
Your Inflammation Diet Plan: Harnessing the Power of Food to Fight Inflammation


Are you overwhelmed by brain fog, memory lapses, or difficulty concentrating? These cognitive challenges can significantly impact your daily life, and may be attributed to your diet because of chronic inflammation, a condition that affects the entire body — including the brain.
Researchers and scientists understand that certain aspects of our modern diet are leading to an epidemic of chronic diseases, from heart disease to cancer to Alzheimer’s disease. The way we eat is certainly a factor, but why and how, exactly?
Let’s explore the connection between inflammation, diet, and cognitive function. The fact of the matter is that you have full control over what goes into your body. With the right resources and support system, you can proactively make positive changes to put together an inflammation diet plan that can help you feel your absolute best.
The Origins of the Human Diet & Where We Are Now

Our hunter-gatherer ancestors ate a wide variety of whatever they could find, pick, or hunt, whenever it was available. Over thousands of years, our bodies have evolved to harness nutrients from many foods, and even endure periods of starvation.
As a result, our bodies have a fairly large buffer when it comes to nutritional stress. In other words, we’re biologically designed for dietary ups and downs.
However, our modern diets rely heavily on fried and processed foods and less on fruits, vegetables, nuts and beans. This literally tips the scale by pushing the body beyond its capacity to adapt and igniting the long, slow burn of chronic inflammation.
The good news is that chronic diseases are largely preventable, and changing your diet can reduce the chronic inflammation that causes many of them.
Before We talk About a Diet Plan, Let’s Talk Inflammation
Inflammation is not inherently harmful. It’s a natural process of the immune system that the body uses to protect you against foreign threats.
When the body detects something wrong, like a virus, injury, or infection, acute inflammation often occurs as part of the immune response. You’re probably familiar with this kind of inflammation, clearly visible in the form of redness, swelling, and pain.
In a healthy person, the response is robust enough to meet the threat: it puts the body under stress in order to repair itself and recover. When the threat is gone, the body quickly returns to baseline.
But sometimes the body’s immune system doesn’t operate as intended. It’s as if a minor alarm is going off all the time, subjecting the entire body to constant, low-level stress and inflammation.
That, in turn, leads to chronic disease.
The Centers for Disease Control (CDC) reports
6 in 10 adults in the US “live with at least one chronic disease.”
Comprehensive treatments, like the Aviv Medical Program, consider diet when leveraging other therapies (such as the world’s most advanced hyperbaric oxygen therapy (HBOT) program) for brain and physical performance.
Stress: The Silent Inflammation Threat
Stress is actually a normal situation for the body; at least on the cellular level. That even applies to oxidative stress, the kind created by free radicals and ultimately leading to chronic inflammation.
Our body naturally produces free radicals as a result of normal cellular metabolism, and these microscopic particles have important jobs in the cell. After they perform their functions, antioxidant molecules help neutralize these reactive free radicals.
It’s about balance; as long as the body has enough antioxidants to neutralize the potentially damaging free radicals, the system runs well. But if something tips the balance, free radicals can build up and cause oxidative stress, which begins a vicious cycle.
Oxidative stress, when out of control, wreaks havoc on your cells. The immune system recognizes the resulting cellular damage and kicks off an inflammatory response, similar to acute inflammation.
While they’re helping clean up the mess, however, immune cells like macrophages may “cause pathogenesis of chronic diseases.” In other words, they produce free radicals themselves, making the problem even worse.
Because this chronic immune response is comparatively weak compared to an acute response, it can easily go unnoticed, and thus untreated, for a long time.

The Link Between Diet, Inflammation, and Cognitive Health
Inflammation can have far-reaching consequences, impacting various aspects of health, including cognitive function.
- Research indicates that the same processes that create temporary cognitive decline when you get a cold can cause severe to permanent brain damage if inflammation sticks around for a while. For example, hepatitis C patients with a chronic infection that went unnoticed for a long time showed “increased rates of fatigue and depression, as well as evidence of metabolic brain dysfunction.”
- Systemic inflammation, the root of all known chronic health conditions, can lead to “profound structural and functional changes” in the brain. This can disrupt nutrient flow to the brain and age the brain.
This is why neuroinflammation has been linked to mood disorders, such as depression, anxiety, and PTSD, and neurodegenerative diseases, such as Alzheimer’s and Parkinson’s disease.
Chronic Inflammatory Foods to Avoid

