
Cognitive Impairment and Long COVID: What You Should Know About Post-COVID Neurological Symptoms


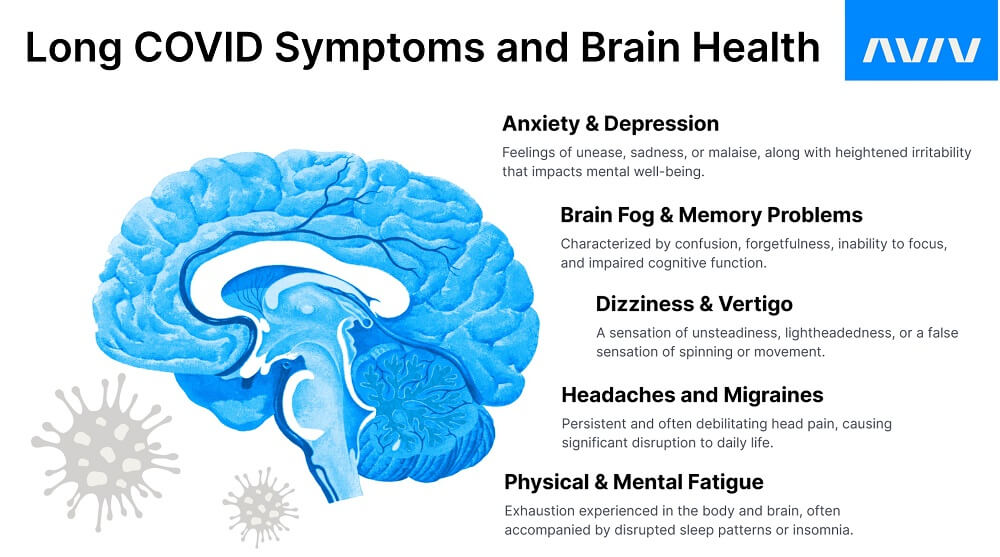
Even years after the pandemic began, there’s a lot that science still doesn’t know about COVID–19, especially when it comes to the long-term effects. Even after recovering from COVID, many people experience lingering neurological challenges. Emerging research suggests a troubling new link between the coronavirus long COVID neurological symptoms, including cognitive difficulties, persistent headaches, dizziness, and the now well-known “brain fog.” Research also suggests links between the virus and an increased risk for strokes, which is concerning for older adults or anyone already at an increased risk.
If your memory, focus, or mental clarity hasn’t returned to normal, you’re not alone. These neurological long COVID symptoms can persist for months or even years, affecting work, relationships, and quality of life. Understanding the link between long COVID and neurological symptoms is the first step in finding solutions and regaining your cognitive health.
In this article, we’ll explore what we currently know about long COVID neurological effects, how COVID-19 impacts the brain, and strategies to help you recover and thrive.
Neurological Effects of COVID-19: What Long COVID Patients Need to Know
Long COVID neurological symptoms are persistent cognitive and nervous system issues following a COVID-19 infection, including memory problems, headaches, and difficulty concentrating.
COVID-19 is best known for its respiratory symptoms, such as coughing and shortness of breath. However, the impact goes beyond the respiratory system. People who develop COVID-19 feel the effects in many other ways:
- Fatigue
- Fever
- Nausea
- Body aches
- Loss of smell or taste
- Cardiovascular issues
We can add the neurological effects of COVID to the list, which can be some of the most frustrating to experience. These can include:
- Headaches
- Dizziness
- Fatigue
- Brain fog
Many people continue to experience lingering symptoms of COVID-19, even months after recovering from the initial coronavirus infection. These people are often called “COVID long-haulers.”
Who Is a COVID Long-Hauler? Understanding Long COVID Neurological Symptoms
“COVID long-hauler” is a term used to describe the growing number of people who continue to experience symptoms of the Coronavirus long after the virus itself has left the body. Common complaints among long-haulers include a cough that won’t go away or persistent shortness of breath. Neurological problems are also common, including headaches, fatigue, and the now-infamous “COVID brain fog.”
While most people with COVID-19 recover within a few weeks, COVID long-haulers experience effects for much longer. People with long COVID are also at risk for developing other conditions, namely cardiovascular problems. In one study, nearly half of the participants “had impaired cardiac function at baseline.”
Long-haulers are a diverse group. Anyone can become one, young or old. It’s not unusual for someone to report feeling like they’re “in a fog” or “stuck in a daze” even weeks after testing negative for the virus. Some people may be plagued by COVID fatigue or headaches, while still others can’t taste their favorite foods.
You don’t need to have been hospitalized to be a COVID long-hauler, either. Even mild cases can lead to these unpleasant after-effects, which is why it’s possible you still don’t feel like your old self even after a minor bout with the virus. It’s unclear exactly why some people become COVID long-haulers while others experience no ill effects.
For some long-haulers, the impact of lingering symptoms greatly affects their quality of life. When long COVID patients were asked about their symptoms, researchers found that “fatigue scores were worse or comparable to those of individuals with cancer-related anemia or severe kidney disease” and that their health-related quality of life scores were lower than those of individuals with advanced metastatic cancers.”
