protocol among other therapies, have experienced relief of chronic pain from conditions like fibromyalgia. HBOT, when combined with nutritional guidance, physical activity, and cognitive coaching in the Aviv Medical Program, can be a life-changing treatment for chronic pain conditions.
Read more about how to manage chronic pain without medications.
Real Stories of Chronic Pain Relief: How Greg Found Hope with the Aviv Medical Program
When fibromyalgia pain affected Greg, he not only needed to quit his job, but struggled to even get out of bed on some days. Some treatments helped, but the side effects often left him with brain fog and other cognitive challenges. For more than 20 years, he sought a better solution. Since completing hyperbaric oxygen therapy and other interventions in the Aviv Medical Program, his pain is under control. Greg says he’s once again living his life naturally, instead of fighting his way through life with the chronic pain of fibromyalgia.
Contact us to determine if the Aviv Medical Program can be a suitable treatment for your chronic pain.
Last Update: July 2, 2025
Can High Blood Pressure Cause Memory Loss?
Understanding the Link Between Hypertension and Cognitive Decline
We all know that high blood pressure can cause a host of health issues, although most of us are unaware that high blood pressure can cause memory loss. Cognitive decline is a side effect that isn’t always discussed. But having high blood pressure can directly affect your cognitive function, causing problems like brain fog and forgetfulness, as well as severe cognitive issues like vascular dementia.
Nearly one in three Americans and two-thirds of adults age 60 and older have high blood pressure, making it one of the most common chronic conditions in the U.S. Fortunately, there are actionable steps you can take to manage your blood pressure and overall healthspan, no matter your age.
Treatment options such as the Aviv Medical Program, which may include a unique, evidence-based hyperbaric oxygen therapy (HBOT) protocol, target associated health challenges like age-related cognitive decline, post-stroke challenges, long COVID and more. Keep reading to learn more about how high blood pressure can cause memory loss.
What is High Blood Pressure and Why Does it Matter for Brain Health?

Also called hypertension, high blood pressure occurs when the force of the blood pushing against the walls of your blood vessels is too high.
Every blood vessel in your body requires a certain amount of pressure to stay intact. High blood pressure may damage arteries, making them less elastic. Lower elasticity slows blood and oxygen flow to vital areas of the body. Health problems happen when your blood pressure wanders outside the acceptable range.
The higher your blood pressure, the greater your risk for health problems like heart disease, heart attack, and stroke. It also increases your risk of cognitive problems later in life.
What is a Normal Blood Pressure Range?
Normal blood pressure levels differ for every person and depend on age, weight, and other factors. According to the American College of Cardiology and the American Heart Association:
- Stage 1 hypertension occurs at 130/80 mm Hg
- Stage 2 hypertension occurs at or above 140/90 mm
High blood pressure is unique because it doesn’t present symptoms on its own. The only way most people discover that their blood pressure is high is when something more serious happens. The best way to learn whether your blood pressure is at a healthy level is to measure it with a blood pressure machine at a doctor’s office, pharmacy, or on a home blood pressure machine.
Tip: A home blood pressure device is a worthwhile investment to monitor your health. Take your measurements at the same time every day for consistency, as your blood pressure will naturally rise and fall during the day.
How High Blood Pressure Affects Brain Function and Memory

The brain receives roughly 20–25% of the body’s blood supply. When high blood pressure causes this supply to decline, the brain lacks the nutrition it needs to perform optimally.
High blood pressure can also harm the tiny arteries that feed white matter, the wire-like cells that transfer information to different brain areas. These issues may manifest as memory problems, confusion, lack of concentration, and other side effects.
The Link Between Hypertension and Cognitive Decline: What the Research Says
Age-related cognitive decline studies show that having high blood pressure during midlife can affect cognition later in life. We’ll let these research studies help clear the fog on the link between the brain and blood pressure:
- In a 1995 study on midlife blood pressure levels and late-life cognitive function, men at an average age of 78 years completed cognitive tests. Those who had high blood pressure in middle age performed most poorly on cognitive tests, even after adjusting for biases like prior education and age. This suggests a direct connection between hypertension and cognitive decline later in life.
- More recent studies, including this 2020 study of both men and women, have helped to reaffirm the connection between hypertension and cognitive decline.
- Researchers have found that the top two cognitive skills affected later in life are mental processing speed and executive function.
Understanding Vascular Dementia and High Blood Pressure
High blood pressure directly increases the risk of developing vascular dementia, a type of dementia caused by blood flow problems in the brain from strained blood vessels. The strain on the blood vessels makes it difficult for the brain to get the oxygen needed to function correctly.
Fortunately, vascular dementia symptoms can be improved through hyperbaric oxygen therapy (HBOT), such as the protocol used at Aviv Clinics in central Florida. HBOT works by delivering oxygen directly to the brain in a pressurized environment. The direct supply of oxygen improves cellular metabolism and sparks angiogenesis, the growth of new blood vessels, in your brain. Researchers propose that these actions can help you regain cognitive function.
How to Manage High Blood Pressure to Support Brain Health
While medication is often the first thing people think of, investing in your health through preventive care and lifestyle changes is essential to managing high blood pressure.
The following lifestyle interventions can help reduce hypertension and improve brain health:
- Eat a clean diet of whole foods to promote your gut health.
- Exercise to help maintain or manage your weight.
- Get enough sleep by establishing a bedtime routine, and turning off the TV.
- Engage your mind by gardening, reading, or even playing a video game with your kids or grandkids.
- Reduce and manage your stress levels with activities like yoga or meditation. Practicing mindfulness meditation can help you stay grounded in the present moment and reduce stress.
- Seek unique and comprehensive therapies, such as hyperbaric oxygen therapy (HBOT). Research-backed HBOT programs, such as the one offered as part of the Aviv Medical Program, encourage damaged vessels to heal and cognitive functions to improve. The evidence-based Aviv Medical Program is a personalized regimen based on your goals, needs and unique physiology. It may include HBOT, cognitive exercises, dietary coaching, and physical performance training. This personalized, holistic approach has been key to restoring our patients to optimal health.

Find Hope and Healing at Aviv Clinics
While high blood pressure is dangerous, especially later in life, it is possible to manage it. It’s never too late to start, even after a cognitive decline diagnosis.
If you’d like more guidance, reach out to the Aviv Clinics team.
Last Updated July 1, 2025
Brain Games: How Cognitive Training Enhances Brain Health
Monopoly, Minecraft, solitaire, bridge: Games are often associated with fun times and good memories. Young or old, we love games for the challenge, the excitement, and the enjoyment that they bring us.
But could playing games also boost your brainpower?
The innovative Aviv Medical Program includes the use of cognitive training (aka “brain games”) to help enhance cognitive functioning. Continue reading to learn why brain training is an important part of our proprietary program.
How the Brain Works — and Why It Needs Cognitive Training
The brain is a remarkable organ, but we don’t often think about everything our brain helps us to do. Something as simple as making a pot of coffee in the morning, when viewed from the brain’s point of view, can get quite complex. The brain has to stir your consciousness, fire the right neurons that direct your muscles to move the right way to get you out of bed, get dressed, make your way to the kitchen, and make some coffee.

