Understanding Alzheimer’s Risk: Causes, Prevention, and the Promise of Hyperbaric Oxygen
Understanding Alzheimer’s Risk: Causes, Prevention, and the Promise of Hyperbaric Oxygen
Last Updated July 8, 2025
We all experience occasional memory lapses, especially as we age. For most of us, these minor cognitive issues are usually just annoyances. But if your cognitive issues interfere with your daily life, they could be the beginning of something much more serious.
Read on to learn more about the risk factors for Alzheimer’s disease and how you can preserve your cognitive health.
What Is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia that impacts a person’s ability to think, reason, and remember. As it progresses, Alzheimer’s can severely affect quality of life, eventually becoming completely debilitating.
The most common type of Alzheimer’s disease is the late-onset form, when symptoms usually “become apparent in [a person’s] mid-60s or later.”
10 Early Signs and Symptoms of Alzheimer’s Disease:

According to the Alzheimer’s Association, ten early warning signs of late-onset Alzheimer’s disease include:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks
- Confusion with time or place
- Trouble understanding visual images and spatial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgment
- Withdrawal from work or social activities
- Changes in mood and personality
If you experience a cognitive problem that impacts your daily life, don’t ignore it. Dementia is not a normal part of the aging process. The sooner you seek help, the sooner you can take action against cognitive decline.
Get in touch with our care team>>
What Are the Risk Factors for Alzheimer’s Disease?
Science is still learning how Alzheimer’s disease develops and why some people are at greater risk of developing it than others. It’s an active area of study, and researchers are making new discoveries every day.
The consensus among scientists is that a combination of age, sex, genetic, environmental, and lifestyle factors all contribute to the development of Alzheimer’s disease.
Let’s take a closer look at some of the greatest risk factors for Alzheimer’s:
- Although old age does not directly cause Alzheimer’s disease, the risk of developing Alzheimer’s “doubles about every 5 years” after age 65.
- More women than men develop Alzheimer’s disease, although this may be because women live longer than men on average.
- Suffering from a traumatic brain injury (TBI) can increase the long-term risk of developing Alzheimer’s or another type of dementia.
- Acute and chronic inflammation are both associated with an increase in cognitive decline. Eating a diet full of inflammatory foods like processed sugar may exacerbate the risk of developing inflammation in the brain.
- Exposure to environmental pollutants has been linked to an increased risk of dementia. Some researchers believe that nearly half of the individual differences in Alzheimer’s risk may be because of environmental factors.
- Being a smoker carries a significantly increased risk of developing Alzheimer’s disease. This risk factor offers another compelling reason to quit.
- People with Down syndrome also have a greater risk of developing Alzheimer’s disease. About 30% of people with Down syndrome develop Alzheimer’s disease by their 50s. The risk reaches closer to 50% in their 60s.
The Role of Brain Proteins in Alzheimer’s: Amyloid Plaques and Tau Tangles
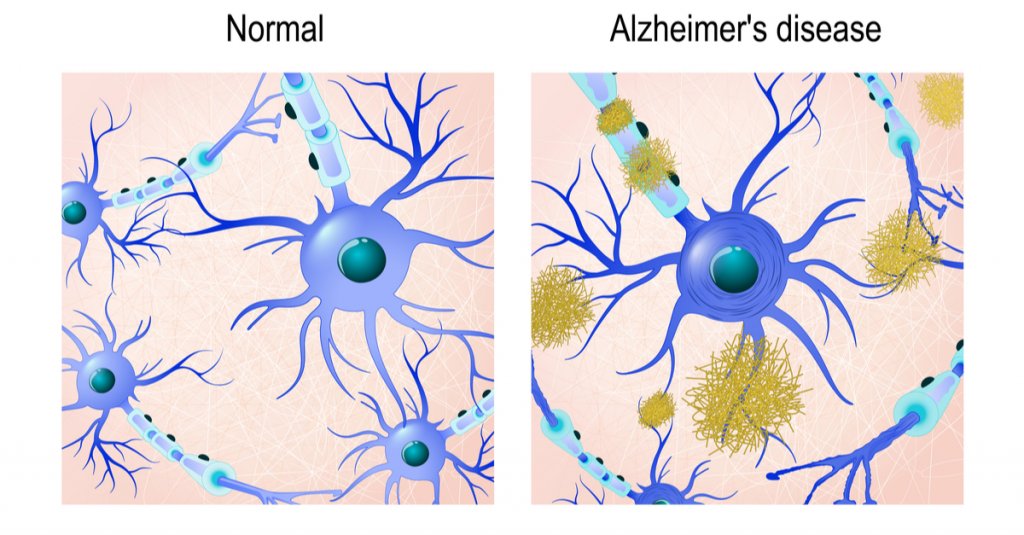
Scientists typically focus on two different protein structures in the brain associated with Alzheimer’s disease: Neurofibrillary tangles and amyloid plaques.
It’s not currently known whether the presence of these structures causes Alzheimer’s disease or if they’re simply byproducts of it. But both can impair cognitive function and can worsen as the disease progresses.
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a simple blood test available at Aviv Clinics may be able to answer this question: pTau Testing
Neurofibrillary Tangles
Neurofibrillary tangles are accumulations of a harmful protein called tau in the brain’s neurons. These tangles can inhibit the neurons’ ability to communicate, causing cognitive decline. Some studies reveal that a lack of oxygen to the brain is associated with neurofibrillary tangles.
Amyloid Plaques
Amyloid plaques are hard, insoluble clumps of beta-amyloid proteins that build up between neurons. Like neurofibrillary tangles, these plaques are toxic to brain cells and disrupt cell-to-cell communication. They can eventually result in cellular death, harming cognitive abilities even further.
Brain scans can reveal the presence of both protein structures, so your doctor can alert you to the presence of Alzheimer’s disease or if you’re at risk for developing it.
Is Alzheimer’s Disease Genetic?
Both early-onset and late-onset Alzheimer’s disease have a genetic component, meaning if you have a family history of Alzheimer’s, you carry a greater risk for developing the disease. The risk factor is greater if an immediate family member suffers from the disease, such as a parent or sibling.
Genetics are almost always the primary contributing factor of early-onset Alzheimer’s disease, which can affect people as young as their 30s or 40s.
Gene Mutations
Researchers have yet to identify any specific genes directly responsible for the development of late-onset Alzheimer’s. However, certain mutations of the APOE gene, which are found in chromosome 19, are currently considered the strongest genetic risk factor for Alzheimer’s disease.
For example, the specific gene mutation APOE ε4 is linked to higher levels of amyloid plaques and is often found in people with Alzheimer’s disease.