Making mindful changes to your diet is key to helping to reduce inflammation and enhance your quality of life. By limiting your intake of the following processed foods (high in unhealthy fats and additives), you can help lower inflammation and improve your overall health:
- Red meat: Steak and hamburgers
- Processed meats: Bologna, bacon, sausage, and lunchmeat
- Baked goods: Commercial treats like snack cakes, pies, cookies, and brownies
- Refined grains: White bread and pasta are made from processed grains
- Fried foods: French fries, fried chicken, and donuts
- Added sugar: Candy, jelly, syrup, sugar-sweetened beverages, and other highly processed carbohydrates
- Trans fats: Found in margarine, microwave popcorn, refrigerated biscuits, and nondairy coffee creamers
The Best Diet and Foods for Chronic Inflammation
No matter where you are in your health journey, the time to make adjustments is now. And rest assured, these changes don’t have to be significant. Often, it’s a matter of introducing just a few new items into your meals or making simple substitutions.
Small steps equal big wins down the road..
Fuel Your Mind and Body with Anti-Inflammatory Power Foods
Each of us have unique needs and preferences when it comes to food. It’s important to honor these inclinations to set everyone up for success.
With that said, here is your anti-inflammatory food list for longevity. We encourage you to use this list to identify ways to incorporate healthy foods into your breakfast, lunch, and dinner.