There is a reason why we don’t think about this process very often; our brain goes to remarkable lengths to make sure you don’t get overwhelmed with too much information. Much of what we do is part of a routine, and the brain likes it that way because it can conserve energy. As we evolved, it was beneficial for the brain to be “lazy” and automate as much as it could, so that it could focus on our survival.
Nowadays, however, with our basic survival needs generally met, the brain doesn’t have as much to worry about. Much of the learning and growing that the brain experiences tends to happen earlier in life, and as we age, our brain focuses more on using existing skills rather than learning new ones. Although it makes things easier for the brain, it’s also how the brain ages and loses neurons. Conditions such as stroke and challenges like brain fog can also worsen cognitive decline.
Neuroplasticity and Aging: The Brain Can Grow at Any Age

For years, scientists agreed that, unlike many cells in our body that repair or replace themselves when damaged, when brain cells died, they didn’t come back. This turned our neurons into a precious finite resource. We thought that learning was primarily a process for the younger brain. Today, we understand neuroplasticity of the brain — that it brain can still grow, learn, and change at any age.
Consider how a muscle grows bigger and stronger. Remember what happened the last time you did something physical that made you really sore? You might have thought, “I didn’t even know I had muscles there.” Muscles get sore because they’ve been challenged by something they’re not used to doing.
The brain learns and grows in almost exactly the same way.
When the brain does the same routine activities every day, it’s the mental equivalent of sitting on the couch all day.
But when the brain encounters something new or challenging, it can learn and grow. Novelty spurs the brain to form new neurons and neuronal connections, building networks of brain activity much the way muscles build muscle fibers.
Boosting Brainpower Through Cognitive Challenge and Novelty
Any activity that’s new, exciting, or challenging for the brain has the potential to build brainpower and even improve cognitive function.
The brain was designed to solve problems and devise solutions to previously unasked questions. When it encounters things that it’s never experienced, our learning process kicks in.
Gaming is a great way to shake things up for your brain without having to abandon the familiarity of your favorite routines.
If you’re wondering if games are a good way to train the brain, you’ll be happy to hear that data shows cognitive training can improve quality of life and ward off cognitive decline. Dietary changes and exercise can also help.
Clinical Evidence: What the ACTIVE Study Says About Brain Training
The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) trial was designed on the premise that cognitive function can be trained and may improve health outcomes and quality of life for older adults. The study aimed to show the actual practical impact that cognitive training can have on daily life.
The study targeted three areas of cognitive function that start to decline on average in the mid-60s: reasoning, memory, and processing speed. A group of 2,802 adults aged 65 and older participated in the study. The treatment group received a total of 10 training sessions lasting 60-75 minutes each, over a period of five weeks. A control group received no training. A select group from the treatment group was also given “booster” training sessions 11 and 35 months later.
To determine the effects of the training, the participants were rated as they performed activities of daily living. These included getting dressed, preparing meals, shopping, managing finances, and so on. Subjects were rated on how independently the tasks were completed and the perceived level of difficulty. Additional computer-based tests analyzed participants’ reaction time as they responded to changing traffic signs.
The study also looked at secondary measures, including improvements in health-related quality of life, the impact on mobility and incidence of falls, and whether driving was affected.
ACTIVE Trial Results: Real-Life Benefits of Brain Training for Older Adults
The study found that all areas of cognitive function measured — speed, memory, and reasoning — showed immediate improvement as a result of the cognitive training.
Although some of the improvements dissipated by the end of the follow-up period, the training group still showed a significant improvement over the control subjects five years later. The booster groups that received additional training saw even better improvements.
The treatment group also reported significantly less difficulty in performing daily tasks. The results for self-reported quality of life were also better for the treatment group than for the control group.
Overall, participants in the treatment group had less difficulty performing functions of everyday living and reported better quality of life. Training also positively impacted driving abilities, including fewer 50% fewer at-fault accidents reported.
What Games Improve Cognitive Function in Older Adults?

The ACTIVE study shows the clear positive impact of cognitive training, and playing games is one of the best ways to train the brain.
Of course, not all games are created equally. While all engage the brain on some level, there are some specific brain functions one should ideally target.
What should you look for in a game?
Cognitive training at Aviv Clinics currently utilizes a platform called BrainHQ. One of the games, Double Decision, is a speed training game based on the intervention used in the ACTIVE study.
In Double Decision, the object is to spot an object that flashes in the middle of the screen while simultaneously tracking a second object that flashes in your peripheral vision. The player must then remember both the object in the center and the location of the other item. The game is designed to scale in difficulty as you improve by adding distractions to further challenge the brain.
Enjoyment Matters: Choosing Cognitive Activities You’ll Stick With
Although BrainHQ uses games that are optimized for the cognitive skills most in need of training, it’s important not to get too hung up on finding the “best” games for your brain. The truth is that the best games are the ones that you’ll play. After all, even the best game won’t do your brain much good if you never play it.
Focus on finding ways to challenge your brain that you enjoy and can ideally complete regularly. And feel free to change it up, too — the brain thrives on novelty! Whether it’s a crossword or sudoku puzzle on your own, a game of chess with a friend, or your grandkid’s latest VR video game, there are endless ways to have some fun while training your brain.
The Aviv Medical Program: Enhancing Brain Performance Through Cognitive Training
Aviv Clinics combines cognitive training with hyperbaric oxygen therapy and other personalized interventions to promote neuroplasticity and cognitive resilience. As the only U.S. location offering the unique, evidence-based Aviv Medical Program, Aviv Clinics in central Florida empowers you to optimize your brain health with lasting results.
Based on nearly two decades of research and development, the intensive treatment program is customized to each client’s needs. Using in-depth assessments, our physicians prescribe a personalized plan for each client.
For a free consultation with one of our board-certified physicians, contact us.
Last Update: July 1, 2025
How Stress Affects Gut Health: 5 Tips for Gut and Brain Health
The human gut is an amazing entity. Our gastrointestinal (GI) tract is home to a vast network of nerves, neural transmitters, and thousands of different microflora that keep our bodies up and running. It’s so complex that scientists sometimes call it “the second brain.” It’s no surprise that stress and gut health are closely connected. Your gut can influence your moods just as much as your brain, too. Scientists are still learning how this incredibly complex system works. We do know, however, that because the brain and gut interplay with each other, changes in one can affect the other.
High levels of stress in your body can inhibit digestion, lower your immune system, and even lead to the breakdown of your intestinal lining. This can cause short-term problems like diarrhea, heartburn, gas, and stomach pains. It can also lead to more severe problems later on, like leaky gut syndrome or IBS. That’s why it’s essential to keep your stress levels under control if you want to improve your gut health.
As a center dedicated to improving cognitive health and performance, Aviv Clinics understands the importance of proper nutrition for brain health. Here’s what you need to know about stress and the brain-gut connection, along with our best tips for keeping your stress levels low and your gut bacteria content.
The Brain-Gut Connection: How Stress Affects the Digestive System
Scientists have barely scratched the surface in understanding how the brain and the gut communicate to affect our moods. But here’s what we do know. Our digestive tract is home to thousands of different species of microbes, all working together. This complex system works to break down the nutrients in our food, keep our immune system strong, and produce hormones that keep our bodies operational. And what you put into your gut can directly affect how you feel.