Your doctor may order genetic testing if you have a family history of cognitive problems or early-onset dementia.
Remember, this doesn’t mean you’re destined to develop Alzheimer’s if a parent or sibling has had it. Some people who possess the APOE ε4 gene never develop Alzheimer’s disease, and some people with Alzheimer’s don’t have any gene mutations at all.
Genetics is just one of many Alzheimer’s risk factors. We still need more research to develop a complete picture of what the largest risk factor for Alzheimer’s disease is.
Can Hyperbaric Oxygen Therapy Help Prevent Alzheimer’s Disease?

A specific hyperbaric oxygen therapy (HBOT) protocol shows promise as a potential preventative measure for Alzheimer’s disease. HBOT is a treatment that involves breathing 100% oxygen in a pressurized chamber to increase oxygen levels in the body and brain. A unique HBOT protocol used at Aviv Clinics has shown several benefits in individuals at risk for or experiencing early cognitive decline:
Benefits of HBOT for Alzheimer’s Disease:
- Improves brain tissue oxygenation
- Lowers neuroinflammation (inflammation in the brain)
- Shrinks beta-amyloid plaques (in laboratory animals)
- Reduces pTau protein levels (in laboratory animals)
- Improves memory recall and cognitive performance
- May slow or reverse early signs of cognitive decline
These benefits have been documented in peer-reviewed studies. This specialized HBOT protocol is available exclusively at Aviv Clinics in Central Florida.
In one study, repeated HBOT sessions showed reduced brain hypoxia, reduced amyloid plaques and pTau, and improvements in cognitive performance. Another study found improvements in memory recall in people with mild cognitive impairment (MCI), a potential early stage of Alzheimer’s. Researchers concluded that HBOT “should be considered as a therapeutic approach to slow the progression or even improve the pathophysiology responsible for [Alzheimer’s] disease.”
Lifestyle Habits That May Lower Your Alzheimer’s Risk
While none of us can change our genetic makeup, we can change our lifestyle. Healthy habits can help lower your risk factor for nearly any disease, not just cognitive conditions. Lowering inflammation levels in your body can also help lower inflammation in the brain. To help preserve your cognitive health:
- Eating a healthy diet full of fruits and vegetables
- Exercising regularly
- Maintaining healthy blood pressure
- Keeping your mind active
- Maintaining a healthy weight
- Practicing mindfulness and meditation
- Avoiding excess alcohol
- Avoiding smoking
- Getting plenty of restful sleep
- Taking care of your mental health
How the Aviv Medical Program Can Support Brain Health
The Aviv Medical Program is a personalized intervention designed to improve brain and body health. Using the unique HBOT protocol discussed earlier, alongside other evidence-based interventions, this program can treat both physical and cognitive performance in older adults. In clinical trials, this protocol has also reversed key biomarkers of the aging process.
Depending on your symptoms, needs, and goals, our clinical team will perform an assessment that may include:
- In-depth medical history review
- Comprehensive physical and neurological exam
- Physical therapy evaluation
- Highly advanced brain imaging scans
- Neurocognitive tests
Once our board-certified physicians review your results, they’ll prescribe a customized treatment program designed to treat your concerns. This program may include:
- A specialized hyperbaric oxygen therapy protocol
- Physical training
- Dietary coaching
- Cognitive exercises
- Other interventions as prescribed
Real Client Results: Carl and Vickie’s Cognitive Improvements
Married couple Carl and Vickie both had parents with dementia and cognitive decline. They soon realized they were beginning to experience the same cognitive issues that they saw in their parents.
The couple’s quality of life was not where it should have been, so they took action with the Aviv Medical Program. They use one word to describe their improvements in cognitive performance: “remarkable.”
I’m dancing, I’m hiking, I’m running again. It’s just remarkable. I don’t know how else to say it.” –Vickie Eckert, Aviv Medical Program Alumna
Take Control of Your Brain Health With Aviv Clinics
While science is still investigating all of the risk factors for Alzheimer’s disease, anyone can lower their likelihood by taking charge of their lifestyle.
Preserving your cognitive health starts with the choices you make every day. Partnering with Aviv Clinics is just one of them. Contact our medical team to learn how we can help you.
Technology and Brain Health: How Screen Time Affects Focus, Memory, and Mental Clarity
Last Updated July 7, 2025
Technology is advancing at a shockingly rapid pace. Screens are now a staple of our daily lives — we interact with them everywhere: at home, in the office, and in our pockets. We use them to communicate, conduct business, shop, entertain ourselves, and more.
Between booming technology, the ever-increasing pace of life in general, and rising rates of ADHD diagnoses, many people may wonder if our attention spans are diminishing. Could technology be negatively affecting our brain health?
To some extent, we aren’t sure yet how technology affects us, cognitively or socially.
Experts have warned against the maladies of screens ever since the television became a staple of the American living room almost 70 years ago. Passive television watching, however, may not compare to the technological onslaught of modern culture.
In a world where everyone has a supercomputer in their pocket that provides access to the entirety of accumulated human knowledge via the internet, what’s happening to our brains?
Here is what we know so far about technology and brain health, as well as strategies for adapting to this new normal.
Is Technology Causing ADHD Symptoms in Adults?
If it seems like everybody you know has ADHD (attention deficit hyperactivity disorder) lately, you might not be imagining it. From 2007 to 2016, rates of adult ADHD diagnoses doubled. Although most studies on screen time involve children, the correlation between screens and poor attention in adults is nonetheless present.
It should be noted that these studies are not necessarily saying that people who use screens often will “develop” ADHD. ADHD is a neurological condition that a person is born with and that often persists through childhood into adulthood. It represents a different “wiring pattern” in the brain.
However, these studies demonstrate that screen time and media use are highly correlated with symptoms of ADHD. In other words, while the underlying mechanism might be different from true ADHD, too much screen time leads to something that looks a lot like ADHD.

The main symptoms of ADHD are:
- Short attention span, especially for non-preferred tasks
- Hyperactivity, which may be physical, verbal, and/or emotional; can also manifest as fidgeting or restlessness
- Impulsivity
- Disorganization and difficulty prioritizing tasks
- Poor time management and time blindness
- Frequent mood swings and emotional dysregulation
- Forgetfulness and poor working memory
- Trouble multitasking and executive dysfunction
- Inability to control anger or frustration
- Trouble completing tasks and frequent procrastination
- Distractibility
- Difficulty awaiting turn
(If you have several of these symptoms, it’s worth discussing them with your doctor.)
