A Post-Concussion Syndrome Test: Does One Exist and How is PCS Diagnosed?
A Post-Concussion Syndrome Test: Does One Exist and How is PCS Diagnosed?
If you have been relentlessly searching online for a post-concussion syndrome test or answers about possible PCS symptoms, you are not alone. It can be incredibly challenging when you don’t understand exactly what is going on in your brain and body. Even completing daily activities with post-concussion syndrome (PCS) symptoms can be especially taxing. Work, school, and relationships can all suffer when PCS is left untreated.
Does a post-concussion syndrome test exist? No, there is no single, definitive post-concussion syndrome that can diagnose PCS, a medical professional can still confirm the condition. Diagnosis is based on a history of head injuries and reported symptoms, as well as a thorough assessment of brain health and function.
Even without a simple PCS test, the Aviv Clinics medical team may be able to provide the clarity you’re seeking. In this article, we’ll explain the common signs of PCS, your treatment options, the type of care you should receive, and how the Aviv Medical Program can help you recover.
Post-Concussion Syndrome: A Condition That Requires a Diagnosis
Post-concussion syndrome is a condition where concussion symptoms continue beyond the normal recovery period.
Most people recover from a mild traumatic brain injury or concussion in a few weeks, with concussion symptoms easing gradually over a period of a few weeks. According to Aviv Clinics physician Dr. Mohammed Elamir, the more chronic symptoms of PCS entail “changes in cognition, whether physical and/or emotional, or sleep as a result of a concussion lasting more than three months.”
PCS occurs after you’ve endured a traumatic brain injury (TBI), even a very mild TBI, also known as a concussion. TBIs can be caused by accidents such as falls, vehicle crashes, and sporting injuries.
It is possible to have a traumatic brain injury and not know it. There are over 2.8 million people who sustain a TBI each year in the United States. When a TBI isn’t treated properly or the recovery isn’t complete, post-concussion syndrome can manifest.
Although there isn’t a quick test for PCS, there is ample research and understanding of this condition that can help explain its signs and symptoms. A clinical evaluation is warranted for symptoms that linger past the typical timeframe for recovery.
Common Signs of PCS That Lead to a Diagnosis
Luckily, there are specific signs to look out for to help you safeguard your health. PCS symptoms encompass four key areas:
- Physical
- Cognitive
- Psychological and emotional
- Sleep
No one enjoys life when dealing with dizziness, balance and vision issues, or challenges with memory or thinking. It’s frustrating to be more irritable than usual, or feel depressed or anxious after a concussion. An injury to your brain can easily impact your sleep, which prevents your brain from getting the rest it needs to reset at night.
How is Post-Concussion Syndrome Diagnosed When No Single Test Exists?
While there isn’t one specific test you can take for a PCS diagnosis, and you certainly can’t get a conclusive diagnosis from online information, there are a variety of assessments that physicians can use to determine if you’re dealing with chronic post-concussion symptoms.
Why use a variety of evaluations? By looking at different assessments, you can rule out any other cause for your troubling symptoms. In addition to reviewing your injury history and monitoring your symptoms, your doctor may perform a combination of any of the following exams to determine if you have PCS:
- Advanced neurological medical exam: This neurological exam entails evaluations of your nervous system. Physicians may use tools such as lights and reflex hammers.
- Neurocognitive testing: Neurocognitive testing examines brain function using memory, verbal communication, and motor tests.
- Advanced MRI with DTI sequence: This advanced version of an MRI maps out specific parts of the brain.
- SPECT scan: A SPECT (Single Photon Emission Computed Tomography) scan identifies parts of the brain that have been negatively affected.
What Happens After Post-Concussion Syndrome Testing?
Once you’ve been thoroughly evaluated, your physician will likely present a variety of treatment options for your post-concussion symptoms. Some facilities depend primarily on cognitive behavioral therapies, which have shown strong results for improving sleep for those suffering from PCS. Others may focus on vestibular therapies for improved balance, psychological interventions for symptoms like depression or anxiety, or neuro-optical therapy for blurred or double vision.
However, in most cases, these treatments only address the symptoms of post-concussion syndrome, and not the underlying cause: damage to delicate brain tissue.
Take time to learn more about your treatment options for post-concussion syndrome. This article walks through more research and treatment protocols you should learn about if you’ve experienced any type of brain trauma.
The Aviv Medical Program: A Treatment Option for Diagnosed PCS
If you’re looking for PCS relief, the Aviv Medical Program can be your answer. Our customized, multidisciplinary program is designed to address both the symptoms and the cause of your PCS by treating your damaged brain tissue. Our program is unique because it is managed by a diverse team of clinical experts, all under one roof, to provide the personalized care and attention you deserve:
- The Aviv Medical Program can include a combination of hyperbaric oxygen therapy (HBOT), cognitive exercises, physical training, and dietary coaching. In numerous clinical trials, a specific protocol of HBOT has been shown to improve the flow of both blood and oxygen to damaged brain tissue, encouraging recovery.
- Our patients have reported improved cognition (attention, memory, focus, balance, etc.) upon participating in our program. In fact, 96% of Aviv’s clients have experienced clinically verifiable improvements in cognitive function after completing the program.
- Our customized program is backed by over a decade of research in both adults and children. Explore more data from The Sagol Center for Hyperbaric Medicine and Research, one of the world’s largest and most advanced facilities of its kind.
Here’s What to Expect from the Aviv Medical Program for Post-Concussion Syndrome:
- Medical analysis: A thorough assessment conducted by Aviv’s clinical staff (physicians, neuropsychologists, physiotherapists, physiologists, and nurses). Depending on your symptoms and concerns, your pre-treatment evaluation can include advanced brain imaging, cellular analysis, neurocognitive testing, and more.
- Personalized treatment plan: Based on the results of your assessment, our team develops a treatment plan specifically for you. Your customized Aviv Medical Program may include HBOT, cognitive and physical training, and dietary coaching to build the best possible foundation for recovery.
- Post-treatment assessment: At your request, after completion of the program, we can repeat the initial tests to measure progress and make recommendations for ongoing progress.
Learn More About the Aviv Medical Program for PCS
If you believe you or your loved one has post-concussion syndrome, don’t wait for an easy PCS test. The sooner you begin treatment, the better your potential for lasting improvement.
At Aviv Clinics, our team of certified medical professionals has helped thousands of people regain clarity, energy, and quality of life, even after years of lingering symptoms.
Take the first step towards recovery today by contacting our clinic. Our team of certified medical professionals has helped a variety of individuals with unique health backgrounds get back to optimal health. Schedule a consultation and let’s create a personalized path to help you function at your best again.
Last Update: August 14, 2025
Effective Treatments and Support for Pediatric Traumatic Brain Injuries
Traumatic brain injury (TBI) in children and teens is a sudden disruption to brain function caused by a blow or jolt to the head. When a young person experiences a TBI or concussion, it can affect physical abilities, cognitive function, and emotional well-being. This impact can disrupt or restrict blood flow to certain regions of the brain, affecting its ability to function properly. Pediatric brain injury treatment focuses on helping teens recover fully and regain their quality of life. At Aviv Clinics, our specialized program offers a comprehensive, personalized approach to treating pediatric TBIs.
Pediatric Traumatic Brain Injury in Teens: Risks and Statistics
When it comes to TBIs and concussions, adolescents are a high-risk group. 2020 CDC data reveals that 12.2% of U.S. children aged 12 to 17 reported experiencing concussion or brain injury symptoms at some point in their lives.