How Stress Impacts Your Digestive System
Serotonin, the happiness hormone, is actually produced in the gut. It’s created by breaking down the essential amino acid tryptophan and is sent to your brain via the vagus nerve. Tryptophan is found in many whole foods like fruits, vegetables, meats, dairy, and seeds. It’s one of many ways that a healthy diet can help you stay happy.
But there’s another hormone your body produces that doesn’t always make you feel good: cortisol. When your body experiences stress or discomfort, your brain triggers the adrenal gland to release cortisol, the stress hormone. Excess levels of cortisol have been linked to everything from weight gain and gastrointestinal problems to a suppressed immune system and cardiovascular diseases.
We can’t always control stress, but we can take control of how we react to those stressors. Adopting healthy habits can help lower your cortisol levels naturally, helping you heal both your brain and your gut.
5 Gut-Friendly Tips to Reduce Stress Naturally
1. Eat Whole Foods to Support Your Gut Microbiome
The number one thing you can do to keep your gut thriving is to eat a diet filled with whole foods. The highly processed foods found in our Western diet lack the necessary nutrients and fiber our gut microbes need to stay healthy.
This can lead to the death of our healthy microbes, weakening your immune system and leaving you susceptible to disease. Whole, unrefined foods like fruits and vegetables are the perfect fuel for your gut’s vast network of microflora. Their rich quantities of fiber promote proper digestion to keep your gastrointestinal tract working properly, and a happy gut usually leads to a happy mind. It’s also important to understand the difference between good and bad sugars.
2. Avoid Stress Eating and Gut Inflammation
When we’re feeling stressed, the first thing most of us do is reach for our favorite candy or snack food to fill the void. It’s called stress-eating, and it’s a common coping mechanism for the chaos in our modern world. But although that burst of satisfaction feels good in the moment, eating sweets can exacerbate your stress-induced stomach issues in the long term.
Foods high in refined sugar and unhealthy fats increase inflammation in the body. This sends your stress levels even higher. While there is something to be said for finding comfort in your favorite foods, stress-eating usually means you aren’t taking the time to properly enjoy your food. There’s a big difference between eating one cookie as a treat versus five because you’re eating your feelings.
The next time you find yourself craving a brownie after a stressful conversation, remember that eating sugar will only stress your belly even further. Save your indulgences for times when you can actually enjoy them instead.
3. Meditate to Calm Both Brain and Gut
The brain and the gut are so intricately connected that calming the brain can also calm the gut. Practicing mindfulness meditation can lower levels of cortisol in the body. These lowered stress levels can lead to improved digestion, which keeps your gut in good shape.
Taking the time to clear your mind of life’s worries can also help you be more calm and understanding in your daily life. Mindfulness meditation practices have even been proven to help with depression and anxiety. Try meditating for just a few minutes a day and see if you feel any improvement in your nervous stomach. Here is more on meditation to get you started.
4. Exercise to Reduce Cortisol and Improve Digestion
Working up a sweat is also an excellent way to deal with stress. In addition to obvious benefits like weight loss and stronger muscles, exercise triggers the release of serotonin, which can lower stress levels. Even a 20-minute stroll outside can do the trick to get the serotonin flowing. Just be careful to pace yourself, and be sure not to overdo it.
5. Improve Sleep to Support Stress and Gut Health
Sleep is the essential period when our bodies take time to recharge every day. Getting a good night’s rest can improve your cognitive performance and help fight off Alzheimer’s disease. Getting adequate rest is also important for lowering stress levels.
You can also improve the quality of your sleep by improving your diet. Eating foods high in tryptophan helps your gut produce serotonin and also leads to the production of melatonin, the sleep hormone. Higher levels of melatonin can dramatically improve the quality of your rest, which can help lower stress in your body. If you want to get a better night’s sleep, try eating more fruits and vegetables during the day.
The Link Between Stress and Gut Health: Final Thoughts
Stress and gut health are closely linked. Eating healthy, whole foods is an effective action to reduce your stress levels and stomach issues. Treats may be enjoyed in moderation, but not to fill an emotional void or coping mechanism for stress.
Aviv Clinics delivers a highly effective, science-based treatment program to enhance brain performance and improve the cognitive and physical symptoms of conditions such as traumatic brain injuries, fibromyalgia, post-stroke, and mild cognitive impairment. The Aviv Medical Program can incorporate a physician-guided program of evidence-based therapies, including a peer-reviewed hyperbaric oxygen therapy protocol, nutrition management, and other interventions to promote recovery. Based on nearly two decades of research and development, the Aviv Medical Program is personalized to meet the needs of each client.
To discover if the Aviv Medical Program is right for you, please contact us for a free physician consultation.
Last update: July 1, 2025
How Sugar Affects the Brain: What You Need to Know about Natural and Refined Sugars
How Does Sugar Affect the Brain?
From the Paleo diet to the Mediterranean diet to the ketogenic diet and beyond, there’s one thing that nearly all modern diets agree on—if you want to maintain a healthy body and mind, cut out sugar.
While there’s wisdom in this advice, blanket statements like “cut out sugar” can leave room for confusion. It leaves many people wondering, is all sugar bad for you? Should you avoid sugar in any form, including in fruits? What about carbohydrates found in fruits and vegetables?
With so many complicated questions like these and no clear answers, it’s no wonder many people feel confused. As a center dedicated to improving brain health and performance, Aviv Clinics understands the importance of proper nutrition and its direct effect on cognitive and physical functioning.
Let’s examine sugar in detail and clarify what dietitians mean when they tell you to “cut out sugar.”
Is All Sugar Bad for Your Brain? Understanding Natural vs. Refined Sugar
Not exactly—foods with high amounts of sugar can still be healthy. For example:
- While apples contain lots of sugar, they also supply water, vitamins, nutrients, and dietary fiber that are vital for a healthy body. Dietary fiber is essential for maintaining a thriving wealth of gut flora. Gut flora builds our immune system and fights off ailments like leaky gut disease.
- You can find natural sugars in many whole foods. They also come in many different chemical forms, including glucose from carbohydrates. Glucose provides our bodies with energy, helping fuel our muscles and vital organs as it circulates throughout the bloodstream. We wouldn’t be able to function normally without the glucose we gain from consuming carbohydrates.
Does The Brain Need Sugar to Function? Glucose and Brain Health
Although the brain can use alternative fuel sources, such as ketones, for fuel if you’re insulin resistant, glucose is the brain’s preferred fuel source. The brain relies heavily on glucose when performing complex tasks.
So when you’re concentrating extra hard on a crossword puzzle or a complicated passage in your favorite book, your brain is burning glucose over time to help you get the job done. If your blood sugar dips too low, you can experience problems like brain fog or trouble concentrating. It’s your brain’s way of telling you that it needs more fuel and that you should grab a healthy snack.

Natural Sugar vs. Refined Sugar: What’s Healthier for Brain Function?
While natural sugar naturally occurs in foods, refined sugar is a processed substance.
How the Body Processes Natural Sugar
When you eat an apple, your body does all the work of processing the unrefined fruit into digestible nutrients all on its own.
First, you must chew the apple, breaking it down into apple sauce. Then, your gut does the hard work of absorbing the vital nutrients and breaking down the sugar to circulate it through your bloodstream.
The leftover fiber is used to nourish your gut’s network of microflora. When you eat whole foods, your body is the factory, and the natural sugars in your foods are the fuel that runs it.