Part of the rise in diagnoses could be due to increased awareness and education. Some adults may realize they have always struggled with these symptoms. For an ADHD diagnosis, symptoms must have been present in childhood, even if they were initially missed.
As an adult, if you “suddenly” develop ADHD-like symptoms that weren’t there before, there may be many reasons for these new cognitive or attentional issues.
Cognitive Decline vs. Screen Overload: What’s Really to Blame?
If you think your attention is suffering, ditching screens may or may not be the ideal solution. When it comes to impaired cognitive function, there are other causes that also should be considered.
Normal aging will cause some minor changes in cognition, including slowed processing speed, taking longer to learn new information, and an increase in distractibility, for example. But normal aging shouldn’t impair daily functioning.
Forgetting a name on occasion isn’t a cause for concern, but repeatedly forgetting the same information, on the other hand, could be a symptom of mild cognitive impairment (MCI). Although MCI rates increase with age, cognitive impairment isn’t inevitable for everybody of advancing age.
Other factors can contribute to MCI, including:
- Depression, stress, and anxiety
- Thyroid, kidney, or liver problems
- Sleep apnea and other sleep disorders
- Diseases or conditions that affect blood flow in the brain
- Low vitamin B12 levels or other nutrient levels
- Eye or hearing problems
- An infection
- History of alcoholism
Stress can also contribute to deficits in cognitive abilities such as short-term memory loss and brain fog. Self-care, including looking after your physical, mental, emotional, intellectual, and social health, is critical for brain health.
Is Technology Making Our Brains Lazy?

Some might argue that the tools of technology have become our crutches. For example, most of us no longer bother to remember phone numbers. A smartphone can remember vastly more information than our brain could ever hope to remember.
There are many challenges to studying the effects of technology and brain health, whether on the biology of the brain or the impact on society, that make this question difficult to answer. Experts are divided, with some seeing technology as a boon to society and others taking a more cynical view.
The one thing both sides agree on is technology’s ability to exploit the inherent human tendency towards laziness and the “quick fix.” As evolutionary geneticist David Krakauer said, “I’m most concerned about the unthinking acceptance of convenient short-term solutions.”
The human brain, in an attempt to be energy-efficient, often chooses the thing that benefits us immediately, foregoing potentially greater future benefits.
Persuasive Technology: How Social Media Hijacks Your Attention
Social media platforms, such as Facebook, Instagram, and Twitter, drive the progress of technology, particularly artificial intelligence (AI), in a way that targets our subconscious minds. After analyzing billions of data points collected each time you swipe, click, or tap online, social media platforms and other websites know you better than you know yourself.
Tristan Harris, president and co-founder of the Center for Humane Technology, calls this “persuasive technology,” or “technology that shapes attitudes and behavior.” By exploiting natural human psychological vulnerabilities, the website explains, “it begins to train us: our thoughts, feelings, motivations, and attention start to replicate what the technology is designed to produce.” This all happens beneath our level of conscious awareness, and yet it’s guiding our behavior; this presents, they argue, a very real threat to personal autonomy.
As these platforms learn your habits, they know exactly what to show you next to keep you scrolling. Thought you were going to breeze through social media in 15 minutes, and 2 hours later, you’re still there? That’s because your 50,000-year-old brain is trying to compete with the most complex supercomputers ever made.
How to Take Control: 3 Strategies to Improve Brain Health
How do you know if you need a break from screens?
Awareness is key for any form of self-improvement. If you look at your screen habits and find that you’re missing out on too much of your life and relationships in favor of screen time, here are three ways to reduce or counter the effects:
1. Spend More Time in Nature to Support Brain Function
Technology has many merits, but one way in which it causes collateral damage is that we tend to stay indoors to use it.
The average person spends up to 93% of their time indoors or in an enclosed vehicle. For a species that has spent most of its history as homeless nomads who knew only nature, transitioning to an indoor concrete jungle is not without consequences for our health. Getting out into nature can have a profound effect on our physical, mental, and emotional health.
Richard Louv, a journalist and author who coined the term “Nature Deficit Disorder”, summarized the research on the effects of nature: “Nature is not only nice to have, but it’s a have-to-have for physical health and cognitive functioning.”
According to a 2019 study, two hours or more per week of nature exposure is enough to significantly improve reported well-being.
2. Try a Digital Detox to Reduce Screen Time and Improve Focus
While we may not understand the mechanisms involved with the brain and media use, we do know one thing: the brain performs its best when exposed to variety and balance. While some amount of educational media or video games can improve cognition, too much of anything can be a bad thing. The brain needs many different kinds of stimulation, or lack thereof, in order to run at its best.
There are lots of tricks and methods for cutting back on screen time, from charging your phone outside of the bedroom to full-on silent meditation retreats. Turning off push notifications for apps that profit from your attention (like social media) is another way to cut down on the number of dopamine hits you get from your phone.
Why target these apps in particular? Because each notification, despite typically being of relatively little importance, registers in our nervous system as a minor threat or alert. Turning off notifications can reduce the number of “pings” on your nervous system.
3. Focus on Quality Screen Time, Not Just Less Screen Time
Of course, technology has provided us with lots of conveniences that we have become accustomed to and may not want to sacrifice completely. If we can’t (or don’t want to) give up technology, are we doomed to fry our brains?
A lot of it might have to do with how we interact with the media, not just how much we interact. Although most studies have focused on the quantity of screen time in hours spent watching, not all screen time is created equally.
One question to ask when it comes to technology and brain health is:
How does the value of whatever you’re doing using technology compare to other things you could be doing?
Or put another way, what’s the tradeoff? If you have free time and feel like doing a deep dive into the biology of narwhals, for example, and that’s the best way you could imagine spending your time, no problem.
But if you’re still on Wikipedia at 3:30 am and you’re losing sleep — or you’re ignoring friends and family in favor of social media — it might be worth re-examining the relationship.
The Bottom Line: Protecting Brain Health in a Digital World
Technology is a fascinating and ever-changing tool of human creation. Like any tool, it can be used to confer great benefits, but used improperly has the potential to cause harm. As the pace of life quickens, it’s more important than ever to slow down, stay aware, and focus on balance.
Can Negative Thinking Hurt Your Brain? New Insights Into Cognitive Decline and Dementia Risk
Last Updated July 3, 2025
Can Negative Thinking Hurt Your Brain?
It’s no secret that negative thoughts are related to mental health conditions like depression and anxiety; in fact they’re pretty much required for diagnosis. We also know that depression and anxiety can increase your risk for dementia, including Alzheimer’s disease.
Of course, not all negative thinking leads to depression. There’s nothing inherently detrimental about negative thoughts — everyone needs to have some negative thoughts on occasion. We’re biologically equipped to handle a certain amount of negativity.