Rest assured, researchers are working hard to gain a greater understanding of the risk factors involved.

How COVID-19 Impacts the Brain and Cognitive Function
Did you know that when it comes to COVID, losing your sense of smell is actually a neurological problem?
It’s true. The coronavirus can affect the olfactory nerve connecting your nose to your brain, which inhibits your sense of smell. This was one of the earliest pieces of evidence that COVID could affect the brain.
While we still need more research to determine the full extent of COVID’s neurological effects, preliminary studies have revealed a connection between the virus and “potential cognitive dysfunction.”
In the study, a group of COVID-19 patients between the ages of 30 and 60 underwent a series of neuropsychological tests to assess various functions of their brains, including memory function, processing speed, and executive function. The COVID-19 patients experienced inhibited cognitive function when compared to a healthy test group, and they especially struggled with sustaining attention on the tests, providing us with evidence that the “COVID brain fog” is a real phenomenon.
Further studies have also provided us with links between COVID-19 and a “higher prevalence of headache” occurrences and an increase in “strokes in patients with COVID-19,” giving us a greater understanding of how the virus can impact the brain.
Long-Term Neurological Effects of COVID-19 and Cognitive Impairment
Neurological effects of COVID-19 can last for months or even years, with symptom severity varying by age, overall health, and initial infection intensity. Long COVID neurological disease is linked to neuroinflammation, blood vessel injury, and immune system dysregulation triggered by the coronavirus.
The effects of COVID on the brain can sometimes last a very long time. It may show up in noticeable ways or in ways that are relatively undetectable in day-to-day life. You may have the feeling that your thoughts feel muddled and your mind is unclear. It may also be difficult to remember things, and you may struggle to stay on task.
Other symptoms are more easily recognized. In addition to headaches and migraines, many long COVID sufferers also experience sleep disturbances, dizziness, and vertigo. These symptoms are incredibly frustrating, especially if they don’t seem to go away.
How Long Do Neurological Symptoms Last After COVID?
Long COVID is surprisingly common—an estimated “65 million people worldwide” have been affected. More notably, researchers have found a “higher prevalence of Neuro-Long-COVID in female individuals.” And, it appears that the most “common, persistent, and disabling symptoms of long COVID are neurological.” This means struggles like frequent headaches and feelings of constant brain fog can linger long after other symptoms have improved.
It’s important to note that this condition affects everyone differently. There is no one-size-fits-all answer to many of the common questions about the neurological symptoms of long COVID, but research is getting closer to clearer answers.
Is Long COVID a Brain Disease? Understanding Neuroinflammation
The neurological effects of COVID can last for several months or longer after the initial infection. Many people experience symptoms for longer than six months, with one study revealing that, at a six-month follow-up, “only one-third reported complete resolution of symptoms.” It can be hard to predict, but some long COVID neurological symptoms “may persist for years.”
How long these symptoms last may depend on the severity of your initial infection, your age, and any pre-existing health conditions.
Is Long COVID Cognitive Impairment Permanent?
Evidence suggests that long-term cognitive impairment in COVID patients may not be permanent and can “spontaneously improve over time.” However, research on long COVID as a neurological disease is still evolving, and a number of questions will take time and further research to fully address.
Is Long COVID a Brain Disease?
Because of the way COVID-19 affects the body, some research suggests that long COVID may indeed be a disease of the brain. This is ultimately caused by neuroinflammation, an inflammatory response in the brain or the spinal cord. This inflammation is caused by activated “immune cells within the CNS” (central nervous system), which could account for many long COVID neurological symptoms and the increased risk of brain-related conditions such as stroke.
Understanding Long COVID and Neuroinflammation
Interestingly, COVID patients also exhibit high levels of inflammation in their blood. That’s not surprising since inflammation is one of the immune system’s natural responses to threats. In low levels, inflammation is a good thing; it’s a sign that your body is addressing the problem as intended. But as with everything in life, balance is key, and excessive inflammation can wreak havoc on your health.
One of the symptoms associated with Coronavirus is a “cytokine storm,” a “hyperactive immune response” that skyrockets inflammation levels. Cytokine storms have been associated with reduced oxygen in the blood and other respiratory problems caused by COVID-19. They’ve also been linked to neurological problems, such as brain fog, fatigue, or the stabbing headaches associated with the virus.
COVID-19 and Stroke Risk: What Long COVID Patients Should Know
While it’s still unclear exactly why COVID increases the risk of ischemic strokes (blood clots) in some people, inflammation could play a part. Medical research suggests that “increased systemic inflammation may itself increase stroke risk,” which could explain why the aging population is more susceptible.
Picture two highways. One highway is smooth and freshly paved without any potholes or blemishes. It’s easy for traffic to flow through this highway on a consistent basis, and traffic jams are uncommon. On the other hand, the second highway is littered with potholes, cracks, and closed lanes, all of which make it difficult for traffic to flow even on a good day. Now, which highway do you think will fare better when a snowstorm strikes?