What Refined Sugar Does to Your Body and Brain
Foods with refined sugar are a different story. Candies, cookies, chips, and other pre-packaged snacks don’t offer your body the same fuel as whole foods. Your body doesn’t have to go through the work of breaking down these highly processed foods—the factory already did it for you.
Processed foods are loaded with refined sugar without any of the nutrients, vitamins, and fiber your body needs. This leaves your gut flora starved of the materials required to function and your immune system vulnerable.
How Too Much Sugar Affects the Brain and Cognitive Performance
It’s possible to have too much of a good thing. Modern Western diets are filled with refined sugar and carbohydrates in the form of ready-made snacks, treats, and processed foods.
Thus, you may feel sluggish once the “sugar high” wears off. Eating too much sugar can also make you susceptible to health conditions like type 2 diabetes.
The best way to limit refined sugar intake is to lean on a natural diet consisting of whole foods.
Sugar and the Brain: Effects on Memory, Mood, and Brain Fog
Excessive sugar intake can impact specific neurotransmitters and bring on memory deficiencies. Among these neurotransmitters is dopamine, the chemical controlling mood, behavior, learning, and memory.
Here’s what research studies further illustrate:
- When rats were fed a high-sugar diet that resembles the average Western diet, their cognitive performance suffered. The rats struggled to complete tasks that relied on their memory. Their struggles suggest their diets were directly responsible for impairing their brains’ prefrontal lobes and hippocampus regions.
- Eating a diet high in sugar can reduce the production of a chemical called “brain-derived neurotrophic factor” (BDNF). This chemical is active in areas of the brain vital to learning, memory, and higher thinking. Low BDNF levels are associated with poor memory function and are linked with Alzheimer’s Disease and dementia.
- Experiments in both laboratory animals and humans have revealed that when the brain needs an extra power boost, blood vessels in the brain dilate to deliver more glucose and oxygen through the bloodstream.
Why the Brain Needs Glucose (And How to Get it From Healthy Foods)
Yes, natural sugars perform a vital role in energizing the body and mind. The body requires a total of 200 grams of sugar or glucose each day. Two-thirds of this, or 130 grams, is used by the brain to help you function to your best ability.
The key takeaway from the information we presented above is this: incorporating a diet filled with natural, whole foods is essential to:
- Nourishing your body with the right type of sugar
- Enhancing cognitive and physical performance
4 Smart Ways to Reduce Refined Sugar and Improve Brain Health
The natural sugars found in whole foods are nothing to fear. Eating a diet with enough carbohydrates and natural sugars is vital for keeping your body and brain healthy.
Here are a few ways to stay on track:
- Make sure the bulk of the sugar you consume comes from whole foods like fruits and vegetables, not processed junk foods.
- Just because a food is labeled “sugar-free,” that’s not always the case. It may be true that a food doesn’t contain added sugar, but remember that carbohydrates turn into glucose in your body.
- You can rack up carbohydrates quickly on a typical day. Try to aim for around 45 total carbs at every meal if you’re a woman or 60 at every meal if you’re a man. You’ll be surprised how quickly you can meet that quota with just a handful of whole foods!
- You don’t have to cut out refined sugar altogether. Obsessing over eating a “perfect” diet only stresses you out and doesn’t leave any room for you to feed your soul. Do you plan on spending a relaxing afternoon baking with your grandkids? Go ahead and treat yourself to a warm cookie fresh from the oven.
If you’re eating healthy at most meals, there’s no need to feel guilty about indulging in rich foods now and then. Just be smart about it, and always make conscious decisions about what kind of foods you put into your body.
Enhance Brain Performance With the Aviv Medical Program
Aviv Clinics delivers a highly effective, science-based treatment protocol to enhance brain performance and improve the cognitive and physical symptoms of conditions such as traumatic brain injuries, fibromyalgia, mild cognitive impairment, long COVID, and others. The Aviv Medical Program’s intensive treatment protocol features Hyperbaric Oxygen Therapy and can include interventions like nutrition management and support for better brain health. Based on nearly two decades of research and development, the Aviv Medical Program is customized by our physicians to meet your needs.
Contact us to speak with a Client Ambassador about the Aviv Medical Program
Last update: June 30, 2025
Brain Fog Causes, Symptoms, and Treatments
“I feel I’m just getting by on autopilot. I feel delayed with my actions and reactions to questions and situations.”
“It’s almost identical to what I go through when I’m awakened from a dream–just total bewilderment and almost complete inability to process anything that’s going on.”
“Sometimes I am very far off. I’ll pause and get confused in the middle of doing things. I’m drowsy all the time and just don’t know what’s going on.”
“I feel heavy on the front of my head, unrefreshed, similar to a hangover or jet lag.”
“I feel like Dory in Finding Nemo.”
If any of these sound familiar, then you know what “brain fog” feels like. Brain fog is a symptom, not a diagnosis or disease. It leaves a person temporarily unable to concentrate or think clearly.

Not all brain fog is created equally: Anything from stress to dehydration to a urinary tract infection (UTI) can cause mild, temporary brain fog. COVID-19 has contributed to a particular kind of brain fog seen in “long-haul” COVID cases. Fibromyalgia patients often complain of “fibro fog” and cancer patients undergoing chemotherapy can experience “chemo brain.” Regardless of the cause, the forecast for the brain remains the same: foggy, forgetful, and fuzzy around the edges.
Fortunately, new treatments, such as the Aviv Medical Program, which can include the world’s most advanced hyperbaric oxygen therapy (HBOT) protocol, may offer relief from brain fog. Understanding brain fog symptoms and causes can help you take charge of this challenging cognitive condition.
What Is Brain Fog?
Brain fog describes a feeling of confusion and forgetfulness, as well as a lack of mental focus. The effects of brain fog can range from mildly annoying to completely debilitating. It can last hours, days, or even weeks, depending on the root cause of the brain fog.
What Symptoms Accompany Brain Fog?
Brain fog can encompass a combination of cognitive and emotional symptoms. A person with cognitive symptoms usually has difficulties with attention, concentration, learning, and memory. This can manifest differently across individuals, but often looks like:
- Struggling with multitasking
- Feeling like you’re in a dream or disconnected from reality
- Forgetting details of a recent conversation
- Having a hard time concentrating and absorbing information
- Being easily distracted
Brain fog can also make you feel emotionally unwell. After all, not being able to put your best foot forward in daily activities can be discouraging.
You might:
- Feel frustrated and helpless
- Experience irritability or mood swings
- Feel more stressed than usual
During these difficult moments, it’s important to be kind to yourself. We’re humans, not robots. Understanding that these feelings might be linked to a medical condition is the first step to regaining optimal cognitive and mental health.

How Does Brain Fog Impact Daily Life?
Most of the time, it feels like we’re in control of our lives, and we want it to stay that way. But with brain fog, that journey grows complex. While it’s easy to brush it off, hoping “it will subside in no time,” the reality is that the brain doesn’t just impact your emotional well-being—it also impacts the circumstances and individuals surrounding you.
- Professional challenges: When we spend “one third” of our lives at work, brain fog can surely creep into the professional realm. Getting tasks done on time or staying attentive during training and meetings feels harder than usual.