Common Causes of Pediatric TBI and Concussions
The most common causes of TBI and concussions in teens include:
- Falls
- Sports like football, basketball, soccer, lacrosse, ice hockey, wrestling, and cheerleading
- Motor vehicle accidents
- Bicycle accidents
- Physical abuse
How Pediatric Traumatic Brain Injury Affects Teens
Teens suffering from TBIs or concussions can experience moderate to severe symptoms that may involve physical, cognitive, and behavioral or emotional issues. New treatment approaches offer a pathway to improvement in teens suffering brain injuries to get them back to feeling like themselves.
The Aviv Medical Program offers pediatric traumatic brain injury rehabilitation using a personalized a multidisciplinary approach. Backed by nearly two decades of research, Aviv Clinics’ unique medical program combines interventions like cognitive and physical training, dietary coaching, and hyperbaric oxygen therapy (HBOT).
Real Life Success Story: Pediatric Traumatic Brain Injury Treatment at Aviv Clinics
The Aviv Medical Program took one teen from concussion to competition.
Linden Perry was a 15-year-old honors student and star athlete when she experienced what seemed like a minor head bump against the goalpost during soccer practice. Not long afterward, she fell and hit her head during a basketball scrimmage — but this time, the result was anything but minor..
Troubling symptoms — including sensitivity to light and sound, loss of balance, double vision, and eye seizures — appeared immediately. The symptoms continued for weeks after the injury, and Linden was eventually diagnosed with post-concussion syndrome (PCS). She had trouble concentrating in school. She was missing classes and assignments. Her grades began slipping, and she could no longer play sports.
Doctor after doctor told Linden there was nothing they could do, and that she needed to accept her new reality.
The Aviv Medical Program: Innovative Brain Injury Treatment
Linden’s mother Carissa learned about Aviv Clinics, and turned to the Aviv Medical Program as their final attempt to get Linden back.
The PCS treatment plan for Linden included sessions of a unique hyperbaric oxygen therapy (HBOT) protocol. While inside the roomy hyperbaric suite, she completed brain exercises that focused on working memory, reaction time, attention, and information processing speed.
Linden’s recovery program lasted three months. During that time, she also worked with Aviv’s nutritional coach, physical therapists, physiologists, and neuropsychologists. This comprehensive, team-oriented approach ensured Linden achieved optimal cognitive and physical performance.
A final assessment of Linden at the end of the program revealed improvement in cognitive ability, strength, agility, balance, confidence, and energy. Undergoing the innovative treatment at Aviv Clinics helped Linden overcome post-concussion syndrome and feel like her old self again. Not only was she able to return to the field, but she also won a state championship with her high school team and is now playing collegiate soccer.
What Parents Should Know about Pediatric Traumatic Brain Injuries
After a TBI incident or concussion, your teen may feel confused or scared. Provide support by offering reassurance and taking them to a physician right away, even if your child didn’t lose consciousness. Receiving a diagnosis quickly can help your loved one avoid further risks to their health and the healing process.
Your child should also pause any sports activities they are involved in.
During the treatment journey, keep these four tips in mind to ensure your teen receives the comprehensive care they need and deserve.
1. Pediatric TBI and Concussion Symptoms Vary in Severity
While symptoms of TBI in children vary in scope and severity, they can all adversely impact a teen’s life.
Parents should be on the lookout for physical, cognitive, behavioral/emotional symptoms, and sleep issues if they suspect their teen might have a TBI.
Physical symptoms of a TBI include:
- Headaches
- Visual problems
- Dizziness
- Loss of balance
- Hearing difficulty
- Ringing in the ears
- Sensitivity to light and/or noise
- Nausea and/or vomiting
- Seizures
- Chronic pain
Cognitive TBI symptoms include:
- Attention and memory problems
- Poor concentration
- Delayed processing speed
- Difficulty finding words
- Impaired judgment
- Confusion
- Perseveration (the continual involuntary repetition of a thought or behavior)
Behavioral/emotional symptoms of a TBI include:
- Anxiety
- Depression
- Irritability
- Impulsivity
- Aggression
- Decline in social skills
TBI-related sleep issues include:
- Difficulty falling or staying asleep
- Sleeping too much (hypersomnia)
- Fatigue and/or loss of energy
2. Pediatric TBIs and Concussions Often Go Undiagnosed
A study found that one in four children with mild traumatic brain injury (mTBI) still suffered from post-concussive symptoms years after an injury. The study concluded that in the vast majority of children suffering from persistent symptoms, the initial concussion diagnosis is missed.
Researchers also concluded that better screening guidelines and practices should be employed after suffering mTBI. They added, “Once diagnosed, patients can be referred to appropriate medical, academic, and emotional consultations and interventions.”
3. Clinical Research Shows HBOT Can Be Effective in Treating Pediatric Traumatic Brain Injury
A significant body of research over the last decade demonstrates the effectiveness of HBOT in improving TBI-related symptoms.
Studies indicate that traumatic brain injury responds well to hyperbaric oxygen therapy when delivered using a unique HBOT protocol. In clinical trials, this specific HBOT protocol improved neurological conditions in patients with mild TBIs, even many years after the initial injury.
- One study that examined the role of hyperbaric oxygen therapy in severe pediatric head injury found that study participants who received HBOT performed significantly better than control group participants who did not receive HBOT. Improvements were seen “on all the parameters with decreased hospital stay, better [Glasgow Coma Scale] GCS, and drastic reduction in disability.”
Researchers concluded that “in children with traumatic brain injury, the addition of HBOT significantly improved outcome and quality of life and reduced the risk of complications.”
- Another study tested the effectiveness of HBOT in improving brain function and quality of life in 56 patients suffering from post-concussion syndrome one to five years after injury. Patients were randomly assigned to either treatment or a control/crossover group. Patients in the treated group received 40 HBOT sessions; patients in the crossover group received no HBOT for a two-month control period.
Researchers found that the HBOT group significantly improved in all cognitive measures, including information processing speed, attention, memory, and executive functions.
The study’s authors concluded that “HBOT can induce neuroplasticity and significant brain function improvements in mild TBI patients with prolonged post-concussion syndrome at the late chronic stage, years after brain injury.”
4. How Aviv Clinics Provides Pediatric TBI Treatment
Backed by science, Aviv Clinics’ innovative TBI treatment protocol integrates the same specialized HBOT protocol into a personalized program. Based on each client’s medical condition, goals, and pre-treatment assessment, this regimen can include cognitive training, physiotherapy, and nutrition coaching. Our board-certified clinical team works together, under one roof, to put TBI and PCS patients on the road to recovery and healing.
The HBOT component of the treatment involves breathing 100% pure oxygen in a special room known as a hyperbaric suite. In the suite, patients experience Aviv’s unique HBOT protocol, which combines two processes:
- Increasing the oxygen level in the tissues of the body and brain
- Fluctuating the level of oxygen to stimulate the body’s natural processes of repair and recovery
Benefits of the Aviv Medical Program for Pediatric TBI Include:
- Improved cognitive performance:
- Attention
- Memory
- Focus
- Clarity
- Information processing
- Psychological symptoms
- Improved motor functioning:
- Coordination
- Balance
- Gait
These benefits can be gained even years after the TBI.
If your teen is struggling with the effects of a pediatric traumatic brain injury or suspected post-concussion syndrome, you don’t have to face the journey alone. Aviv Clinics offers an advanced, research-backed treatment program designed to support recovery and help children regain their cognitive, physical, and emotional strength. Every child’s brain is unique, and so is our personalized approach.