But as with most systems, it works under tight parameters. Taxing the system can throw it off balance. And when we get stuck in depressed rumination or anxious worry loops, we put ourselves at risk for physical health effects.
Repetitive negative thinking, it turns out, can lead to depression… but it also increases one’s risk for dementia all on its own.
Repetitive Negative Thinking and Dementia Risk
Although researchers have been aware of a relationship between depression or anxiety and dementia, the direction of the relationship wasn’t clear. Did depression or dementia come first? Or was there a third factor that affected them both?
In a recent study examining the effects of negative thinking on cognition, nearly 300 people aged 55 and over were tested and monitored over two years. Researchers measured cognitive skills such as attention, spatial cognition, language, and memory, as well as physical markers for cognitive decline. These markers included tau and amyloid proteins; higher levels of these proteins have been observed in patients with Alzheimer’s Disease (AD).
Are You At Risk of Developing Alzheimer’s Disease?
Learn how a blood test available at Aviv Clinics may be able to answer that question: pTau Testing
These cognitive factors were measured against the tendency to engage in repetitive negative thinking (RNT). The researchers found that RNT was causally associated with:
- A more rapid decline in global cognition
- A more rapid decline in immediate and delayed memory
- Higher levels of AD biomarkers (tau and amyloid proteins)
Repetitive Negative Thinking and Cognitive Debt
This study squares well with research that emerged in 2015 on the theory of “cognitive debt“. Depression, anxiety, PTSD, and other factors may contribute to cognitive decline and memory issues over a long, cumulative process.
The researchers proposed the theory of cognitive debt to explain how our thoughts and behaviors can lead to cognitive decline. They recognized that several related, but distinct, conditions (depression, anxiety, life stress, neuroticism, sleep disturbances, and PTSD) all shared increased risk factors for dementia.
But what precisely do they all have in common? The answer is Repetitive Negative Thinking.
The authors defined the term RNT to include both rumination (negative thoughts regarding past events) as well as worrying (typically future-related thoughts). They emphasized that the repetitive and negative nature of the thoughts, NOT their temporal nature, was key to the association.
Why?
The stress system gets chronically engaged due to RNT and accrues cognitive debt by affecting where your attention is focused.
The Brain’s Built-in Negativity Bias

Maybe you’ve been told before to just “look on the bright side” or “find the silver lining,” but somehow you end up still focusing on the negative. If that’s you, don’t feel discouraged. Humans come pre-equipped with a natural negativity bias.
Research has repeatedly shown that we’re more responsive to negative stimuli in the environment than positive stimuli. When making decisions, we tend to weigh the cons more heavily than the pros. In studies examining how we arrive at our impressions of others, the participants relied more on the negative traits when forming first impressions, even if positive traits were similarly intense.
That’s because our brains, which are constantly scanning the environment for potential threats, essentially throw away much of the positive data before it even reaches “you.”
Why would it do this? A few reasons.
Your Brain is Wired for Survival, Not Positivity
One of the main jobs of the brain is to act as a filter for stimuli coming from the physical world. Your brain is constantly bombarded with raw data: sights, sounds, and other incoming information. Only a fraction of this data ever reaches your conscious awareness, lest you be completely overwhelmed. The brain is forced to pick and choose what to let through and what to toss away.
Second, negative and positive information isn’t equally weighted from the brain’s perspective.
Consider your distant prehistoric ancestor foraging for edible berries, suddenly happening upon a ferocious wild animal looking for lunch. Recognizing a threat to survival, her brain directs her to hightail it back home. Do you think she had an opportunity to notice the beautiful sunset in the distance as she ran for her life?
Your brain isn’t in the business of being fair to reality. It doesn’t even distinguish between “good” and “bad” or make moral judgments. It’s distinguishing between things that need your attention and things that don’t.
In other words, it’s trying to keep you alive.
It’s human nature to filter out some of the positives. The good news is that while your subconscious brain may have designs on the negative, that’s just the default setting on your autopilot system.
In other words, you have the option to chart your own course.
Most of Your Thinking is Habitual — and That Matters
Researchers estimate that up to 95% of human activity is driven by the unconscious brain. Our brains are efficient, and consciousness is expensive, metabolically speaking. So if your brain detects a pattern (such as driving the same route to work every day), it’ll simply automate that for you, taking it off of your cognitive plate.
In other words, it forms a habit.
That means that 95% of the time, your brain is relying on your habits: past information, thoughts, and behaviors that you frequently engage in. Most of the time, you’re not actively deciding the course of your life.
How to Interrupt Negative Thought Loops
We do have the power to choose to take the wheel when it comes to negative thinking. By doing so, we can construct a more positive reality for ourselves.
We may not be able to fight biology and always be in the moment. But you can reprogram your autopilot so that it takes you where you want to go. With some tweaking, your autopilot can work for you, not against you.
It starts with choosing what to “feed” your brain. Whatever your brain experiences most will shape your unconscious, and thereby your thoughts and behaviors.
Take the idea of doomscrolling, which became so popular during the COVID pandemic that Merriam-Webster added it to the list of “words we’re watching.” Doomscrolling involves “the tendency to continue to surf or scroll through bad news, even though that news is saddening, disheartening, or depressing.”
What happens to a brain that’s exposed to hours of negative thoughts? Like a carrot in a stew absorbs the flavors of all the other ingredients, your brain soaks up all the elements of the environment around you: sights, sounds, thoughts, and emotions. It’s no surprise that doomscrolling can lead to patterns of negative thinking.
Train Your Brain to Think Differently
You can’t choose all of your thoughts, but you can choose what you’re exposed to. The more intentional you are with your environment, the more you can reprogram your brain. Here are a few ways to get started.

- Choose your circle. Humans are social animals, and if you surround yourself with negative people, you’re more likely to adopt negative thinking.
- Cultivate mindfulness. Before you can change anything, you have to be aware of it. On average, we may only be truly conscious and aware 5% of the time, but mindfulness can raise that number. Meditation and other mindfulness strategies are great for catching negative thinking in the act.
- Try cognitive reframing or reappraisal. If you’re able (using mindfulness) to catch a negative thought in the act, you can try reframing it. The idea isn’t to sugar coat anything, ignore or dismiss the negative, or invalidate feelings, because you’re grounded in reality–the idea is to question your assumptions and logic and consider if it’s worth rethinking. Try to approach it like a scientist, with nonjudgmental curiosity.
