Post-Stroke Brain Imaging: The Role of Radiology and Radiography in Functional Recovery

. When someone experiences a stroke, a timely series of steps in treatment, recovery, and risk management is essential. Many of us are aware of the fundamental rule of stroke care: “Time is tissue.” Immediate action is vital. Yet, that’s just the first stage on the stroke management timeline. A crucial element in stroke management is radiography, or post-stroke brain imaging. Radiologists use different types of imaging modalities to capture and assess damage to the brain caused by a stroke.
Stage 1: Stroke Diagnosis and Immediate Treatment
When initially diagnosing a stroke, radiographers and radiologists typically employ one or more of these advanced imaging tactics:
General CT Scan (computed tomography angiography): A CT scan (also called a CAT scan) provides a quick view of the brain to ensure there’s no active bleeding, as well as to rule out a brain mass that may be causing stroke-like symptoms.
MRI (magnetic resonance imaging): Sometimes an acute stroke will not show up on a CT scan, but it will be identifiable with an MRI.
MRA (magnetic resonance angiography) or CTA (computed tomography angiography): Once a diagnosis of an ischemic stroke has been made, the next step is to assess the “clot burden.” MRA or CTA can be used to determine if an obstruction is still present, how large it is, if it can be retrieved, or if the patient is eligible for a clot-dissolving medication called tPA.
Stage 2: Stroke Rehabilitation and Recovery

Once an acute stroke is treated and a patient enters the recovery and rehabilitation phases of stroke management, additional scans are available. These are used to assess the level of damage and reveal the strategies that may help address the damage. These include:
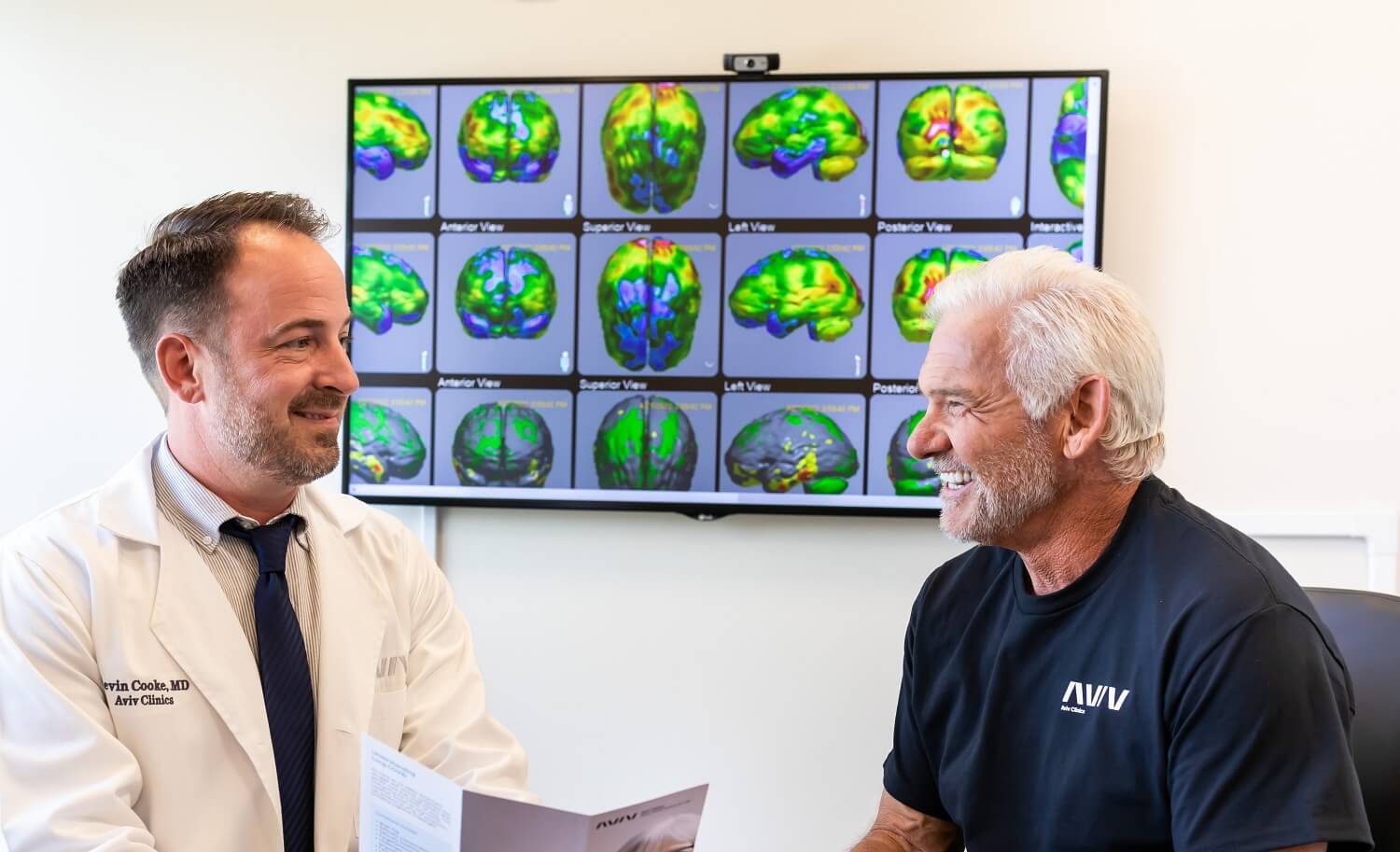
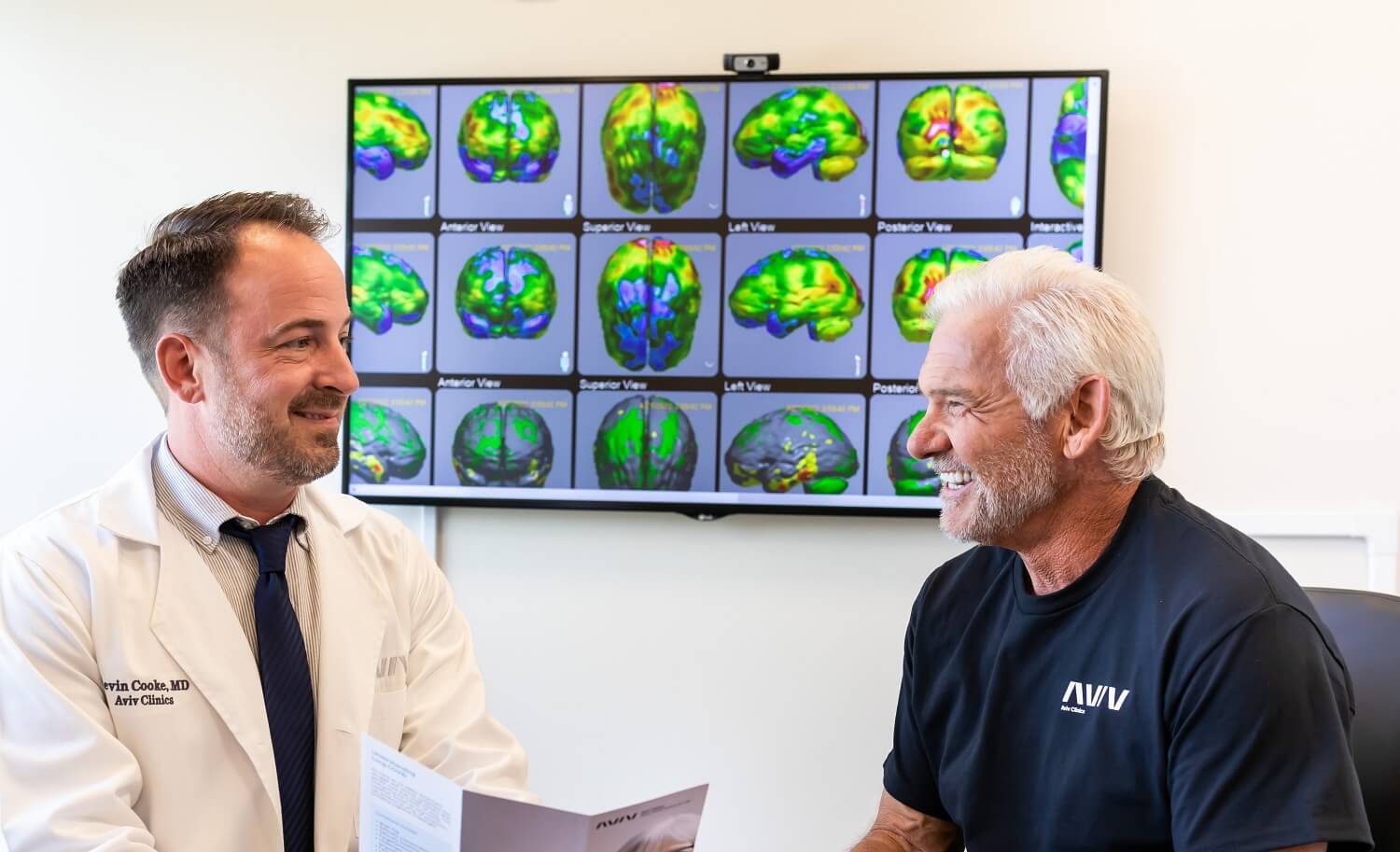
3T MRI: MRI technology is categorized by the strength of the magnet in the MRI machine, using a measurement known as a Tesla. Most standard MRIs are 1.5 Tesla. A 3 Tesla (3T) MRI is more advanced and provides a better view of the brain’s structure to detect evidence of stroke. It also allows clinicians to look at blood flow through the brain and assess nerve fiber tract connections. This advanced imaging is used at Aviv Clinics for the aforementioned reasons and to measure new brain cell growth.