- Strained personal relationships and social interactions: Building and maintaining genuine connections with loved ones requires equal investment on both sides. Brain fog can cause an imbalance, making it difficult to keep up with social interactions and stay fully invested in relationships.
- Decline in emotional well-being: Living with brain fog can become emotionally and cognitively draining. Knowing you’re not your best self can make you feel detached from your surroundings. As this starts to impact your performance and relationships, daily activities may grow even more overwhelming.
- Safety risks and implications in daily activities: Since brain fog may make you less attentive than usual, it can expose you to unsafe situations. Examples include making less careful decisions and not watching where you’re going.

One way to take back control of your life is by learning brain fog causes. Doing so will help you understand yourself better and, more importantly, give you the strength, expertise, and courage to pursue the right solutions.
What Causes Brain Fog?
Brain fog isn’t a specific medical diagnosis but a side effect of lifestyle factors and emotional or medical conditions.
The common reasons why your brain feels foggy might include:
- Stress—Stress impacts the entire body, inclufing and especially the brain. When stress becomes chronic, high cortisol levels can negatively affect the brain, inhibiting it from optimal function.
- Lack of sleep—Another obvious but often overlooked cause of brain fog is lack of sleep. Sleep deprivation causes “cognitive lapses.” Brain cells have difficulty communicating with one another, resulting in a lack of focus or clarity. More severe sleep issues, such as sleep apnea, can also cause brain fog and cognitive decline.
- Hormones—Menopause is known for wreaking havoc on the brain. Menopausal and postmenopausal women were reported to “show gradual declines in cognitive performance.” The drop in estrogen levels can trigger memory and concentration issues. Hormonal changes are also known to exacerbate sleep deprivation, which may contribute to brain fog. Learn more about menopause and brain health.
- Diet—When your brain isn’t provided with quality nutrition, it doesn’t have the fuel it needs to function optimally. Harvard Health notes there is a link between “a diet high in refined sugars and impaired brain function.”
- Medications—Medications, especially psychiatric drugs and antibiotics, can “affect memory and cognitive function.” This impact on brain performance is especially common in older adults whose metabolic processes are slower, making them more sensitive to medications.
- Mental health disorders—Disorders like depression can “reduce cognitive functions,” which may cause brain fog. An individual may feel fatigued, dissociated, and hopeless.
- Long COVID—The CDC lists brain fog as one of long COVID’s neurological symptoms. COVID-19 can attack the brain in ways that may cause post-COVID brain fog. If your cognition has not been the same since your COVID-19 infection, we recommend speaking with a physician.
- Environmental toxins—Exposure to chronic “traffic-related pollutants may increase the risk of neurological disorders.” Additional research notes that “exposure to environmental toxins, such as cigarette smoke, polluted air, and pesticides, can negatively impact brain health, leading to cognitive decline and an increased risk of neurodegenerative diseases.”

What Chronic Conditions Cause Frequent Brain Fog?
People who have myalgic encephalitis, chronic fatigue syndrome (ME/CFS), or fibromyalgia often experience brain fog.
In fact, the term may have originally come from “fibro fog,” which sufferers of fibromyalgia have used to describe their frequent cognitive challenges. Chemotherapy patients may also be familiar with “chemo brain,” which refers to the fogginess caused by chemotherapy treatment.
Other medical conditions that sometimes feature cognitive dysfunction include:
- High blood pressure
- Depression
- Anemia
- Thyroid disorders
- Autoimmune diseases
- Diabetes
When Should You Be Worried About Brain Fog?
Your brain fog may be cause for concern when memory problems and other cognitive issues interfere with normal functioning. People with mild cognitive decline and/or early stages of dementia may find they have difficulty completing simple, everyday tasks like paying bills.
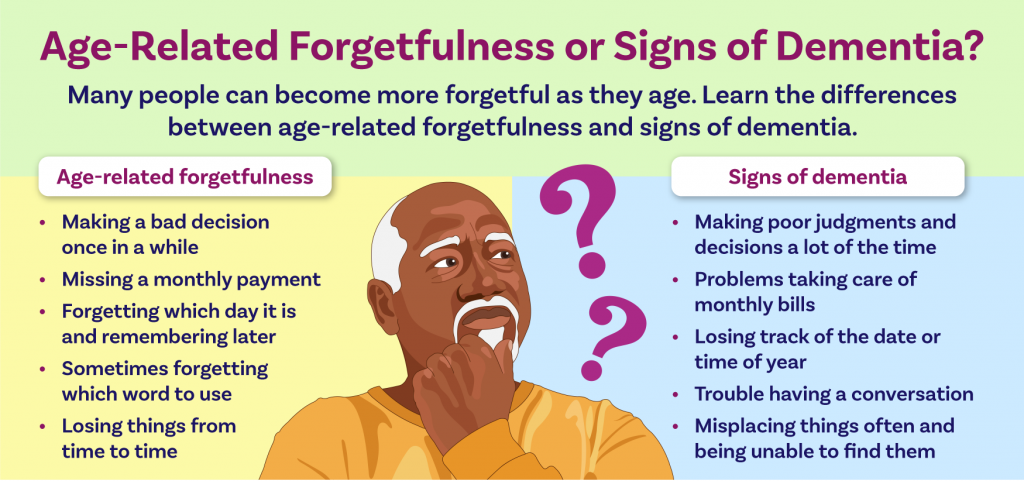
As we age, some amount of cognitive decline is natural, due to age-related changes in the brain.
This infographic from the National Institute on Aging details some common differences between normal aging and signs of serious memory loss.
Brain Fog and COVID-19
Experiencing brain fog long after recovering from COVID-19 is common. As Aviv Clinics’ physician Dr. Mohammed Elamir, MD, FACP, explains, there is a link between where the COVID-19 virus attacks the brain and how that impacted location affects long COVID symptoms.
If you’ve had COVID-19 and haven’t felt the same since, reach out to a trusted physician.
Your physician may ask about:
- Your current physical activity levels
- Medications or supplements you’re taking
- Possible nutritional deficiencies
- Possible infections and inflammatory diseases/conditions
- A timeline of symptoms
- How symptoms have changed over time
Your doctor may also request a blood test, Electroencephalogram (EEG), CT scan, or advanced MRI.
What Can You Do to Fight Brain Fog?
When your head feels heavy and foggy, this may be a sign that your body isn’t operating at peak performance, much like when you get sick with a cold or flu. The brain needs constant oxygen, the right supply of nutrients, and rest to function well.
When we fall short in one area of health, it’s easy to spiral out of control. Looking at the list of causes for brain fog, the cycle becomes clear: lack of sleep can lead to stress, which can lead to poor diet, and so on.
Often, the key to managing brain fog lies in good self-care. To ensure general health and wellness, try to:
- Manage stress—Many people find yoga and meditation helpful in dealing with stress. Counseling can also help you find customized coping mechanisms and an opportunity to chat about concerns with a trusted mental health professional.
- Eat a variety of healthy foods—Maintain a diet rich in vitamins and nutrients. Intermittent fasting, an eating regimen that alternates between eating and fasting, can help optimize brain function and sharpen the mind.
- Nutritional supplements—Specific nutrients may help combat brain fog. For example, vitamin D may help some of those suffering from symptoms linked to brain fog, such as fatigue and depression. Review your dietary intake with a medical professional or dietitian; consider filling in any nutritional gaps with supplements.
