Ischemic vs. Hemorrhagic Stroke Symptoms: Types, Causes, and Recovery Options


A stroke can dramatically change a person’s life, affecting not only physical health but also emotional and cognitive well-being. Knowing the difference between ischemic vs. hemorrhagic stroke symptoms is crucial for seeking timely treatment and supporting recovery.
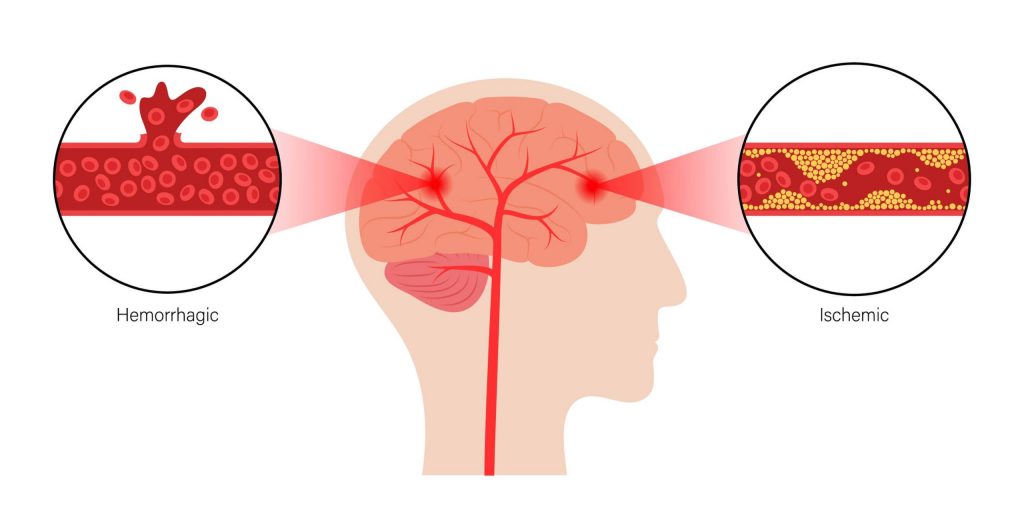
An ischemic stroke happens when a blockage interrupts the flow of oxygen-rich blood to the brain. A hemorrhagic stroke happens when a broken blood vessel causes bleeding to occur in the brain. In either situation, seek medical treatment immediately. Each type of stroke can present different warning signs, and early medical intervention can make a critical difference in outcomes.
In this guide, we’ll discuss the key differences, symptoms, and causes of ischemic vs. hemorrhagic strokes to help you better understand these conditions and make informed decisions if a stroke impacts you or someone you love.
Ischemic vs. Hemorrhagic Stroke Symptoms: Key Differences
The brain is a powerful yet delicate organ that enables the body to participate in countless activities. But when this organ experiences a stroke, it can manifest in several ways.
These manifestations can, unfortunately, make even routine activities we took for granted much more difficult. Both ischemic and hemorrhagic strokes minimize blood flow to the brain.
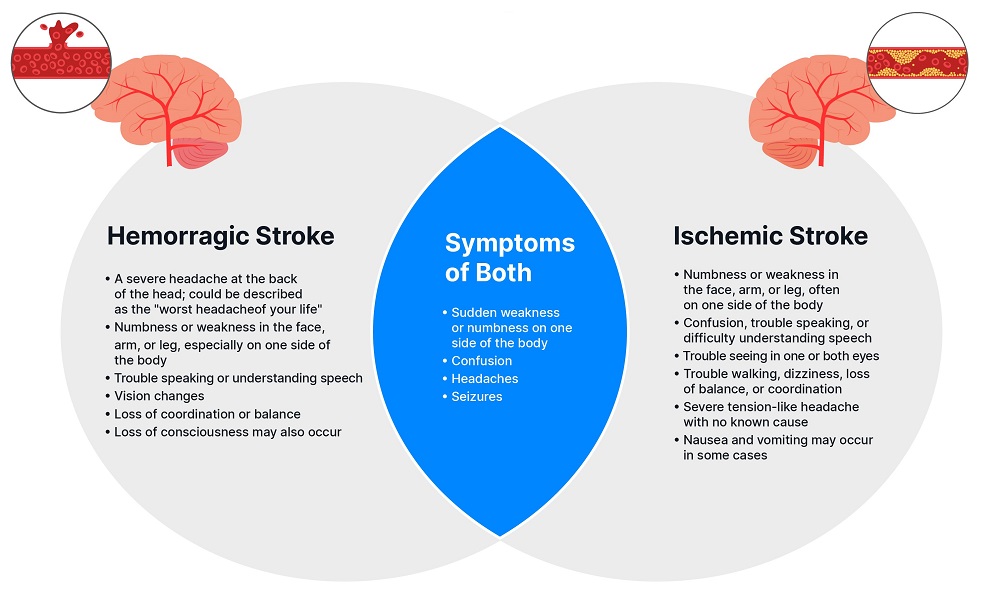
It’s important to know that frequency and symptom type can vary when comparing ischemic and hemorrhagic strokes. For example, seizures are more common in hemorrhagic stroke patients, while nausea and vomiting occur more often with ischemic strokes.