Contact us today to learn how our team can create a personalized treatment plan to help your teen thrive after a brain injury.
Last Update: August 10, 2025
TBI and Mental Health: Understanding the Link and Your Recovery Options
Concussions and traumatic brain injuries (TBIs) are well known for causing physical and cognitive impairments, but their impact on mental health is often overlooked. The connection between TBI and mental health can be profound, affecting mood, behavior, and overall quality of life long after the initial injury.
Each year in the U.S., an estimated 2.8 million people sustain a TBI from falls, motor vehicle accidents, contact sports, and other incidents. Dubbed a “silent epidemic,” people of all ages are at risk for TBIs. Brain injuries can disrupt the brain’s ability to regulate emotions, leading to issues like anxiety, depression, mood swings, and other challenges. Even mild TBIs (what we consider a concussion) can trigger lasting emotional and psychological symptoms left untreated.
Fortunately, innovative and holistic therapeutic medical programs that use hyperbaric oxygen therapy (HBOT) show promise in alleviating behavioral and emotional symptoms. A large body of research shows the effectiveness of HBOT in improving brain function and quality of life in mild traumatic brain injury (mTBI), or concussion, patients suffering from chronic neurocognitive impairments.
How TBI and Mental Health are Connected
According to the CDC, mental health is essential to overall health and includes our emotional, psychological, and social well-being.
The CDC says that mental health:
- Affects how people think, feel, and act.
- Helps determine how people handle stress, relate to others, and make healthy choices.
- Influences our susceptibility to chronic conditions
- Is “important at every stage of life, from childhood and adolescence through adulthood.”
A TBI or concussion can impact areas of the brain that regulate behavior and emotion (i.e., the frontal lobes). People suffering from a TBI can experience behavioral and emotional challenges.
If these TBI mental health issues are not addressed promptly, they may exacerbate over time. For example, someone having trouble remembering or following conversations may become frustrated and depressed. When a TBI or post-concussion syndrome strips away these small capabilities we take for granted, it can take a toll on our mental health.
Behavioral and emotional symptoms that can emerge after a TBI include:
- Anxiety
- Depression
- Mood swings
- Irritability
- Post-traumatic stress disorder (PTSD)
- Brain fog
- Apathy
Research on TBI and Mental Health Challenges
Research points to a connection between brain injury and mental health disorders:
- A National Institutes of Health (NIH)-funded study published in JAMA Psychiatry revealed just how common mental health disorders are following a mild head injury. Approximately one in five individuals may experience mental health symptoms up to six months after a mild TBI.
- Children are also susceptible to TBI-related mental health challenges. One study found that young people with pediatric acquired brain injury (pABI) are twice as likely to develop a mood disorder as their peers and, as adults, are twice as likely to use adult mental health services.
- Another study found that people who have sustained an mTBI are three times more likely to experience depression than those without a history of mTBI. Researchers noted that this risk remains decades after the concussion (mTBI).
TBI Recovery at Aviv Clinics?
You’ll find the world’s most innovative treatment program for improving the cognitive, physical, emotional, and behavioral symptoms of TBI at Aviv Clinics.
At Aviv, concussion and TBI survivors will benefit from:
- A personalized medical treatment program
- A team approach to care
- Innovative treatment protocols backed by science
- Cutting-edge technology
Personalized Treatment for TBI and Mental Health Symptoms
Aviv Clinics takes a unique, holistic mind/body approach to post-concussion syndrome and TBI rehabilitation with a multidisciplinary medical care program. Our program entails three parts:
- Assessment: When clients come to Aviv, we can conduct an in-depth evaluation of their physical, neurological, and cognitive condition to ensure they qualify for the Aviv Medical Program. This may include cognitive assessments, high-definition brain imaging, physical evaluations, and more.
- Treatment: For those who are a fit, the next step is for our team of licensed clinicians to prepare a personalized treatment plan. The program can incorporate various therapies, including a robust HBOT treatment schedule combined with personal cognitive training, physiotherapy, and nutritional coaching.
- Analysis: At your request, once the program is complete, we can perform a comprehensive post-treatment evaluation. This enables us to measure improvements empirically and make recommendations for ongoing progress.
Collaborative Care for TBI and Mental Health Recovery
Our team of physicians, clinical program managers, physiotherapists, nurses, clinical psychologists, and nutrition specialists collaborates to provide the care patients need for the best health outcomes.
This coordinated patient-centered approach helps ensure the quality, safety, and reliability of care. Perhaps most important, 96% of our clients experience clinically verifiable improvements in brain function after the Aviv Medical Program.
Science-Backed Therapies for TBI and Mental Health
The innovative Aviv Medical Program is based on dozens of high-quality clinical studies over nearly two decades of research.
These studies provide documented evidence of the effective use of hyperbaric oxygen therapy to help people suffering from traumatic brain injuries, regardless of the severity of their condition.
Research suggests the Aviv HBOT protocol:
- Improves neuroplasticity, the brain’s ability to adapt in response to an injury or disease
- Activates neurogenesis, the regeneration of nerve cells in the brain
- Initiates angiogenesis, the growth of new blood vessels in the brain and body
- Promotes improvements in mental health, such as decreased depression
The carefully regulated oxygen and pressure levels in HBOT help to oxygenate damaged tissue. This treatment ultimately encourages those tissues to regenerate and heal faster, improving chronic impairments in patients with post-concussion syndrome and TBIs. This can be effective even with brain injuries that are many years old.
A series of additional clinical trials demonstrates the efficacy of HBOT as a therapeutic intervention for many conditions, including stroke, fibromyalgia, long COVID symptoms, and a host of other conditions.
Aviv Clinics replicate the same HBOT protocols used in these clinical trials and administer them under the same strict conditions.
This evidence-based treatment protocol is unique to Aviv Clinics and is performed at our medical facility by trained physicians. They’re not the same treatments delivered at oxygen spas and pods.
Advanced Technology to Support TBI and Mental Health Healing
At Aviv Clinics, patients have access to cutting-edge technology designed to help improve the cognitive, physical, and emotional/behavioral symptoms of TBI and concussion. Aviv’s spacious HBOT suite is the most technologically advanced and comfortable chamber available. These suites feel more like a first-class airplane cabin than a treatment chamber at a medical facility. It provides an exceptional, safe experience for patients as they participate in every HBOT session with a qualified member of our medical team.

Begin Your TBI Treatment Journey With Aviv Clinics
Understanding how TBI affects mental health is a critical first step toward effective treatment. Patients don’t have to continue suffering from the “invisible illness” that is TBI. If you or a loved one is experiencing cognitive, physical, or behavioral symptoms after a TBI, contact us today to find out how we can help.
Last update: August 10, 2025
Asking “What Can HBOT Treat?” Is Like Asking Why Oxygen Matters
Every time you take a breath, your body receives vital oxygen, which helps it to grow, function, and convert the food you eat into energy. Oxygen is also vital in cellular function and brain activity.
But inhalation isn’t always enough to supply the body with the oxygen needed for optimal functionality and healing. Learn more about how to regulate and elevate the oxygen in your body, as well as how treatment options can resolve ongoing health conditions and symptoms.
What Is HBOT?
Hyperbaric oxygen therapy (HBOT) is a process that elevates the amount of oxygen in the body.
Patients breathe in 100% oxygen in a pressurized environment, which can help:
- Increase the amount of oxygen in the blood
- Regenerate damaged tissue to heal faster
In other words, HBOT can help patients live healthier and happier lives.
Why People Seek Out HBOT
Patrick Bol experienced lingering symptoms of COVID that extended well beyond the expected recovery period. Watch Patrick’s journey below!