- Get enough sleep—What qualifies as a “good night’s rest” varies from person to person, so figure out what is right for you and stick to it. Sleep helps the body “cleanse your brain of toxins and waste,” helping you achieve a healthy brain.
- Maintain physical activity—Exercise has proven benefits for the brain. Start with 30 minutes per session, three days per week. Sticking with a physical activity you genuinely enjoy can help you stay committed to a routine.
- Drink enough water every day—Some cases of brain fog are due to simple dehydration. While fluid needs vary, the general rule of thumb is “15.5 cups” for men and “11.5 cups” for women daily.
- Challenge the brain with games, puzzles, or novel experiences—Just as our body needs to exercise to remain strong, our brains need exercise to perform at optimal levels. As we age, the brain loses neurons, often making brain fog more frequent. Cognitive training via brain games can improve memory and reasoning.
Diagnosis and Potential Therapies
If your circumstances merit additional assistance, there are medical interventions and therapies to pursue. What you select depends on the root cause of your brain fog. So we encourage you to take the time to speak with a physician to diagnose your situation and discuss options.
Diagnosis – Your physician may carry out one or a combination of the following clinical assessments to diagnose your case:
- Cognitive function tests
- Blood tests
- Neurological exams
Potential Therapies – Your physician may suggest therapies such as:
- Hormonal replacement therapy: Brain fog due to hormonal imbalances may require hormonal treatments. This treatment intends to balance your hormonal levels due to conditions such as menopause and helps improve brain fog symptoms.
- Cognitive behavioral therapy and counseling: Psychotherapeutic approaches such as cognitive behavioral therapy (CBT) help individuals cope with brain fog symptoms and gain a healthier perspective. CBT may also work on strengthening your cognitive function through brain exercises.
- Herbal supplements and nootropics for cognitive enhancement: Herbal supplements may be recommended for nutritional gaps. Nootropics such as L-theanine are known to provide a “boost of mental clarity and enhance your ability to focus.”
- Acupuncture and traditional Chinese medicine: For some, acupuncture and traditional Chinese medicine can alleviate brain fog and memory and concentration issues by increasing blood circulation.
- Pharmacological treatments for underlying medical conditions: If an underlying medical condition is causing your brain fog, your medical provider may prescribe medication to target the root cause. Over time, depending on how effective the medication is, you may experience improvement in brain fog symptoms.
- Hyperbaric Oxygen Therapy: In a randomized, controlled scientific study, a specialized hyperbaric oxygen therapy protocol was found to improve “global cognitive function, attention and executive function,” including brain fog, in patients suffering from long COVID.
The Aviv Medical Program Can Include the World’s Most Advanced Hyperbaric Oxygen Therapy (HBOT)
Identifying a long-term solution that looks after your health and happiness is essential. One long-term solution that has restored hope for many of our clients is a unique medical program offered exclusively at Aviv Clinics in central Florida.
Our effective treatment plan for cognitive dysfunction, including brain fog, may involve the world’s most advanced hyperbaric oxygen therapy (HBOT) in combination with cognitive, nutritional, and physiological therapies. This allows our clinical team to provide a customized approach uniquely tailored to your needs.
Aviv Clinics’ evidence-based treatment protocol helps enhance brain performance and reduce brain fog for many conditions like aging, traumatic brain injuries, fibromyalgia, post-stroke, long Covid, Lyme disease, and mild cognitive impairment.
Based on nearly two decades of research and development, the Aviv Medical Program is customized to your needs. Aviv Clinics in central Florida is the only center in the United States to offer this state-of-the-art program. Clients who choose our clinic can benefit from a personalized and comprehensive treatment approach.
Carl & Vickie Eckert
“Our quality of life was not what it should have been.”
Having parents who endured their fair share of cognitive issues, Carl and Vickie Eckert were alert to experiencing cognitive decline themselves. They were beginning to lose confidence in tackling their daily activities and knew it was time to make a change.
Fortunately, they discovered Aviv Clinics’ program, and today, they are happy to report that they are active, healthy, and enjoying all that Florida retirement has to offer.
Defy Limitations: Achieve Optimal Cognitive Health with Aviv Clinics
For more guidance on managing brain fog and cognitive health, contact Aviv Clinics. Our diverse medical team will happily provide the personalized care you need to get back on track.
Last update: July 1, 2025
What Is the Gut-Brain Connection? Exploring Gut Health and Brain Function
With much information available about “gut health” these days, it is difficult to know what’s real and what’s just hype. Data emerging from recent scientific research strongly suggests that gut health matters – much more than we previously thought, thanks to the gut-brain connection. The trillions of microbes that live in your gut may play a key role in keeping you healthy. Some scientists now treat the gut microbiome like an organ system, as important as our respiratory or circulatory systems.
Gut flora works in symbiosis with other organ systems, which means the gut could impact – and even prevent – numerous diseases and conditions. Autoimmune disorders, Alzheimer’s, heart disease, cancer, and even depression have all been associated with gut health.
For this reason, innovative centers such as Aviv Clinics are using customized nutrition plans as an integral part of treatment for clients seeking to improve their cognitive and physical performance, or symptoms of conditions like fibromyalgia, Lyme, dementia, and traumatic brain injuries.
Why Gut Health Matters for Brain Health: The Gut‑Brain Connection
As scientists continue to study our complex brains, we are learning that the brain’s functions extend far beyond the skull. The brain is deeply connected to the entire body, especially the gastrointestinal (GI) tract, or the “gut.” We can’t talk about brain health or brain function without including gut health and function. It’s exciting news for anyone struggling with neurological or psychological disorders. Could the secrets behind mysterious, complex, or debilitating conditions reveal themselves in the gut?
So what is going on in the gut, and how does it affect our health?
Understanding Your Microbiome: A Key to Better Gut Health
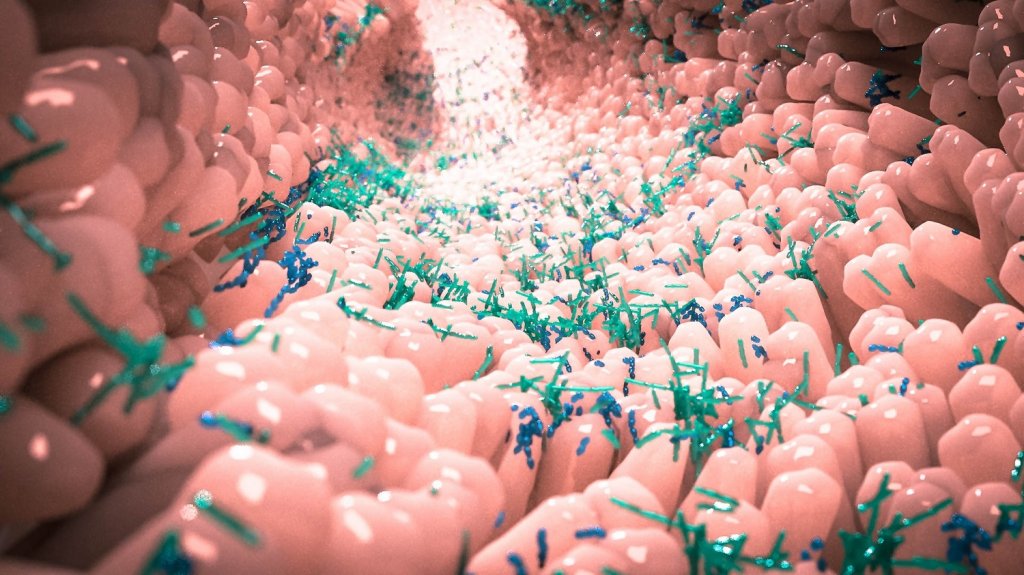
Your gut is home to over 100 trillion microbes, collectively called the microbiome or gut flora. With more than 1000 species of bacteria, viruses, fungi, and protozoa in your gut flora, they outnumber your human cells by 10 to 1.