Both ischemic and hemorrhagic strokes may involve headaches, but those experiencing hemorrhagic strokes are more likely to have sudden, severe pain in the back of the head.
Ischemic vs. Hemorrhagic Stroke at a Glance:
- Ischemic Cause: Blood vessel blockage
- Hemorrhagic Cause: Blood vessel rupture
- Ischemic Stroke Common Symptoms: Numbness, vomiting, speech issues
- Hemorrhagic Stroke Common Symptoms: Severe headache, seizures, loss of consciousness
No matter what symptoms you or a loved one face, it’s critical to seek medical attention immediately if any of these signs are present.
What Is an Ischemic Stroke? Symptoms, Causes & Types
An ischemic stroke happens when a blood clot or other blockage interrupts the blood supply to the brain.
This blockage prevents brain tissue from getting the necessary oxygen and nutrients.
Ischemic strokes “account for about 87% of all strokes.” The two types of ischemic strokes are:
- Thrombotic stroke: Caused by a blood clot that builds in an artery that supplies blood to the brain
- Embolic stroke: Caused by a clot that forms in the body and travels through the blood vessels to the brain
- Cryptogenic stroke: Caused by unknown or undetermined factors despite medical investigation
The severity of ischemic stroke symptoms can differ depending on the location and impact of the stroke.
Common symptoms of Ischemic stroke often include a sudden onset of:
- Numbness or weakness in the face, arm, or leg, often on one side of the body
- Confusion, trouble speaking, or difficulty understanding speech
- Trouble seeing in one or both eyes
- Trouble walking, dizziness, loss of balance, or coordination
- Severe tension-like headache with no known cause
- Additional symptoms, such as nausea and vomiting, may occur in some cases
What Is a Hemorrhagic Stroke? Symptoms, Causes & Complications
Hemorrhagic strokes occur when a weakened blood vessel ruptures and bleeds into the brain.
This stroke category is further split into two sub-categories:
- Intracerebral hemorrhage: Bleeding into the brain tissue
- Subarachnoid hemorrhage: Bleeding in the space that surrounds the brain
Common symptoms of hemorrhagic stroke can include a sudden onset of:
- A severe headache at the back of the head; could be described as the “worst headache of your life”
- Numbness or weakness in the face, arm, or leg, especially on one side of the body
- Trouble speaking or understanding speech
- Vision changes
- Loss of coordination or balance
- Seizures and loss of consciousness may also occur.
The Key Differences Between Ischemic vs. Hemorrhagic Stroke Symptoms:
Again, we strongly urge you to seek medical attention if you or someone you know experiences any of the symptoms of an ischemic or hemorrhagic stroke.
Still experiencing post-stroke challenges? Contact us to learn how Aviv’s post-stroke program helps improve long-term function, even years after a stroke.
Thrombotic Stroke Symptoms and Causes
An intricate network of arteries supplies blood flow to the brain. When this flow is disrupted, it compromises the supply of vital oxygen to the brain, setting the stage for neurological repercussions.
Thrombotic strokes, a subset of ischemic strokes, occur when a blood clot forms in one of the arteries supplying blood to the brain. This restriction in blood flow can damage brain cells and result in severe neurological symptoms that can have a profound effect on the patient’s well-being.
Thrombotic Strokes and Atherosclerosis
Thrombotic strokes are often associated with a buildup of plaque in the blood vessels, a condition known as atherosclerosis. As plaque builds in the arteries, it increases the risk of blood clots.