While Patrick turned to Aviv for relief of his long COVID symptoms, the Aviv Medical Program, which can include HBOT, offers a clinically-tested treatment option for a number of conditions.
14-year-old Linden Perry suffered post-concussion syndrome after multiple concussions sustained while playing basketball and soccer.
74-year-old Trice Hirr couldn’t get back to her competitive swimming speed because of a history of injuries and a hip replacement.
Lyndi Scott-Strite suffered from symptoms of Lyme disease, which made her step back from her usual activities and routine.
The stress from her husband’s illness put pressure on Zizi McKinnon’s mental and physical health.
This common thread that binds these individuals is not just about health—it’s about taking control of their minds and bodies to help them live life the way they want. No one deserves to live an average life, plagued with discomfort or health problems.
Living a full and active life comes down to finding the right team of medical professionals, and you’ve come to the right place. Aviv Clinics is here to support you in your journey back to optimal health.
The Aviv Medical Program treatment can include hyperbaric oxygen therapy. We are proud to offer HBOT as a part of our program to help patients finally experience relief from a range of conditions, so they can start living their life to the fullest again. This could be you.
Why Does Hyperbaric Oxygen Therapy Matter?
HBOT revitalizes your body by increasing the oxygen concentration in the body. For wound healing, it delivers oxygen-rich plasma to areas that have been slow to heal.
Whether you’re experiencing a decline in sports performance or lingering symptoms from an illness or injury that occurred months or even years ago, your physician may determine HBOT to be a beneficial component of your treatment plan.
“With a chronic illness, it can feel like you’re done living…I feel like I am myself again.” Lyndi Scott-Strite, former Aviv patient
“[The Aviv Medical Program] was more for a survival perspective. I wanted to keep my job. I wanted to keep on living. I wanted to keep being an outdoors person and be there for my family.” Patrick Bol, former Aviv patient
HBOT: A Research-Backed Therapy Program
Oxygen and HBOT are at the forefront of innovative medical research. And for good reason—every tissue and cell in our bodies need a constant supply of oxygen to work properly.
Oxygen also serves the following functions in the human body:
- Promotes blood circulation
- Reduces inflammation
- Encourages collagen formation
- Help blood vessels grow
HBOT has been used since the 1800s, which demonstrates its longevity and effectiveness over the years. Aviv uses advanced and unique HBOT technology to deliver safe and secure medical treatments. Decades of research illustrate that HBOT may help people suffering from a variety of health conditions, including:
- Stroke
- Post-Concussion syndrome
- Lyme disease
- Long COVID
- Concussion and TBI (traumatic brain injury)
- PTSD (Post-traumatic stress disorder)
- MCI (mild cognitive impairment)
How Does HBOT Work?
Here’s what to expect during your HBOT journey as a part of the Aviv Medical Program:
1. You’ll enter a hyperbaric oxygen chamber. This spacious HBOT chamber feels similar to the business class section on an airplane. You’ll sit comfortably and breathe through a custom-fitted oxygen mask. Patients generally don’t feel anything during this process. Most play brain exercise games on a tablet during their HBOT sessions. Others listen to podcasts or learn a new language.

2. You’ll rotate between breathing through the mask and breathing air. During the HBOT treatment, you will alternate between breathing 100% pure oxygen and medical-grade air. Our medical staff will help you prepare for HBOT before your first session.

3. You’ll come back for repeated HBOT sessions. Most of our patients complete roughly 60 sessions altogether, but your Aviv Clinics physician will determine the treatment plan that’s right for you. Medical staff will be in the oxygen chamber with you at all times to ensure your comfort and that the process goes smoothly. At the end of your treatment, you’ll receive detailed before-and-after reports that outline your progress.

Aviv’s Holistic Approach
A holistic approach to recovery can include HBOT coupled with additional therapies for a more comprehensive treatment. Your holistic plan may include:
- HBOT
- Cognitive training
- Physical training
- Nutritional coaching
Our holistic medical protocol delivers incredible results, which are often greater than what research studies illustrate. Each body ages and functions differently, so it’s imperative that your plan is uniquely your own.
“At your beck and call, you have a physician, dietitian, physical therapist… so many professional people who will help you. What came out was a plan for me—just for me.” ZiZi McKinnon, former Aviv patient
“You get to work with everybody from the neurologist who works with you on brain games to the dietitian who helps you with your diet. For Lyme disease, that’s extremely important.” Lyndi Scott-Strite, former Aviv patient
If you believe that you or a loved one would benefit from hyperbaric oxygen therapy in Florida as part of the Aviv Medical Program, contact our team of certified medical professionals today. Contact Us!
How Long Does HBOT Take to See Results?
Most people see improvement from the Aviv Medical Program very early in the 8-12 weeks of therapy and see medically verifiable results at the end of their treatment. This time frame allows the body to begin maximizing its ability to regenerate cells and blood vessels.
Keep in mind, there is no one-size-fits-all approach. You’ll receive your own unique, holistic therapy plan that can include HBOT, so outcomes and timelines will vary.
We’ve had patients who were amazed at how much more weight they can lift at the gym, how they can think through and remember things more clearly, and how energetic they feel each day.
Aviv Clinics provides objective data during your treatment plan to assess your oxygen levels and brain output before and after implementing HBOT coupled with other therapies. Our ability to quantify your health plan is ultimately what can give you hope.
How Long Do the Effects of Hyperbaric Oxygen Therapy Last?
We strive for long-lasting effects of the Aviv Medical Program for every patient. Our relationship with you does not stop at the end of your plan timeline. We’ll send you off with a wearable device and continue to check in with you and send reports on your health and performance.
“I’m five months after the program, and I really do feel a lot calmer. I’ve been able to think through things more clearly. Before I was losing confidence, I was in a panic… now I plan to tap dance until I’m 120 years old!” ZiZi McKinnon, former Aviv patient
HBOT for Various Conditions
HBOT can bring hope to those dealing with various unique medical challenges. Here are some conditions Aviv can help you fight.
Aging
Researchers discovered HBOT may improve signs of aging by:
- Improving cognitive function, specifically attention span, information processing, multitasking, and memory,
- Lowering the number of cells responsible for aging,
- Increasing telomere length.
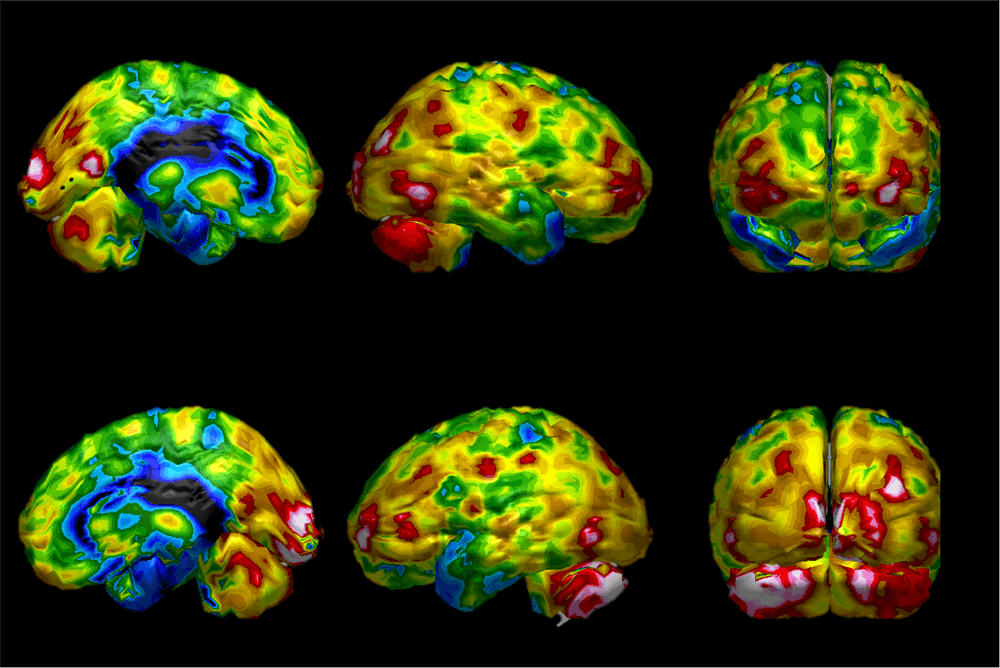
SPECT brain scan images of anti-aging before and after HBOT trials suggest positive effects of HBOT on aging.