For example, if you enjoy having ground beef tacos for dinner, trade the beef for salmon. If you enjoy sandwiches for lunch, swap the white bread for whole-grain bread.
- Vibrant fruits: Dark blue, purple, and red fruits like cherries, berries, plums, and pomegranates are packed with anthocyanins, powerful antioxidants that help reduce inflammation.
- Leafy greens: Spinach, kale, and other dark leafy greens are nutritional powerhouses, offering vitamins C and K to support your body’s inflammatory response.
- Whole grains: Oatmeal, quinoa, whole-wheat pasta, and whole-grain bread provide fiber and other essential nutrients that can help combat inflammation.
- Healthy fats: Nuts, seeds, olive oil, and avocado offer healthy fats that support overall health and can help reduce inflammation.
- Omega-3 fatty acids: Salmon and other fatty fish are rich in omega-3s, essential nutrients for reducing inflammation and supporting heart health.
- Legumes: Beans and lentils are excellent sources of fiber and protein, helping you stay full and regulate your digestive system.
- Coffee: Coffee can have a positive impact on brain health, as it contains polyphenols and antioxidants, which fight inflammation.
The MIND Diet
There are many anti-inflammatory diets out there, which can make your research journey pretty complex (not to mention burdensome). But if you want to focus on your cognitive health, check out the MIND diet.
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) combines two popular and scientifically proven diets (the Mediterranean and DASH diets, as the name implies). These nutritional plans were specifically developed to optimize anti-inflammatory effects on the brain.
Adapted from two plant-based diets that already have strong research behind them, it’s designed around foods with proven cognitive benefits. Research on the MIND diet itself showed that it works. For example, older adults who adhered to the diet experienced a 53% decrease in Alzheimer’s risk.
It’s important to remember that sticking to a particular diet 100% isn’t the goal, and it’s not necessary to get benefits. In the research mentioned above, the patients only had to follow the diet “moderately well” to see the decreased risk of Alzheimer’s.
The MIND diet has numerous advantages, including its simplicity.
It prescribes just 10 foods to eat, including:
- Dark leafy greens and other veggies
- Berries
- Nuts
- Olive oil
- Poultry
- Fish
It prescribes five foods to eat less of, including:
- Cheese
- Butter
- Fried food
- Red meat
- Sweets
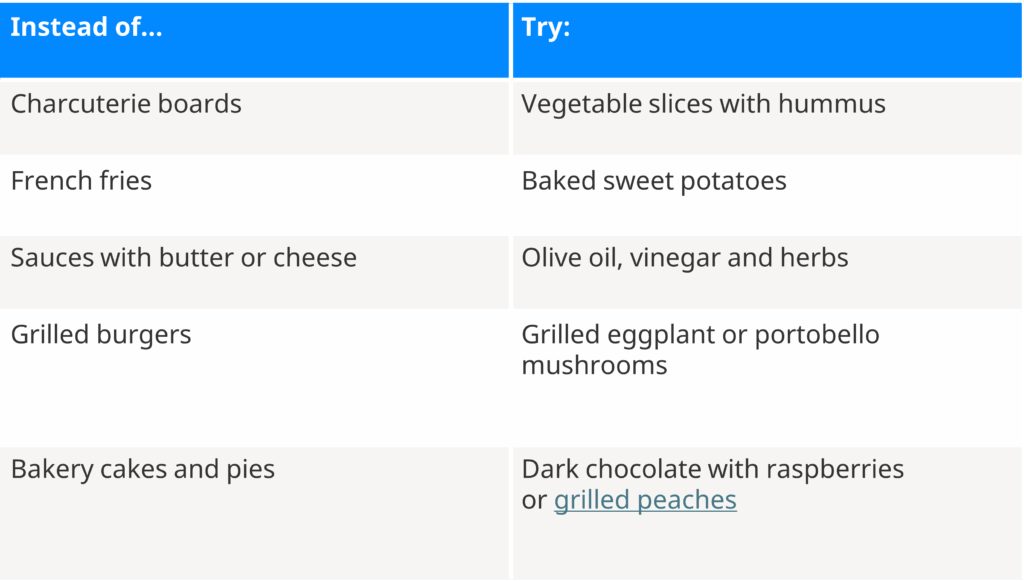
Making some minor substitutions to some of your favorite meals can help you jump-start your MIND diet journey. For example, Hopkins Medicine recommends:
Intermittent Fasting
Intermittent fasting is an eating style where you alternate between periods of eating and fasting. Rather than a diet, intermittent fasting is considered to be a lifestyle. So you’re in charge of your meal plan and fasting periods.
In addition to weight loss, intermittent fasting delivers anti-inflammatory properties via metabolic switching. The key is in ketones — acids your body produces when burning fat instead of glucose for energy.
Ketones have anti-inflammatory properties and can “directly relieve conditions of oxidative stress and inflammation.” The can help minimize the factors that drive conditions such as diabetes and heart disease.
Notes on Inflammation Supplements
So, can’t we just take antioxidant supplements to balance the free radicals?
Antioxidants became popular in the 1990s when research first began to reveal oxidative stress and inflammation were the culprits behind heart disease. Taking antioxidants seemed to be the perfect solution to counterbalance the free radicals produced by our modern diet.
In reality, a supplement pill cannot close the nutritional gaps our diets leave behind. From antioxidants to vitamin C, there are a few reasons why supplements aren’t the answer.
- Most people don’t need them. Supplements were primarily developed for people with conditions that prevent them from consuming or absorbing nutrients properly. In the United States, you’re more likely to be susceptible to over-nutrition or getting too much food for the body to handle. You don’t need 100% of the recommended daily allowance (RDA) of vitamins and nutrients every single day. The body has adapted to tolerate huge fluctuations in nutrients; some nutrients can be stored for a month or more in your body.
- They can’t improve on nature. When creating a supplement for, say, fish oil, manufacturers would want to be careful to provide purified fish oil with no contaminants, fillers, or unknown variables. It’s the best way to ensure that someone who wants to add fish oil to their diet is getting just that, nothing else. However, this is exactly the opposite of the way nature works. Most foods are combinations of hundreds of nutrients, and many work better together than separately.
- They just don’t work. More research is required to explain the exact reasons supplementation is inferior to food, but the studies show it nonetheless. One study notes that the “use of dietary supplements is not associated with mortality benefits.”
While many supplements are marketed as anti-inflammatory, it’s important to consult with a healthcare professional before adding them to your diet. Individual needs and health conditions can vary. So, it’s essential to discuss potential benefits or risks with a qualified medical expert.
Clearly, supplements aren’t a be-all and end-all solution. They can be used as part of a holistic approach to managing inflammation, which includes a healthy diet, regular exercise, and stress management. Getting the same nutrients from food, however, did lower risk factors for disease and mortality.
Combat Chronic Inflammation with Aviv Clinics

Remember, any change in the right direction can impact your health. If all you did was find a way to eat a single big handful of leafy green vegetables every day, you’d be consuming additional fiber, antioxidants, vitamins, and minerals, and working to slow down the inflammation process. So we encourage you to trust the process and stay consistent.
Nutrition coaching is one of the pillars of the Aviv Medical Program. Our nutritional coaching team includes licensed dietitians who offer personalized guidance to help optimize your diet and unlock your body’s full potential.
Keep in mind, a personalized nutrition plan is just one piece of the puzzle. Discover how Aviv Medical’s comprehensive approach reverses the aging process to rejuvenate your mind and body.
Aviv Medical Program provides you with a unique opportunity to invest in your health while you age.