Each microorganism in your body also contains DNA; added up, the microbiome contains roughly 200 times the amount of genetic material as in our own human cells. In fact, according to the University of Washington, “autoimmune diseases appear to be passed in families not by DNA inheritance, but by inheriting the family’s microbiome.”
The GI tract (via the mouth) is an entry point into the body, and the microbiome helps to keep out invaders by maintaining the intestinal barrier. This barrier acts as a filter to let in nutrients and keep out pathogens. The intestinal barrier also helps us digest our food, providing nutrients we’d otherwise be unable to harvest.
Gut Health Basics: Good vs. Bad Microbes Explained
The thought of trillions of bacteria hanging out in your body may seem a bit disarming. Generally, though, our guts are inhabited by commensal (good) bacteria and other microbes. Most microbes are harmless, so it’s important to understand that calling some microbes “good” and others “bad” is an oversimplification. Even the ones that may cause harm don’t always do so. A specific species of microbe might be completely harmless under most conditions, but potentially cause disease under different conditions. In the GI tract of an otherwise healthy person, the potentially harmful microbes reside in small numbers and are typically kept in check by other microbes.
What Makes a Healthy Gut?
Science can’t answer this definitively because everyone’s microbiome is unique. It’s not about one species of microbe or even a certain combination; what a healthy gut looks like varies from person to person.
“It would be great if we could identify 10 or so bacteria and say these are the ones you need most, but it doesn’t work that way, and there is no magic bullet,” says Dr. Elizabeth Hoffman, an infectious disease doctor from Massachusetts General Hospital.
What healthy guts have in common is diversity. They are colonized by a wide variety of microbial species. Assessing the health of the microbiome is about the balance and stability in the entire “ecosystem” of the gut. When this balance is thrown off, the microbiome can shift into a state of dysbiosis, where its normal supportive functions in the body get disrupted. As a result, the body becomes even more susceptible to disease and dysregulation.
What Causes Gut Dysbiosis?
Many factors have been found to cause gut dysbiosis: environmental factors like stress, diet, medications such as antibiotics, illness or disease, or even “inflamm-aging” can throw off the balance. Neurological and psychological conditions are being associated more and more with gut dysbiosis. By understanding the physical and functional links between the brain and the gut, we can see how their fates seem to be intertwined.
Your ‘Second Brain’: How Gut Health Influences Neurological Conditions
The sensation of butterflies in your stomach is one example of the gut-brain connection. If you’ve had digestive issues in stressful times, it’s not just a coincidence. Our thoughts and feelings can influence our health by directly altering the gut. Neurons, which we typically think of as only residing in the brain, also line our gastrointestinal tract and branch into our stomach and intestines. With over 500 million neurons, the enteric nervous system (ENS) is sometimes referred to as the “little brain” in our gut. This neural matter doesn’t contribute to thinking or consciousness, but it is part of a robust pathway for two-way communication between the big brain in your skull and your microbiome, known as the Gut-Brain Axis (GBA).
The Gut-Brain Axis is a complex two-way communication channel between the brain and the gut, involving the limbic system, central nervous system (CNS), autonomic nervous system (ANS, our fight or flight system), ENS, immune system, hormones, and more. Whatever is going on in your head, including emotions, behavior, and even thoughts, could partially be affected by what’s going on in your gut, and vice versa. As a result, if we want to understand neurological conditions, we can’t just study the brain. The gut microbiome has been linked to Alzheimer’s disease, Parkinson’s, depression, anxiety, and even “motivation and higher cognitive functions” all have been linked to the gut microbiome. The gut microbiome presents an area for more research that may be the key to treating these disabling conditions.
How Gut Health Drives Brain Chemistry Via the Gut‑Brain Axis
One of the gut’s primary roles is the production and turnover of neurotransmitters like serotonin, dopamine, and norepinephrine. The gut produces up to 95% of serotonin, sometimes called the “happiness hormone,” in our bodies. The gut also maintains the integrity of the intestinal mucosal barrier. This protective layer acts as a filter to keep out bad pathogens and toxins while letting in nutrients. If this barrier gets disrupted, invaders can infiltrate the body, promote inflammation, and exacerbate many autoimmune disorders. Gut flora also produces a metabolite called short-chain fatty acids (SCFA) that are integral in gut-brain signaling. When this signaling malfunctions, it can contribute to nervous system disorders, ranging from neurodevelopmental disorders to neurodegenerative diseases.
Brain‑to‑Gut Influence: Stress, Hormones & Gut Health Feedback
The microbes in our gut have receptors on their surface designed to interact with the neurotransmitters produced in the brain. Stress can directly affect your neurotransmitters, which can go on to influence the gut flora and its habitat. Stress can also change the total mass of the microbiota and the composition of species in the gut.
The GBA may control and respond to stress through our hypothalamic pituitary adrenal (HPA) axis, which involves hormones like cortisol. One theory of depression is that overactivation of the HPA axis often causes heightened levels of cortisol. The brain can also affect the gut by changing the habitat for the microbiome. This includes mucosal secretions in the intestines, altering how fast your bowels move, and other environmental conditions. It can also directly affect what enters your body from the outside and your immune function.

Tips for Better Gut Health to Support Your Gut‑Brain Connection
Here are a few tips:
Diet: It’s all about diversity. Eat a wide variety of foods for a healthier microbiome.
Stress: Keep your stress in check. When you’re stressed, your microbiome is stressed.
Antibiotics: While useful for fighting infections from harmful bacteria, antibiotics also often kill some of the good bacteria in your gut. Use of antibiotics may contribute to dysbiosis.
Prebiotics and Probiotics: Probiotics and prebiotics work together. Probiotics contain good bacteria that could correct gut dysbiosis. Probiotics may also improve depression and anxiety after just 30 days. Prebiotics are healthful carbohydrates and fiber from fruits and vegetables that help feed your probiotics. The more colorful your diet, the healthier your diet — and your gut — are likely to be.
The Bottom Line: Why Gut Health Is Vital for Brain & Whole‑Body Wellness
The discovery of the Gut-Brain Axis tells us that your thoughts, feelings, experiences, and environment all play into gut health, and can directly impact your overall health.
Aviv Clinics delivers a highly effective, science-based treatment protocol to enhance brain performance and improve the cognitive and physical symptoms of conditions such as traumatic brain injuries, fibromyalgia, Lyme disease, stroke, and mild cognitive impairment. The Aviv Medical Program is customized to each client’s needs and goals. The program can include nutritional support in addition to a unique hyperbaric oxygen therapy protocol. The personalized Aviv Medical Program and our HBOT protocol are based on nearly two decades of research and development.