Post-Stroke
One research study suggests HBOT can significantly improve post-stroke conditions. Study participants described an improved quality of life. When combined with proper nutrition, exercise, and regular assessments, HBOT may help post-stroke patients regain their speech, motor functions, and independence in performing day-to-day tasks.
Mild Cognitive Decline
HBOT’s ability to increase blood flow to the brain shows promise in improving memory function. The number of brain vessels naturally declines with age, and HBOT can help lessen this effect. One study suggests that HBOT can help combat memory loss and reverse early biomarkers of Alzheimer’s disease.
Traumatic Brain Injury (TBI) and Post-Concussion Syndrome (PCS)
Approximately 30-40% of those who suffer concussions or traumatic brain injuries experience lingering symptoms. This condition is called post-concussion syndrome (PCS) or persistent post-concussive syndrome (PPCS) and merits careful medical attention.
While the brain is an impressive organ with millions of capabilities, sometimes it needs intervention and treatment to fully heal and function at its best. Studies indicate HBOT may improve PCS, even years after a mild traumatic brain injury event.
“I’ve noticed that my balance, which was really thrown off when I first got [to Aviv], is coming back now.” Linden Perry, PCS survivor and Aviv Clinics patient
Lyme Disease
Chronic Lyme disease is one of the most challenging illnesses to recover from. Patients often receive little relief from antibiotic-heavy therapies. Luckily, recent research suggests that HBOT may improve symptoms of Lyme disease in patients who have taken antibiotics for at least 10 years.
“I now have a solution. I have a way to get back to this place where I’m feeling energized, I’m feeling vital, I’m feeling like I can take on the world again.” Lyndi Scott-Strite, Lyme disease survivor and Aviv Clinics patient
Fibromyalgia
In one research study, fibromyalgia patients who underwent HBOT sessions five days per week over 12 weeks experienced less chronic pain. Further research needs to be conducted, but these early studies suggest that HBOT may help fibromyalgia patients live a more comfortable life.
Start Your Healing Journey with Aviv
If you’re looking for answers and solutions to your challenging medical conditions, reach out to the Aviv staff. You’ll speak directly to a member of our comprehensive team of certified medical specialists. During your first call, we’ll discuss your medical background to determine if the Aviv Medical Program may be right for you.
As Dr. Mohammed Elamir, MD, FACP, puts it: “The Aviv Medical Program can be successful because it addresses the cause of the symptoms, not just the symptoms alone. In combination with cognitive, physical, and nutritional coaching, some HBOT protocols can be very effective.”
Contact our HBOT Florida medical professionals to talk about how you can incorporate hyperbaric oxygen therapy benefits into your healing and relief journey.
Silent Stroke Symptoms: What They Are & Why You Shouldn’t Ignore Them
You’re probably familiar with common stroke symptoms like difficulty speaking, seeing, walking, and numbness on one side of the body. These are all obvious signs, enabling you to quickly get the help you need. However, it’s possible to have a stroke and not even know it or remember it happening. Silent cerebral infarction (SCI) is a “silent stroke” that causes brain damage and often leads to a more severe stroke down the road, possibly within the next year.
- Silent strokes are much more common than other recognizable types of strokes. Experts estimate:
- Silent strokes affect 8 million to 11 million Americans each year.
- “For every person who has a stroke with symptoms, about 14 others have a silent stroke.”
Understanding the symptoms of a silent stroke is critical to safeguarding your health. Over time, the damage from these strokes can accumulate, leading to more serious issues.
None of us want to live under such uncertainty. Aviv Clinics is here to help you take full ownership of your health. Learn the facts about silent stroke and how to recognize the 10 key symptoms.
What Is a Silent Stroke, and How Does It Differ from Other Strokes?
Like other types of strokes, a silent stroke occurs when an obstruction cuts off the blood supply to part of your brain.
The difference between silent strokes versus other strokes is this: The part of your brain affected by a silent stroke is too small to block your vital brain functions. Your symptoms may go unnoticed or be blamed on other health or mental conditions.
Most people don’t know if they’ve experienced a silent stroke. They would only know through an MRI or CT scan, which shows affected small blood vessels, changes in white matter, or lesions.
What Are the 10 Symptoms of a Silent Stroke?
There are 10 signs of a silent stroke you or a loved one may experience. Depending on the sign, these may last a couple of hours, a few days, or even persist long-term.
However, he symptoms of silent stroke may mimic signs of other medical conditions, making them complex to recognize. Be sure to speak with your doctor about any concerns you may have. Following are symptoms you should be aware of:
- A lapse in (or loss of) short-term memory: Do you have to ask someone to repeat instructions they just told you, but still remember details from a conversation you had last month? Is there a day or activity you had recently that you simply don’t remember, even with prompts?
- A decreased ability to think or reason: Have you given up on a game you used to love playing, like Sudoku or crossword puzzles? Do you find yourself frustrated or arguing more because you don’t understand someone else’s reasons for wanting you to do something?
- Mood changes: Are you suddenly irritable, anxious, apathetic, or depressed? Have you found yourself crying or laughing for no apparent reason or at inappropriate times?
- Psychiatric disorders: Do you have hallucinations or delusions? Have you engaged in inappropriate motor behavior, like repeatedly banging your head?
- Trouble with balance: Are you experiencing dizziness or feeling like your head is spinning? Is it difficult to make quick adjustments to maintain balance? Do you find yourself stumbling or bumping into things? Does it feel like you’re standing upright when in fact, you’re leaning to one side?
- Movement or walking impairment: Are your toes now catching on the ground when you take steps? Do you tire quickly just from walking to your neighbor’s house? Is walking and talking at the same time difficult for you?
- Limb clumsiness: Does it take concentration to control your hand motions? Is it tricky to type even though you’re normally very proficient? Do you have a shaky leg? Are you noticing a decrease in hand-eye coordination?
- Incontinence: Do you feel the urge to urinate more often than usual? Are you consciously or unconsciously leaking urine or stool during the day or while asleep at night? Is it difficult to empty your bladder completely?
- Headaches or migraines: Are you having more headaches or migraines than usual? Or are you getting long-term, persistent headaches? Have your headaches become severe enough to disrupt your daily activities?
- Vision issues: Does seeing clearly take concentration? Are you less aware of your surroundings? Do you have double vision? Has your field of vision become smaller?
It’s important to note that these symptoms of silent stroke may also be signs of other medical conditions, so it’s important to speak with your doctor about your concerns and treatment options.