You might do the following once you’ve identified a troubling thought:
- Stop and observe the thought
- Consider the available evidence for the thought
- Question what emotions might be associated with the thought
- Consider that alternatives to this thought might exist
- Look out for thinking traps, but don’t blame yourself for falling into them–they’re traps, after all!
The Bottom Line: Change Your Thinking, Protect Your Brain
Left to our devices, humans tend towards the negative by nature. This gets programmed into our unconscious, and so we continue towards the negative — unless you choose to take steps against it.
Aviv Clinics combines neuropsychology with hyperbaric oxygen therapy and other personalized interventions to promote better brain health and cognitive resilience. As the only U.S. location offering the unique, evidence-based Aviv Medical Program, Aviv Clinics in central Florida empowers you to optimize your brain health with lasting results.
Based on nearly two decades of research and development, the intensive treatment program is customized to each client’s needs. Using in-depth assessments, our physicians prescribe a personalized plan for each client.
For a free consultation with one of our board-certified physicians, contact us.
Improving Brain Health Naturally at Any Age
Old Beliefs, New Possibilities: Can Bran Health Really Improve With Age?
When it comes to brain health, most scientists used to believe the old saying, “you can’t teach an old dog new tricks.” The long-held belief was that the adult brain lost the ability to grow after a certain age. In other words, the conventional wisdom believed that once we lost certain cognitive functions, they were gone forever. Fortunately, new research has revealed that improving brain health is possible at any age.
Not only is it possible to change your brain at any life stage, but you can improve your cognitive functions just by making a few simple lifestyle changes. Here’s how you can improve your brain health naturally, no matter how old you are!
What is Neurogenesis and Why Does it Matter for Brain Health?
The human brain is home to millions of hard-working neurons, or brain cells, firing their synapses to create connections. As we age, the number of neurons in our brains naturally begins to decline, which can lead to cognitive problems. You might find yourself forgetting where you put your keys more often, or struggling to solve a simple brain teaser that might’ve taken you minutes in earlier years. These small slips in your cognitive functions can become frustrating. They can interfere with your daily life, and even become outright debilitating over time. Fortunately, some people can recover their cognitive functions with a little help.
The creation of new neurons is called “neurogenesis.” New research suggests that the brain can continue to create neurons well into adulthood. The findings reveal that adults with Alzheimer’s disease have fewer neurons in their brains than neurologically healthy adults, suggesting that Alzheimer’s disease and a lack of neurons are directly connected.
Treatment options, like the non-invasive HBOT (hyperbaric oxygen therapy) protocol offered at Aviv Clinics, have been shown to stimulate neurogenesis in the adult brain, slowing and even reversing the effects of age-related cognitive decline. It’s also possible to stimulate neurogenesis on your own.
Neuroplasticity Explained: How Your Brain Adapts and Grows
When you experience something new, such as playing your grandkid’s favorite video game for the first time, the stimulation causes the neurons to form new pathways in your brain. The more you play the game and hone your skills, the stronger those connections become. This is “neuroplasticity”—the brain’s ability to change itself in response to new information. With neuroplasticity, your brain can rewire itself by changing its physical structure.
But neuroplasticity can do more than help you level up your gaming skills. Through neuroplasticity, the brain can even restructure itself after suffering an injury, such as a traumatic brain injury (TBI) or stroke, by forming new neural connections in undamaged parts of the brain. Building and strengthening your neural connections is a key aspect of maintaining brain health at any age. Here are a few ways to promote neuroplasticity you can try out at home.
5 Tips for Improving Brain Health Naturally
Eat for Your Brain: Foods the Fuel Neurogenesis
Think of the brain as your body’s engine. If you want your brain to run optimally, you need to give it the proper fuel. Eating processed foods high in saturated fat and sugar can stall neurogenesis, slow your thinking, or cause “brain fog” and other cognitive issues.
The good news is, eating a diet with foods that promote neurogenesis can improve your cognitive health. The omega-3 fatty acids in salmon and fish can increase neuron production. So can the flavonoids in foods like dark chocolate and fresh berries. Even the resveratrol in a glass of wine can give your brain a boost, although drinking in excess can have the opposite effect.
The amount of food you eat and how often you eat also have a role to play. Caloric restriction diets promote neurogenesis, and so do eating methods like intermittent fasting. Try a simple 16:8 fasting schedule and see if your cognitive functions improve.
Move to Improve: How Exercise Enhances Brain Performance
The brain and the body are intimately connected. When one is out of shape, the other can suffer. To give your brain an extra boost, try getting up and moving your body. Studies have shown that physical activity can promote neuroplasticity.
The skills you learn from playing sports like pickleball or golf can stimulate neural connections in your brain. Plus, the physical activity can improve your heart health and help you reach your recommended exercise. You don’t have to run a marathon to see results. The key is to find a physical activity you enjoy doing and to do it regularly. Your body and brain will both reap the benefits.
Learn Something New: Stimulate Neuroplasticity With Mental Challenges
Of course, you can also exercise your brain directly. Just like any other organ or muscle in your body, the brain needs regular stimulation to remain strong. Learning new skills is one of the key aspects of stimulating neuroplasticity in the brain. The possibilities for promoting new neural pathways are endless. You could learn to play a musical instrument, practice speaking different languages, try out a new recipe in the kitchen, or even take a class online.
Playing specialized brain games is one of the best ways to give your brain a good workout. Even solving a crossword puzzle or a challenging Sudoku game can provide extra stimulation. So long as your brain is facing a challenge, then you’re promoting the growth of new neural connections.
Calm the Mind: How Meditation Supports Cognitive Health
Meditation is more than just a way to calm down. It’s an activity you can use to hone your brain’s focus and concentration. Meditating can improve your ability to focus on cognitive tasks by training you to stay present in the current moment. Practicing mindfulness meditation can also ward off stress and anxiety, which can improve mental health. A calm brain is a healthy brain.
Meditation can even slow the progression of Alzheimer’s disease and increase memory recall. You can start seeing positive results in as little as a few weeks of regular practice. The next time you’re having a hard time concentrating, try meditating for a few minutes and see if your cognitive functions improve.

Sleep Smarter: The Role of Rest in Brain Repair
Just like every other age range, older adults need plenty of sleep. Sleep is the vital period when our bodies take the time to recharge after a hard day’s work. It’s when the brain consolidates memories, solidifies learned experiences, and cleanses itself of harmful waste. If you’re not getting enough sleep, you could be sabotaging your efforts to create new neural connections in your brain.
Practicing healthy sleep habits can promote neuroplasticity and improve your overall cognitive health. Try to fall asleep at roughly the same time every night to establish a routine. Avoid consuming caffeine too close to bedtime to prevent sleep disturbances. If you need a nighttime snack that can help boost your sleep, try reaching for a handful of almonds to spark your melatonin production!