The highways in this analogy are your blood vessels, and the flow of traffic is your blood cells. The snowstorm is, of course, COVID-19. High levels of inflammation in your body make it easier for the blood to clot, which can ultimately lead to strokes. This is also why those with pre-existing conditions are hit hard by the virus—their immune systems are already inflamed from fighting other problems.
Managing Inflammation to Protect Your Brain After COVID
Because COVID patients almost always exhibit higher levels of inflammation in their blood, having low inflammation levels in your body can help combat the severity of the virus. Eating a clean diet, exercising regularly, getting plenty of sleep, and avoiding stress keep inflammation levels low, which can help COVID long-haulers find relief. Avoiding stress is especially key, although that’s often easier said than done.
If you’re feeling stressed because of the pandemic and its impact on the world, you’re definitely not alone. If life changes, the news, or social media are stressing you out, try taking a break and unplugging for a while. While it’s important to stay informed, it’s also important to take care of your mental health.

When to Seek Medical Help for Long COVID Neurological Symptoms
If you’re struggling with long-term COVID neurological symptoms, you don’t need to suffer alone. Whether you’re being plagued by fatigue, brain fog, dizziness, headaches, or loss of taste or smell, any problem that affects your quality of life is worth bringing up to your doctor.
Although your doctor may not have all the answers yet, they’ll do everything they can to help you cope with your symptoms. There’s also the possibility that your symptoms may not be caused by COVID at all, but by another health condition instead. Never hesitate to seek help when you need it, especially when it comes to your cognitive well-being.
Coping Strategies for Long COVID Neurological Symptoms
When dealing with the neurological effects of COVID, it’s important to prioritize self-care and implement coping strategies that can help you navigate daily life. Care practices can help.
This can look like:
- Getting sufficient rest
- Maintaining a balanced diet
- Engaging in hobbies
- Practicing meditation and deep breathing
- Seeking counseling
It can also be helpful to complete activities at a pace that feels most comfortable. Breaking tasks into smaller, more manageable steps and using reminders can help improve focus and organization. Seeking support from professionals, such as those specializing in neurological conditions, can provide valuable guidance and treatment options tailored to your needs.

Treating Long COVID Neurological Symptoms With the Aviv Medical Program
Specialized treatments such as the Aviv Medical Program can help you on your journey toward managing and coping with long COVID neurological symptoms. The program uses a personalized approach and medical science backed by clinical trials to create a treatment catered to your unique symptoms and boost your brain and body performance. Your Aviv physician will prescribe a customized combination of therapies to treat your challenges. These interventions may include nutritional coaching, physical and cognitive training, and a unique, clinically-tested hyperbaric oxygen therapy (HBOT) protocol.
Hyperbaric oxygen therapy helps support the brain and body to regenerate healthy tissue. HBOT involves breathing high levels of pure oxygen inside a pressurized chamber. Clinical trials show the unique Aviv hyperbaric protocol can trigger the body’s healing mechanisms to help with recovery and overall wellness in the face of long COVID neurological symptoms.
Aviv Clinics’ unique HBOT protocol uses pressure fluctuations to increase these effects. In groundbreaking HBOT research, it was found that HBOT can improve “dysexecutive functions, psychiatric symptoms (depression, anxiety, and somatization), pain interference symptoms, and fatigue.”
When attorney and law firm COO Josh W. developed COVID pneumonia in 2021, it was only the beginning of his struggles. After months, he still suffered from excruciating nerve pain and other symptoms that left him unable to work for more than a few hours a day and distanced him from his family. Now, he’s back on his ‘A-Game’ at work and at home after completing the Aviv Medical Program.
WATCH: Recovering from Debilitating Long COVID Symptoms – Josh
The Aviv Medical Program begins with a medical assessment to get a clear picture of your symptoms and tailor a customized treatment program to best address your unique needs. Using the latest long COVID research, we take a personalized approach supported by cutting-edge technology.
WATCH: Latest Long COVID Research on Treatment Options for Long COVID Symptoms – Shai Efrati, M.D.
Key Takeaways: Long COVID Neurological Symptoms and Treatment Options
While we still need more research to determine the full extent of the coronavirus — especially when it comes to long-term symptoms — anyone of any age can minimize the damage caused by COVID.
Persistent cognitive challenges, headaches, or dizziness after COVID don’t need to be permanent. At Aviv Clinics, our physicians specialize in diagnosing and treating long COVID neurological symptoms with a personalized, science-backed approach. From comprehensive assessments to targeted therapies like hyperbaric oxygen for long COVID symptoms, we help people like you reclaim your mental clarity and overall well-being.
The Aviv Medical Program can be an effective treatment option for many conditions. For a consultation with one of our board-certified physicians, contact us to set up an appointment today.
Last Update: October 6, 2025
Aviv Medical Program provides you with a unique opportunity to invest in your health while you age