Why Silent Stroke Symptoms Can Be So Dangerous
- Just because you don’t feel a silent stroke doesn’t mean it’s not harmful. A silent stroke kills brain cells and tissues. A study published by the American Heart Association (AHA) journal calls signs of a silent stroke the “most common incidental finding on brain scans.”
- It’s common to suffer several silent strokes before noticing a cumulative neurological effect, even vascular (post-stroke) dementia. In fact, “almost a quarter of people who have had a stroke will go on to develop dementia after about three to six months.”
Can You Treat a Silent Stroke?
Please know there is still hope after a silent stroke.
Peer-reviewed, published scientific studies show a unique hyperbaric oxygen therapy (HBOT) protocol can help improve neurocognitive functions of post-stroke patients.
Hyperbaric oxygen therapy involves breathing 100% pure oxygen in a pressurized chamber. The unique protocol in these studies fluctuates oxygen levels, unlocking the body’s self-healing abilities through a phenomenon known as the hyperoxic-hypoxic paradox.
The Aviv Medical Program for Stroke Recovery
The Aviv Medical Program was founded on this research and unique protocol. The post-stroke program at Aviv Clinics has helped stroke survivors regain some of their capabilities, in many cases several years after their incident.
In addition, our team can conduct high-resolution scans as part of an in-depth assessment of stroke and its resulting damage to the brain. Clinicians can use this information as a map for each client’s customized program and to track recovery in post-treatment assessments.
Learn about our post-stroke program>>
Depending on your symptoms, needs, and goals, your post-stroke program can include the following:
- In-depth review of medical history
- Comprehensive physical and neurological exams
- Physical therapy evaluation
- Highly advanced brain imaging scans
- Neurocognitive tests
Once results are received, our medical team collaborates to build a personalized program for each client. The customized treatment plan can include a combination of the following:
- Hyperbaric oxygen therapy
- Cognitive training
- Physical training and/or physical therapy
- Dietary coaching
Stay educated on post-stroke treatments – sign up to watch our webinar >>
Don’t Suffer in Silence: Schedule a Consultation
Don’t suffer in silence. If you or a family member are showing signs of a silent stroke, Aviv Clinics is here to help.
Schedule a complimentary consultation with an Aviv Clinics doctor or take a tour of our specialty clinic and get your advanced brain imaging scans to check for symptoms of a silent stroke.
Last Update: August 8, 2025
Is it Age-Related Cognitive Decline? A Guide to Symptoms, Causes and Treatment
Cognitive health — the ability to think clearly, learn, and remember — is essential in helping us live happy and fulfilling lives. Maintaining our cognitive health can become a challenge as we get older, and many people experience what is known as age-related cognitive decline. Like the physical changes that occur in our bodies (e.g., stiff joints, wrinkles, etc.), our brain also experiences age-related changes over time.
You may notice you’re struggling to pay attention, for example, or find you’re having trouble recalling conversations or people’s names. These experiences are a natural part of aging and manifest as a condition coined age-related cognitive decline.
Understanding Age-Related Cognitive Decline Symptoms
According to the Centers for Disease Control and Prevention (CDC), cognitive decline is a self-reported experience of “worsening or more frequent confusion or memory loss.” It’s considered one of the earliest symptoms of Alzheimer’s disease and other related dementias, although it’s important to know that these conditions aren’t inevitable.
While experiences may be different person-to-person and can vary daily in scope and severity, common age-related cognitive decline symptoms include the following areas:
- Memory: Forgetting names, dates, and places becomes more frequent. You may place items in odd locations, like putting the car keys in the refrigerator
- Language: Forming words, phrases, or sentences becomes increasingly more challenging.
- Thinking or judgment: You may lose track of time or your train of thought. Making decisions can become more difficult or overwhelming.
- Apathy: An often-overlooked symptom. You may suddenly lose interest in your favorite activities or give up when an activity feels difficult. This can signal a mental withdrawal during the decline process.
- Incessant rumination: People experiencing cognitive decline can feel chronic stress or get stuck in a fight-or-flight response.
If you are experiencing any of these symptoms, take the opportunity to have a conversation with an Aviv Clinics physician to assess their severity and discover how you may be able to improve your cognitive health.
Have you noticed changes in your memory, attention or thinking skills?
Download our free e-book, “What’s Happening to My Brain?” to learn how you can improve your brain health and cognitive vitality at any age.
The Causes of Age-Related Cognitive Decline
There are four main reasons age-related cognitive decline may occur:
- Hormonal fluctuations: As we age, it’s natural for hormonal imbalances to happen. Research indicates these changes can be a key factor in the decline of cognitive function.
- Stroke or head injuries: Head injuries or a stroke can damage blood vessels in the brain, which may incite cognitive impairment and even vascular dementia. Even a minor head injury sustained many years ago increases your chances of developing dementia.
- Psychiatric disorders: Disorders like depression and anxiety have been connected to cognitive and functional decline. They are commonly experienced by patients with mild cognitive impairment (MCI) and can either be a contributing factor or a symptom.
- Heart conditions: Research shows that those in their 40s to early 60s with high blood pressure have a higher risk of experiencing cognitive decline later in life. Lowering blood pressure decreases the risk for MCI.

Age-Related Cognitive Decline vs. Dementia and Alzheimer’s Disease
Approximately 12% to 18% of individuals over age 60 live with mild cognitive impairment. If left untreated, MCI can bring on various disorders related to more significant age-related cognitive decline.
Approximately 10% to 15% of people with MCI develop dementia every year. Dementia is an umbrella term that encompasses a variety of neurological conditions. These conditions negatively affect the brain. In essence, nerve cells stop functioning normally and eventually die, causing cognitive decline.
There are different types of dementia, such as:
- Alzheimer’s disease: Those with MCI are at greater risk of developing Alzheimer’s disease — the most common dementia diagnosis. In addition to cognitive decline, those with Alzheimer’s may experience shifts in behavior and personality. Read about the risk factors for Alzheimer’s disease.
- Frontotemporal dementia (FTD): FTD can occur when there is damage to the frontal and temporal lobes of the brain. Someone with FTD can show unusual behaviors, emotional problems, and difficulty communicating.
- Lewy body dementia (LBD): LBD is a condition caused by a buildup of Lewy bodies (a protein) in the brain. Common symptoms of LBD include movement issues (e.g., slowed movements, stiffness, tremors), cognitive issues, and mood shifts.
- Vascular dementia: A lack of blood flow to the brain can cause vascular dementia. People with this condition typically experience issues with reasoning, planning, judgment, and memory.
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a simple blood test available at Aviv Clinics may be able to answer this question: pTau Testing
How to Slow Down Age-Related Cognitive Decline
Your brain is your superpower, but energy (in the form of oxygen and proper nutrition) is needed to make it perform like a superhero. If you give your brain energy, especially as you age, you can effectively slow down the aging process.
Aviv has developed a way to harness the power of oxygen using Nobel Prize-winning research. The Aviv Medical Program can incorporate a variety of therapies, including a specialized protocol of Hyperbaric Oxygen Therapy (HBOT). This protocol involves sending 100% pure oxygen to your deprived brain cells and body tissues, turbocharging your body’s own regenerative mechanisms through a phenomenon known as the hyperoxic-hypoxic paradox. In essence, this protocol deceives your body into believing it is deprived of oxygen, causing to to release healing factors to repair damage in your brain. Potential results include angiogenesis (new blood vessels), neurogenesis (new nerve and brain cells) and neuroplasticity (the brain’s capacity to rewire itself).
If you’re concerned about age-related cognitive decline, either in yourself or a loved one, contact Aviv Clinics in Florida today.