The Aviv Clinics Advantage: Taking Brain Health to the Next Level
Cognitive decline doesn’t need to be inevitable as we age. With these consistent lifestyle interventions that promote neuroplasticity and neurogenesis, you can take control of your brain health at any stage of life.
For those seeking to go the extra mile to remain cognitively fit, the Aviv Medical Program offers an evidence-based personalized treatment protocol for brain and body health. The Aviv Medical Program harnesses the power of a unique hyperbaric oxygen therapy protocol and complementary therapies like cognitive exercises, physical training, and nutritional coaching to enhance brain performance. Backed by nearly two decades of published scientific research, this program is designed to help you regain mental sharpness and increase energy using a program personalized specifically for you. If you’re ready to take a proactive approach to brain health and aging, contact us to learn if the Aviv Medical Program can help you unlock your brain’s full potential.
Managing Chronic Pain Without Medications: 4 Mind-Body Strategies That Work
Last Updated July 2, 2025
Chronic pain is as much a psychological problem as it is a physical one because the mind and the body are linked. All pain originates as a signal in the brain, which is sent out to the body via the nervous system. Training your brain to respond differently to chronic pain can change the way your body responds to it.
According to the Institute for Chronic Pain, chronic pain is a type of pain that lasts for months or years on end. Unlike acute pain, which goes away once the underlying injury or illness subsides, chronic pain is a pain that has developed a life of its own.
Why Medication Alone Isn’t Enough to Treat Chronic Pain
When you’re in pain, you just want it to go away…fast. People often go to their doctors looking for a “magic bullet” to treat their chronic pain quickly. Unfortunately, chronic pain doesn’t work that way.
Although opioids are frequently prescribed for chronic pain, studies have shown that opioids are not an effective management tool. While they may provide relief in the short term, opioids can cause lasting problems in the long term and put patients at risk for dangerous addiction and overdoses. Older adults are especially vulnerable to the opioid epidemic.
It’s far more effective to take an active approach to pain management by using a combination of dietary changes, exercise, and cognitive-behavioral techniques.
Train Your Brain to Control Chronic Pain
Think of pain as an annoying neighbor. We’ve all had a neighbor we’d rather live without. It seems as if their very purpose in life is to be a nuisance to us.
You can hope that they’ll eventually move away, but chances are good that the neighbor will continue to live next door, and there is nothing you can do about it. Avoiding or hiding from them will only allow them to control your life. So, you have a choice to make.
You can avoid your neighbor forever, stuck inside the four walls of your own house. Or, you can invite them inside for a cup of coffee and make peace with them.
Chronic pain is like that neighbor. Unless you make peace with your pain, it can control your life. Re-think your pain with these four helpful and drug-free chronic pain relief techniques.

1. Mindfulness for Chronic Pain Relief
Mindfulness is an evidence-based technique with a proven track record of relieving chronic pain. In fact, all of these cognitive techniques incorporate principles of mindfulness.
Being mindful requires adopting an attitude of curiosity and non-judgment. It encourages you to look at your pain in an objective way and teaches you how to bear unpleasant sensations without emotional distress. Common mindfulness practices include:
- Meditation
- Breathing techniques
- Visualization exercises
- Awareness shifting techniques (see below).
2. Redirect Your Attention: Focus-Shifting Techniques for Pain Management
Sometimes the most effective way to stop yourself from thinking about your pain is to shift your awareness onto something else. The next time your chronic pain begins to flare up, try picking up a small object and examining it.
- Notice exactly how it feels in your hand.
- Pay attention to its unique shape, temperature, and texture.
- Does it feel rough or smooth against your skin? Is it hot to the touch, or cool? Are there any sharp edges, or is the surface completely rounded?
After a few moments of intensely focusing on the object, you may find that your chronic pain no longer feels as intense. That’s because you’ve actively shifted your focus away from the unpleasant sensation and replaced it with a different one.
3. Guided Imagery and Visualization for Pain Reduction
Guided imagery involves imagining a specific reality for yourself, rather than using a real object. If your pain is sharp and hot, you might envision a ball of cool white light enveloping your pain. Imagine exactly how this would feel using all five of your senses. Try to be as vivid as possible: Feel the cool ball of light washing over your body and soothing your pain.
While the ball itself isn’t real, the relief you feel just might be. Guided imagery has scientifically proven benefits for pain relief. It’s one of the most common techniques for those who suffer from chronic pain. You can envision nearly anything you like here, as long as the effect is soothing, relaxing, and positive. You can try guided imagery sessions on your own, with the help of a professional, or even through meditation apps and subscription services.
Another example of this technique is the pain circle. This visualization exercise can help you actively shrink the area of your pain. The next time your chronic pain flares up, try envisioning a circle around your pain. Ask yourself, where is the pain most intense? Does it hurt more on one side of the circle or the other? Are there any places inside the circle that don’t hurt at all?
By actively assessing the area of your pain, you can begin to redraw the boundaries of it. You’ll likely find that the area of your pain is smaller than you originally thought. It’s a mindful way to actively reframe the way you experience pain and put yourself back in control.
4. Support Brain-Body Healing With Nutrition and Movement

Remember that while these techniques are effective on their own, they work best in tandem with proper diet and exercise programs.
Eating a nutritious diet of whole foods can lower inflammation and stress levels, which can significantly improve chronic pain. Exercising regularly can also lower chronic pain levels. You don’t have to do anything too extreme. Even a simple walk around the block can help you feel better. Try practicing some of these mindfulness techniques as you walk. You might just be surprised at how far you can go.
Explore Non-Pharmaceutical Pain Relief at Aviv Clinics
In addition to non-medication techniques such as these, ongoing innovations like the comprehensive Aviv Medical Program can help manage chronic pain associated with conditions like fibromyalgia. Scientists believe that fibromyalgia and other chronic pain conditions may be caused by damage to the brain’s central pain sensitization region. Peer-reviewed, published studies indicate that the HBOT protocol used at Aviv Clinics may be able to restore function in these areas of the brain. The Aviv Medical Program combines this specialized HBOT protocol with therapies like physical training, nutritional counseling, and cognitive exercises to maximize positive outcomes.
To learn more about the treatment options available at Aviv Clinics:

Understanding Chronic Pain: Causes, Treatment Options and Non-Opioid Relief Strategies
Last Updated July 2, 2025
Chronic pain is one of the most common reasons why people seek medical care today. It’s also a leading cause of disability. Chronic pain can be debilitating when it’s severe enough. Many people who suffer from it experience a loss of mobility, leaving them unable to leave their homes or even their beds. While chronic pain this intense is rare, even less severe pain can leave you unable to enjoy activities you once loved, potentially leading to isolation and mental health problems like depression.