SPECT Scan: This scan uses an intravenous contrast agent that provides insight into brain cell function and reduced blood flow. While the 3T MRI identifies the “real estate” of the brain that’s been taken up by the stroke, the SPECT can determine how much of that tissue is dead versus merely injured. It shows the “mismatch” between the brain’s structure, captured by MRI, and its function.
When used in combination, these two scans help guide a treatment plan that addresses a patient’s deficits. For example, the stroke may have impacted a person’s cognitive function in different areas of the brain (e.g., verbal memory, non-verbal memory, attention, processing speed). Stroke may also cause physical challenges such as weakness, paresis, or gait disruption. Whatever the patient’s unique circumstances are, a strategic plan — like the personalized Aviv Medical Program — works to stimulate those specific areas of the brain and optimize recovery.
Stage 3: Assessing Post-Stroke Progress

Upon completion of a treatment protocol, patients undergo follow-up scans to assess structural improvements. An MRI technique called diffusion tensor imaging (DTI) tractography can be used to measure:
- Strength of signals among nerve fiber tracts, connectivity, and direction of signals
- Density—how many brain cells were generated along the treatment timeline
Even during treatment, clinical improvements and changes may indicate that treatment is progressing positively. For instance, if a patient sees better mobility in an affected arm, there are likely improvements in the part of the brain that controls that limb. Those improvements can be confirmed later through advanced brain imaging.
Who Might Not Be a Candidate for MRI or SPECT?
Although advanced imaging is central to stroke diagnosis and rehabilitation, it is important to understand that some scans are not appropriate for all patients.
- MRI limitations: Anyone who has metal in their body may not be a candidate for MRI because of the magnetism involved. Furthermore who have kidney disease may not receive contrast with their MRI, but imaging should still provide adequate results.
- SPECT limitations: Because SPECT uses radiation, younger patients or those with specific concerns may need an alternate imaging method.
- Claustrophobia: Both of these types of scans require containment in a confined space and can trigger symptoms of claustrophobia. If closed conditions are a concern, patients are encouraged to have a conversation with their doctor before the scan.
Who Should Consider a Post-Stroke Imaging Assessment?
Not all stroke survivors fully recover with standard rehabilitation alone. Many hit a plateau and believe that further recovery is not possible. Advanced brain imaging can reveal hidden damage and help guide more targeted recovery strategies. You may benefit from a post-stroke imaging assessment if you are:
-
- A stroke survivor with lingering symptoms after therapy has ended
- Experiencing cognitive or physical deficits that remain undiagnosed or unresolved
- Seeking a data-driven, personalized plan for continued recovery
- Medically eligible for imaging procedures like MRI or SPECT
At Aviv Clinics, we use this detailed information, alongside other assessments, to identify areas of functional and physiological damage. This helps our physicians develop a client’s customized stroke treatment plan.
Your Personalized Roadmap to Stroke Recovery
Radiography offers an in-depth assessment of stroke and its resulting damage to the brain. But these images don’t just show damage; they also help define the path to recovery.
At Aviv Clinics, our board-certified medical team combines cutting-edge imaging methods with a personalized treatment program. Our physician-guided Aviv Medical Program is designed around our clients’ conditions, symptoms, needs, and goals. Physician-prescribed treatments may include an evidence-based hyperbaric oxygen therapy (HBOT) protocol and complementary therapies like cognitive exercises, physical therapy, physical training, and dietary support. Together, these elements support healing at the cellular level, helping stroke survivors regain quality of life.
If you or a loved one is recovering from a stroke, contact us to learn how Aviv Clinics can support your journey.
Last Update: July 17, 2025
Aviv Medical Program provides you with a unique opportunity to invest in your health while you age.