Last Update: August 8, 2025
Long COVID Symptom List: What They Are, Why They Persist, and What Helps
Millions of people who tested positive for COVID-19 continue to experience ongoing health issues, clinically known as long COVID. If you’re one of these people, you may experience a range of issues found on the long COVID symptoms list, including fatigue, shortness of breath, brain fog, aches and pains, and other symptoms.
While there is still uncertainty surrounding COVID-19 complications and their long-term side effects, extensive studies offer insight into:
- Post–COVID symptoms
- How long COVID can impact your body and lifestyle
- Treatment methods that can help mitigate long-haul COVID effects
It can be incredibly challenging to navigate these symptoms and find strategies to manage them. Rest assured, there is hope. To help those experiencing long COVID, Aviv Clinics has research-backed information on what the condition entails and what you can do.
What is Long COVID?
Long COVID refers to continuing signs and symptoms that persist, or even develop, after recovering from a COVID-19 infection. In some cases, symptoms may appear to disappear, only to return after a matter of days or weeks.
Below, we detail what long COVID is, how it affects your body, and what you can do to treat it.
As you read through this, keep in mind:
- Each person has a unique experience with COVID-19.
- Therefore, speaking with a doctor is an essential first step.
- Several alternative terms are used for long COVID, such as post-COVID, long-haul COVID, post-acute COVID, and chronic COVID.
How the CDC and WHO Define Long COVID
Throughout the pandemic, these agencies collaborated to monitor and support public health. Based on the list of long COVID symptoms, the CDC and WHO have addressed long COVID as an ongoing health concern:
- The Centers for Disease Control and Prevention (CDC) defines long COVID as a “chronic condition that occurs after SARS-CoV-2 infection and is present for at least 3 months.” They note further that symptoms can last for weeks, months, or years after their first infection.
- The World Health Organization (WHO) defines long COVID as “the continuation or development of new symptoms 3 months after” the acute infection that lat for at least with no other explanation for those symptoms.
Some estimates put the number of people living with long COVID at “65 million individuals worldwide,” with cases increasing daily.
Acute vs. Long-Term COVID Symptoms
Many of the symptoms of an acute COVID infection overlap with common ailments found on the long COVID symptoms list. For a comprehensive understanding of what long-haul COVID is, it’s important to note some differences between acute COVID symptoms and the symptoms of long COVID.
Acute COVID Symptoms
- Acute COVID is the initial phase of a COVID-19 illness, when a person is actively infected with the virus.
- During this phase, people commonly experience respiratory symptoms such as cough, fever, and difficulty breathing.
- Individuals may experience COVID-19 symptoms for up to four weeks, starting from the onset of illness.
- The virus can still be found in the body for up to 12 weeks, with people experiencing subacute COVID symptoms.
Long COVID Symptoms
- Long COVID involves ongoing or new symptoms that continue after an acute COVID infection has subsided.
- Individuals continue to experience COVID-19 symptoms for an average of three months from the onset of illness, sometimes longer.
- Long-haul COVID symptoms may either begin after initial recovery from acute COVID or persist from the initial illness.
- Long COVID symptoms cannot be explained by an alternative diagnosis.
How Common is Long COVID?
In 2021, the WHO released the first clinical definition of long COVID, more than a year after patients coined the term in the face of ongoing symptoms. From nearly the beginning of the pandemic, health organizations studying the virus were seeing long-term side effects and symptoms of impairment from COVID-19 infections.
You aren’t alone if you don’t feel like yourself after having COVID-19. New data suggests that among those who have reported a COVID-19 illness, “nearly one in five (19%)…are currently still having symptoms” months after they first caught the virus.
While many long COVID cases may go undocumented, researchers have estimates for its prevalence:
- Between 10–30% of nonhospitalized cases
- Between 50–70% of hospitalized cases
- Between 10–12% of vaccinated cases
By other estimates, anywhere from “31%–69% of COVID-19 survivors will experience long COVID symptoms after initial recovery.”
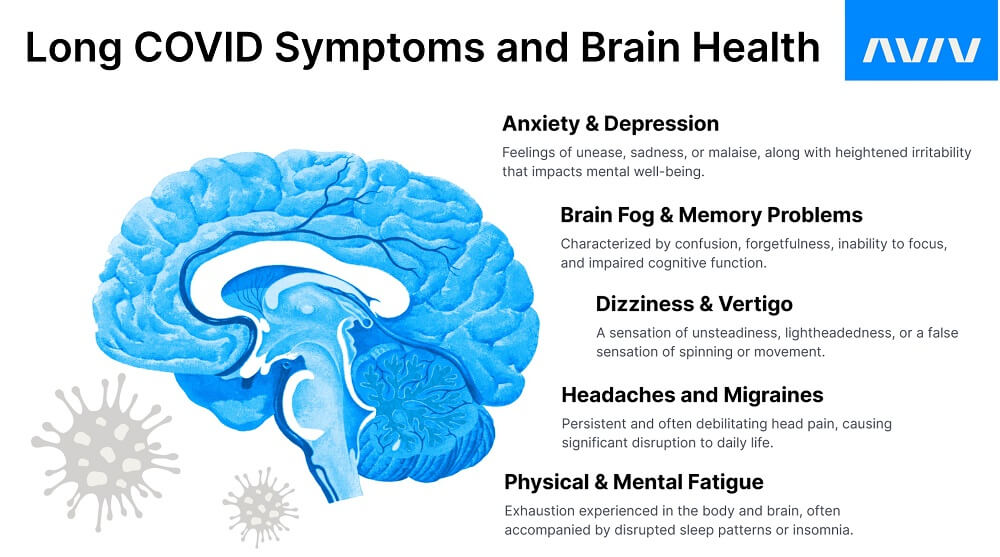
Long COVID Symptoms List
By scrutinizing four key areas from the long COVID symptoms list, patients can better understand the symptoms associated with long-haul COVID.
Physical symptoms:
- Fatigue
- Dyspnea (labored breathing)
- Chest pain or tightness
- Cough
- Dysgeusia (loss of taste)
- Anosmia (loss of smell)
- Joint or muscle pain
Cognitive & psychological symptoms:
- Memory decline
- Attention and concentration difficulties
- Brain fog
- Anxiety
- Depression
- Sleep disturbances
- Headaches
- Generalized disabling pain
- Lung symptoms
- Shortness of breath
- Chest pain or tightness
- Vertigo
Cardiac symptoms:
- Myocarditis (inflammation of heart muscles)
- Heart palpitations
- Shortness of breath
- Elevated blood pressure
- Drops in oxygen saturation
Can Long COVID Symptoms Come and Go?
According to current research, yes, long COVID symptoms can come and go over time. Some people may experience periods of improvement, where symptoms lessen or seem to disappear, followed by a relapse or a return of symptoms. In some cases, this relapse can mean a worsening of symptoms. These fluctuations are common in people living with long COVID, with most people reporting “fluctuating (57.7%) or relapsing symptoms (17.6%).”
How Long Until COVID Symptoms Go Away?
The duration of COVID-19 symptoms, in both acute and long-haul cases, vary widely from person to person. Most mild cases resolve within a couple of weeks. Long COVID cases are less predictable. As of now, “more than 200 symptoms have been identified with impacts on multiple organ systems.”
The nature of long-haul COVID, and the way it affects one individual compared to another, suggest that treatment and resolution of symptoms may rely on many personal factors.
If you are experiencing long COVID symptoms, contact our team of certified medical professionals today.
Why Long COVID Symptoms Persist
The persistence of COVID-19 symptoms can be attributed to several factors.