Contact us to learn more.
Last update: June 25, 2025
Meditation and Brain Health: How Scientific Evidence Supports Its Benefits
The COVID-19 virus has left us all under more stress than ever, but there’s one group of people that the pandemic has hit especially hard: older adults. A recent poll conducted by the National Poll on Healthy Aging interviewed 2,000 adults aged 50 to 80. More than half (56%) of the participants reported struggling with feelings of isolation during the pandemic, a dramatic increase from 27% in the 2018 poll.
Long hours spent indoors away from family and friends can have us all feeling low, and stress and loneliness can wreak havoc on our mental health. That’s why many older adults are turning to the practice of mindfulness meditation to cope with stressful feelings during the pandemic.
Just like washing your hands to get rid of germs, meditation is an excellent way to help cleanse your mind of troublesome thoughts, and practicing mindfulness can do more than just help you relax. Taking a few minutes out of your day to ground yourself in the present moment is one of the most rewarding things you can do for your mental health, and the benefits are backed by science.
Supportive wellness practices, such as meditation, can be helpful to enhance cognitive and physical performance.

What is Meditation? Exploring Mindfulness Meditation and Brain Health
Mindfulness meditation is the art of being present in the here and now.
It’s about taking a few minutes every day to clear your mind of distressing thoughts and engaging with what’s right in front of you.
Think of it as a workout for your brain. In the same way that you might lift weights to keep your body strong, meditation is a way to train your mind and increase your focus and awareness. It’s not a spiritual practice or a mystical art; it’s a learned skill, and anyone can learn to meditate, regardless of age.
5 Benefits of Meditation for Brain Health — Backed by Science
There are several proven benefits to meditating regularly. Numerous studies have shown that mindfulness practices like meditation and yoga can improve numerous mental health concerns. From easing anxiety and depression to stalling memory loss in Alzheimer’s patients, here are our top 5 benefits of meditation.
1. Slowing Cognitive Decline Through Meditation
Although many people dismiss lapses in memory recall as a side effect of growing older, there’s no scientific evidence to suggest memory loss is a natural side effect of aging. On the contrary, forgetting valuable memories doesn’t have to be the new normal for older adults.
Meditation has been proven to improve memory recall in adults in as little as eight weeks. Research also shows promising results in the use of mindfulness to slow the progression of cognitive conditions like Alzheimer’s disease and dementia. Patients who practiced mindfulness exercises reported reductions in cognitive decline and stress levels, and overall improvements to their quality of life.
Mindfulness isn’t only beneficial for those diagnosed with cognitive conditions, either. Studies have also shown that caregivers of those with cognitive impairments can benefit from the stress reduction offered through practicing meditation. In other words, everyone can benefit from a boost to the cognitive centers of the brain.
2. Enhancing Focus and Mental Clarity With Meditation
Practicing mindfulness can keep your brain active and in good shape, no matter how strong your memory is. You don’t have to be a seasoned expert. Even beginners can reap the benefits of mindfulness meditation.
In one study, participants who listened to a 10-minute meditation tape experienced increased attention span and focus when completing a test compared to those who didn’t meditate beforehand. One researcher further confirmed that people who meditate regularly consistently perform better on focus-related tasks. The same study also found that meditation calms the areas of the brain associated with mind-wandering and spontaneous thoughts, helping you stay focused on what you are doing in the present.
3. Meditation Supports Better Sleep and Combats Insomnia
Getting a good night’s rest is more important than ever for seniors and older adults. Sleep is the vital period when our minds cleanse themselves of harmful waste. Yet current research estimates 10-30% of people are affected by chronic insomnia, with older adults showing more susceptibility to sleep disturbances.
A randomized trial found that mindfulness meditation significantly improved sleep quality in middle-aged and older adults. Because meditation can lower stress levels, it helps clear your mind from troubling thoughts, which can make sleep come more easily. If you have trouble sleeping at night, turn off your screens and try meditating for a few minutes before bed.
4. Reducing Anxiety Through Meditation
Although everyone worries from time to time, harboring too much stress in your body can be unhealthy. According to researchers, anywhere from 3-14% of all older adults meet the diagnostic criteria for generalized anxiety disorder. Unchecked anxiety and stress can worsen health conditions like fibromyalgia and lead to other mental health problems like depression.
If you want to take control of your anxious thoughts, meditation may be the solution. Studies have shown that mindfulness meditation can alleviate symptoms of generalized anxiety disorder and reduce stress levels, helping you clear your mind of fears and worries.
5. Uplifting Mood — Meditation’s Role in Mental Well-Being
Loneliness was already a common problem among older adults and retirees, but the COVID-19 pandemic has made it worse. Going out in public and visiting your family isn’t an option for many older adults, and the isolation can worsen feelings of loneliness and despair
Practicing mindfulness can help you manage these difficult emotions and improve your overall mood. Studies have shown that mindfulness training reduces feelings of loneliness and isolation, helping participants be happier in the present moment.
Mindfulness training has been shown to help reduce feelings of depression in adults. Those who practiced meditation therapy reported fewer symptoms of depression compared to their counterparts who didn’t meditate at all. Practicing mindfulness every day reminds you not to stress over every little thing, helping you stay calmer and more in control of your emotions.
How to Start Mindfulness and Meditation for Improved Brain Health
You don’t need any special equipment or training to get started. All you need is a comfortable place to sit and the willingness to give it a try. Here’s a quick guide to get you started:
- Find a quiet space where you can relax, free from distractions. If you’re inside, make sure that all televisions and electronic devices are turned off.
- Sit in a comfortable position and breathe gently.
- Pay attention to each inhale and exhale.
- Focus on all the sensations of your body as you breathe.
- Release any tensions you may be holding until you are completely relaxed.
- Continue to breathe in and out as you focus on your body’s inner sensations.
- If your mind wanders, that’s ok. Just re-focus on your breathing and start again.
- Keep going for 5-10 minutes or as long as you’d like to meditate.
Try to meditate at the same time every day to establish a routine. If you don’t want to sit in silence, you can find guided sessions via apps on your smart devices, or you can play some calming music to help you focus. For added benefits, try meditating outside on the porch or in a garden. Doing your daily session in nature can calm you even further, helping you make the most of your mindfulness practice.
The Bottom Line: Meditation Can Boost Brain Health and Well-Being
Mindfulness meditation is one of the most positive things you can do for your mental health and emotional well-being. It doesn’t take long to do, either. Having a simple routine to keep your mind in shape can offer benefits across all areas of your life. From improving memory recall to lowering stress levels and improving your sleep, practicing meditation can keep you more engaged in the present moment, helping you stay happy and calm during the best years of your life.
Cognitive health is one pillar of Aviv Clinics’ highly effective, science-backed medical program. The Aviv Medical Program is a customized, evidence-based intervention that can incorporate therapies like cognitive training and a specialized hyperbaric oxygen therapy protocol to achieve optimal results in both the brain and the body. Based on nearly two decades of research and development, the therapies in the Aviv Medical Program are customized to your specific needs and goals.
Curious if the Aviv Medical Program is the right choice for you? Contact Aviv Clinics today to schedule a complimentary consultation.
Last update: June 13, 2025