According to the CDC, nearly 1 in 5 adults in the United States suffers from chronic pain. The older population is hit especially hard because the risk of chronic pain increases with age. Adults aged 65 and older experience the most chronic pain of any demographic. Older adults are also more likely to experience high-impact chronic pain, or pain that affects a person’s daily life, work, socializing, and self-care.
Fortunately, there is hope. While the medical community is still learning about chronic pain, scientists are gaining more knowledge every day. Physicians are learning how to treat it effectively, so that those who suffer from it can live full lives.
What Is Pain? Understanding the Body’s Natural Response

In its most basic sense, pain is a sensation of discomfort created by the brain in response to unpleasant stimuli. If you stub your toe on a table leg, the nerve endings in your toe will send a signal to your brain, telling the brain that it’s been hurt. The brain then emits a signal back through your body, which you experience as pain.
This particular type of pain is known as acute pain.
Acute pain is a survival mechanism. If you never felt pain, then you would not know that your body was injured. For example, if you were to get a cut to the back of the thigh, you couldn’t visibly see your injury. Without pain signals from the brain, how would you know that your body had suffered an injury? You could die of an infection before you realized anything was wrong.
Acute pain is nature’s way of making us pay attention to our injuries. It alerts us to stop and take care of ourselves before we suffer further harm. Fortunately, acute pain like this usually disappears once the injury has healed. Chronic pain, on the other hand, is a different story.
What Is Chronic Pain and Why Doesn’t it Go Away?
Unlike acute pain, chronic pain persists after an injury or illness heals. By definition, chronic pain lasts for at least three months, but outbreaks can last for months or years, with no signs of disappearing. The sensation can vary from sharp and stabbing, like a migraine, to dull and throbbing, like an ache in your bones.
Everyone experiences chronic pain in different ways. There is no standard sensation or unifying characteristic.
This is why the classic 1-10 “pain scale” isn’t always an effective tool to gauge how much pain a person is suffering. Pain is a subjective experience, and we all have different pain threasholds. To complicate matters, chronic pain can come from multiple sources, as well.
Common Causes of Chronic Pain in Adults

-
Chronic Pain After Injury: When Acute Pain Becomes Long-Term
Chronic pain may be caused in response to acute pain, like a lingering ache in your back after rupturing or pulling a disc. Doctors and patients alike often mistake chronic pain for acute pain at first, because it may appear that chronic pain is simply the re-emergence of an old injury. But chronic pain is a pain that has taken on a life of its own.
Researchers are making progress towards understanding why acute pain sometimes shifts into chronic pain. In chronic back pain, for example, studies have identified risk factors like “…higher pain intensity, higher body weight, carrying heavy loads at work, difficult working positions, and depression.”
-
Chronic Pain From Illnesses Like Arthritis and Fibromyalgia
Just like with acute pain, chronic pain may be brought on by a condition like Lyme disease, fibromyalgia, sciatica, or arthritis. Older adults are more likely to suffer from chronic illnesses than younger adults. Common side effects of chronic illnesses include fatigue, aches, migraine, and nerve pain.
Certain types of cancer can also cause chronic pain. Tumors can put pressure on nerves, or release chemicals that irritate nerves. Cancer treatments, like chemotherapy or surgery, can also produce a chronic pain response.
-
The Link Between Chronic Pain, Depression and Anxiety
Chronic pain is also common in people who suffer from mental health conditions like depression and anxiety. It’s not currently clear whether depression itself causes chronic pain or if chronic pain causes depression. Given what we know about the mind-body connection, however, it’s likely that having one condition can worsen the other.
If you feel depressed, then you’re more likely to experience chronic pain more intensely. If your pain is so intense that you can no longer leave your home, then your depression can worsen from the isolation, creating a vicious cycle.
-
When Chronic Pain Has No Clear Cause
Sometimes, there’s no clear cause for chronic pain at all, which can be all the more frustrating for someone who suffers from it. It’s easy for someone with chronic pain to feel powerless in the world around them. However, that doesn’t have to be the case. There are plenty of different ways to manage chronic pain without addictive medications like opioids.
Non-Opioid Treatment Options for Chronic Pain Relief

In the past, it was common for doctors to prescribe opioids as a solution for patients with chronic pain. These medications can be effective against short-term acute pain, but using opioids alone is unlikely to give you the relief that you want. Even more concerning, however, is that opioids are extremely addictive. Using them for too long can create a dependence that can put users at risk for dangerous side effects and deadly overdoses.
Holistic Pain Management: A New Path to Relief
The most effective way to manage chronic pain is through a multi-pronged approach of proper nutrition, physical activity, and psychological aid.
Studies also indicate that hyperbaric oxygen therapy (HBOT) can benefit patients experiencing chronic pain from fibromyalgia and myofascial pain syndrome. In these studies, patients experienced improvements in pain threshold and quality of life, as well as decreased disability, after an HBOT treatment program. Patients of the Aviv Medical Program, which can include an evidence-based HBOT protocol among other therapies, have experienced relief of chronic pain from conditions like fibromyalgia. HBOT, when combined with nutritional guidance, physical activity, and cognitive coaching in the Aviv Medical Program, can be a life-changing treatment for chronic pain conditions.
Read more about how to manage chronic pain without medications.
Real Stories of Chronic Pain Relief: How Greg Found Hope with the Aviv Medical Program
When fibromyalgia pain affected Greg, he not only needed to quit his job, but struggled to even get out of bed on some days. Some treatments helped, but the side effects often left him with brain fog and other cognitive challenges. For more than 20 years, he sought a better solution. Since completing hyperbaric oxygen therapy and other interventions in the Aviv Medical Program, his pain is under control. Greg says he’s once again living his life naturally, instead of fighting his way through life with the chronic pain of fibromyalgia.
Contact us to determine if the Aviv Medical Program can be a suitable treatment for your chronic pain.
Meditation and Brain Health: How Scientific Evidence Supports Its Benefits
Last update: June 13, 2025
The COVID-19 virus has left us all under more stress than ever, but there’s one group of people that the pandemic has hit especially hard: older adults. A recent poll conducted by the National Poll on Healthy Aging interviewed 2,000 adults from the ages of 50 to 80. More than half (56%) of the participants reported struggling with feelings of isolation during the pandemic, a dramatic increase from 27% in the 2018 poll.