1. Ongoing Inflammation
The initial COVID-19 infection triggers an immune response in the body that results in inflammation. For some people, this immune response continues even after the virus has been cleared.
2. Immune Dysregulation
COVID-19 can affect the immune system long after the initial infection. Long COVID patients can experience immune dysregulation that remains “persistently high at eight months after the infection.”
3. Post-Viral Syndrome
Many viral infections can cause a condition known as post-viral syndrome, which is defined by the presence of persistent symptoms after fighting an infection. This may be the case with the COVID-19 virus.
4. Autoimmunity
Some people may develop an autoimmune response, where the immune system mistakenly attacks healthy cells and tissues. While it’s far from certain, “one theory is that long COVID could be an autoimmune disease” itself.
5. Persistent Viral Presence
Some studies suggest that fragments of the virus can remain in some tissues of the body after recovery of the initial infection. After one year, viral proteins and/or RNA can be found in various bodily systems in some long COVID patients.
Long COVID affects more than just the respiratory system. As stated above, lingering symptoms can affect the cardiovascular, neurological, gastrointestinal, and musculoskeletal systems. Recent research has found that people with long COVID are “at increased risk of a range of cardiovascular disorders,” among other issues.
Of particular concern is the impact of COVID-19 on brain health, specifically because of the presence of many brain-related ailments on the long COVID symptoms list.

Long COVID and Its Effects on Brain and Body
Essentially, COVID-19 impacts the brain. This is why the majority of long COVID symptoms are cognitive and may lead to brain injuries, depending on how severely your body is affected by the virus. According to Dr. Mohammed Elamir, MD, FACP, although there are no patterns between the severity of COVID-19 and the likelihood of experiencing long COVID, there are patterns between:
- Where the virus attacks the brain
- How long COVID symptoms are impacted by that region of the brain
Here are four ways that connection can manifest.
1. Direct Brain Invasion
The COVID-19 virus travels through the nose, into the olfactory sensory neurons, and into the insula, which is located between the frontal and temporal lobes of your brain. The olfactory neurons manage taste and smell, while the insula oversees an “overwhelming variety of functions,” including memory and executive function. Depending on where the virus attacks and the level of damage it creates, an individual may experience prolonged COVID symptoms.
For example, when the virus significantly attacks your olfactory nerves, this may induce a loss of taste and smell. This is why these symptoms are such a strong indicator of the virus.
2. Blood Vessel Injury
Studies show COVID-19 can result in “microvascular injury in the brain.” In other words, it can injure blood vessels that feed blood to the brain. As the virus circulates throughout your bloodstream, the inner blood vessel lining is susceptible to damage. When the inner lining deteriorates, this allows the virus to seep into the tissues or inhibit blood flow to the brain. Both can cause brain injuries. And depending on where those injuries occur, specific brain functions (memory, concentration, etc.) may decline more rapidly than normal.
3. Dysregulated Immune Response
Damage to the inner blood vessel lining can also inhibit the growth of cells, the exact opposite of what our immune system should be doing. Dysregulated immune responses are common, with “marked dysregulation in severe cases” of COVID-19. When the body cannot adequately produce a normal immune response, it either:
- Underreacts to foreign invaders, causing viruses to spread quickly
- Overreacts to foreign invaders, causing the immune system to attack even healthy cells, tissues, and organs
4. Cellular Dysfunction
On a cellular level, COVID-19 can affect metabolic function through the mitochondria. This cell damage slows the body’s response rate to infection, leading to high inflammatory conditions.
How Long Will Patients Have to Deal with COVID Symptoms?
According to Dr. Mohammed Elamir, MD, FACP, the answer isn’t available. But a key guiding factor is the extent of blood vessel damage.
Dr. Elamir explains:
“There’s still a lot to learn about how [mitochondrial dysfunction] will last, but it will probably be tied to the level of microvascular change or blood vessel damage. The more blood vessel damage you have, the more [long COVID symptoms] you’re likely to have. Also, the amount of real estate that those microvascular changes are occupying will probably dictate how long [symptoms] will last.”
WATCH: Long COVID Treatment at Aviv Clinics
How Aviv Clinics Supports Long COVID Recovery
Long COVID is a complex condition with a wide range of symptoms that vary significantly from person to person. That’s why treatment must be just as personalized.
At Aviv Clinics, our medical team takes a highly customized approach to care, starting with a conversation and evolving into a treatment program designed specifically for you.
Because of the complexity of long COVID, it’s important to find a treatment program that:
- Is rooted in data and research
- Offers a comprehensive assessment process
- Connects you with a diverse medical team
While many clinics offer a standard treatment program for long COVID, the Aviv Medical Program is built differently: we begin with a physician-guided evaluation to determine exactly which assessments and therapies are appropriate for your specific symptoms, goals, and medical history.
Depending on your needs, your board-certified Aviv physician will prescribe a personalized treatment program that may include one or more of the following:
- Hyperbaric oxygen therapy using our evidence-based protocol
- Cognitive training
- Physical therapy
- Nutrition coaching
- Neuropsychological support
- Other physician-recommended therapies
The goal is to reduce symptoms, restore cognitive and physical function, and help you feel like yourself again, all with a focus on sustainable improvement and long-term health.
Many individuals with long COVID symptoms, including fatigue, brain fog, memory loss, and cardiovascular complications, have experienced meaningful improvements after completing the Aviv Medical Program.
Watch Danielle’s recovery story to see what’s possible.
Diagnosis and Management of Long COVID
There is no single test that can definitively diagnose long COVID. At Aviv Clinics, your diagnosis starts with a detailed consultation and clinical evaluation by our physicians. From there, we focus on identifying the causes of those symptoms, whether neurological, physical, metabolic, or psychological, and then select therapies that target those mechanisms.
Depending on your symptoms, management strategies may include:
- Cognitive and psychological support to restore brain function and address brain fog, memory loss, anxiety, depression, or emotional strain.
- Physical therapy or physiotherapy to restore stamina, balance, strength, and ability to function daily.
- Nutritional strategies to improve energy and reduce inflammation.
- Targeted symptomatic treatments to address pain, sleep disruptions, or challenges with lung function
- Hyperbaric oxygen therapy delivered with a specific protocol to restore blood flow and oxygen to brain and body tissues
Multiple forms of support can be found through the Aviv Medical Program. Instead of a one-size-fits-all solution, our program relies on a multidisciplinary team that delivers a personalized care plan grounded in science and data.
The Future Outlook for Long COVID Patients
Looking ahead, the future for long COVID patients holds promise. As researchers and medical professionals continue to study the condition and its effects, the medical community gets closer to understanding the mechanisms behind long COVID. New treatment strategies are emerging to target those root causes, rather than masking symptoms.
At Aviv Clinics, our medical team is at the forefront of this research. If you live with symptoms of long COVID, know that recovery is still possible. With the right support and a personalized plan, many patients are reclaiming their cognitive function, energy levels, and quality of life.
Maximize Your Health and Performance with Aviv Clinics
The lasting impacts of COVID-19 don’t have to define your future. Though COVID-19 may have brought ongoing health challenges, the Aviv Clinics team is here to help you and your loved ones get back to optimal health. The Aviv Medical Program delivers a data-driven, personalized protocol to enhance your mind and body and feel like yourself again.
Our team is here to support you every step of the way. Contact our clinic to schedule a free phone consultation and learn whether the Aviv Medical Program is right for you.
Maximizing your health and performance begins with Aviv Clinics.
Last Update: July 16, 2025