Long hours spent indoors away from family and friends can have us all feeling low, and stress and loneliness can wreak havoc on our mental health. That’s why many older adults are turning to the practice of mindfulness meditation to cope with stressful feelings during the pandemic.
Just like washing your hands to get rid of germs, meditation is an excellent way to help cleanse your mind of troublesome thoughts, and practicing mindfulness can do more than just help you relax. Taking a few minutes out of your day to ground yourself in the present moment is one of the most rewarding things you can do for your mental health, and the benefits are backed by science.
Supportive wellness practices, such as meditation, can be helpful to enhance cognitive and physical performance.

What is Meditation? Exploring Mindfulness Meditation and Brain Health
Mindfulness meditation is the art of being present in the here and now.
It’s about taking a few minutes every day to clear your mind of distressing thoughts and engaging with what’s right in front of you.
Think of it as a workout for your brain. In the same way that you might lift weights to keep your body strong, meditation is a way to train your mind and increase your focus and awareness. It’s not a spiritual practice or a mystical art; it’s a learned skill and anyone can learn to meditate, regardless of age.
5 Benefits of Meditation for Brain Health — Backed by Science
There are several proven benefits to meditating regularly. Numerous studies have shown that mindfulness practices like meditation and yoga can improve numerous mental health concerns. From easing anxiety and depression to stalling memory loss in Alzheimer’s patients, here are our top 5 benefits of meditation.
1. Slowing Cognitive Decline Through Meditation
Although many people dismiss lapses in memory recall as a side effect of growing older, there’s no scientific evidence to suggest memory loss is a natural side effect of aging. On the contrary, forgetting valuable memories doesn’t have to be the new normal for older adults.
Meditation has been proven to improve memory recall in adults in as little as eight weeks. Research also shows promising results in the use of mindfulness to slow the progression of cognitive conditions like Alzheimer’s disease and dementia. Patients who practiced mindfulness exercises reported reductions in cognitive decline and stress levels, and overall improvements to their quality of life.
Mindfulness isn’t only beneficial for those diagnosed with cognitive conditions, either. Studies have also shown that caregivers of those with cognitive impairments can benefit from the stress reduction offered through practicing meditation. In other words, everyone can benefit from a boost to the cognitive centers of the brain.
2. Enhancing Focus and Mental Clarity With Meditation
Practicing mindfulness can keep your brain active and in good shape, no matter how strong your memory is. You don’t have to be a seasoned expert. Even beginners can reap the benefits of mindfulness meditation.
In one study, participants who listened to a 10-minute meditation tape experienced increased attention span and focus when completing a test compared to those who didn’t meditate beforehand. One researcher further confirmed that people who meditate regularly consistently perform better on focus-related tasks. The same study also found that meditation calms the areas of the brain associated with mind-wandering and spontaneous thoughts, helping you stay focused on what you are doing in the present.
3. Meditation Supports Better Sleep and Combats Insomnia
Getting a good night’s rest is more important than ever for seniors and older adults. Sleep is the vital period when our minds cleanse themselves of harmful waste. Yet current research estimates 10-30% of people are affected by chronic insomnia, with older adults showing more susceptibility to sleep disturbances.
A randomized trial found that mindfulness meditation significantly improved sleep quality in middle-aged and older adults. Because meditation can lower stress levels, it helps clear your mind from troubling thoughts, which can make sleep come easier. If you have trouble sleeping at night, turn off your screens and try meditating for a few minutes before bed.
4. Reducing Anxiety Through Meditation
Although everyone worries from time to time, harboring too much stress in your body can be unhealthy. According to researchers, anywhere from 3-14% of all older adults meet the diagnostic criteria for generalized anxiety disorder. Unchecked anxiety and stress can worsen health conditions like fibromyalgia and lead to other mental health problems like depression.
If you want to take control of your anxious thoughts, meditation may be the solution. Studies have shown that mindfulness meditation can alleviate symptoms of generalized anxiety disorder and reduce stress levels, helping you clear your mind of fears and worries.
5. Uplifting Mood — Meditation’s Role in Mental Well-Being
Loneliness was already a common problem among older adults and retirees, but the COVID-19 pandemic has made it worse. Going out in public and visiting your family isn’t an option for many older adults, and the isolation can worsen feelings of loneliness and despair
Practicing mindfulness can help you manage these difficult emotions and improve your overall mood. Studies have shown that mindfulness training reduces feelings of loneliness and isolation, helping participants be happier in the present moment.
Mindfulness training has been shown to help reduce feelings of depression in adults. Those who practiced meditation therapy reported fewer symptoms of depression compared to their counterparts who didn’t meditate at all. Practicing mindfulness every day reminds you not to stress over every little thing, helping you stay calmer and more in control of your emotions.
How to Start Mindfulness and Meditation for Improved Brain Health
You don’t need any special equipment or training to get started. All you need is a comfortable place to sit and the willingness to give it a try. Here’s a quick guide to get you started:
- Find a quiet space where you can relax, free from distractions. If you’re inside, make sure that all televisions and electronic devices are turned off.
- Sit in a comfortable position and breathe gently.
- Pay attention to each inhale and exhale.
- Focus on all the sensations of your body as you breathe.
- Release any tensions you may be holding until you are completely relaxed.
- Continue to breathe in and out as you focus on your body’s inner sensations.
- If your mind wanders, that’s ok. Just re-focus on your breathing and start again.
- Keep going for 5-10 minutes or as long as you’d like to meditate.
Try to meditate at the same time every day to establish a routine. If you don’t want to sit in silence, you can find guided sessions via apps on your smart devices, or you can play some calming music to help you focus. For added benefits, try meditating outside on the porch or in a garden. Doing your daily session in nature can calm you even further, helping you make the most of your mindfulness practice.
The Bottom Line: Meditation Can Boost Brain Health and Well-Being
Mindfulness meditation is one of the most positive things you can do for your mental health and emotional well-being. It doesn’t take long to do, either. Having a simple routine to keep your mind in shape can offer benefits across all areas of your life. From improving memory recall to lowering stress levels and improving your sleep, practicing meditation can keep you more engaged in the present moment, helping you stay happy and calm during the best years of your life.
Cognitive health is one pillar of Aviv Clinics’ highly effective, science-backed medical program. The Aviv Medical Program is a customized, evidence-based intervention that can incorporate therapies like cognitive training and a specialized hyperbaric oxygen therapy protocol to achieve optimal results in both the brain and the body. Based on nearly two decades of research and development, the therapies in the Aviv Medical Program are customized to your specific needs and goals.
Curious if the Aviv Medical Program is the right choice for you? Contact Aviv Clinics today to schedule a complimentary consultation.