Blood clots can affect large and small arteries, with varying outcomes depending on the location of the blockage:
- Large artery thrombotic strokes (atherosclerotic strokes)—which account for approximately 20% of all ischemic strokes—occur in “large blood vessels of the brain” and restrict blood flow more extensively, potentially leading to greater disability.
- Small penetrating artery thrombotic strokes (lacunar strokes) comprise around 25% of ischemic strokes and often result in milder symptoms.
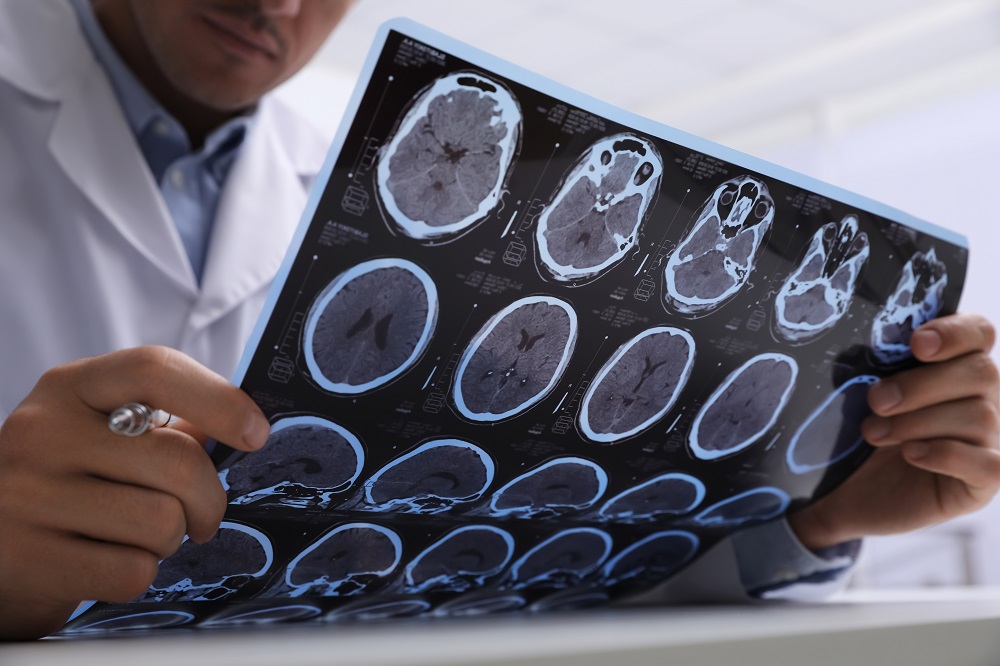
A CT scan can be used to show if there is bleeding in the affected area of the brain. The absence of bleeding on the scan suggests the stroke is ischemic or caused by a blood clot. By comparison, a hemorrhagic stroke will reveal bleeding in the CT scan.
Understanding the Causes of Atherosclerosis and Thrombotic Strokes
The primary cause of thrombotic stroke is atherosclerosis. Plaque deposits restrict blood flow in arteries near the brain, depriving it of essential oxygen and nutrients.
A number of risk factors can increase the risk of developing atherosclerosis, including:
- Smoking
- High cholesterol
- High blood pressure
- Lack of exercise
- Poor diet
- Genetics/family history
Addressing these risk factors can help reduce the likelihood of thrombotic stroke through proactive prevention of developing or worsening atherosclerosis.
Detecting Thrombotic Stroke Symptoms
The symptoms of a thrombotic stroke can strike suddenly. The urgency lies in immediate recognition of these symptoms, as timely intervention can be crucial to mitigate brain damage and support a healthy recovery.
Particular symptoms differ depending on the area of the brain affected but typically resemble symptoms of other stroke types:
- Sudden numbness or weakness on one side of the body
- Difficulty speaking or understanding speech
- Visual disturbances, such as blurred vision or changes in perception
- Cognitive impairments affecting memory, concentration, and mental clarity
- Difficulty walking or maintaining balance
A thrombotic stroke may also cause a severe headache, often described as a terrible migraine. This may be accompanied by excessive dizziness.
Prior to a stroke, it’s common to experience a transient ischemic attack (TIA), “a stroke that only lasts a few minutes.” This may also be called a “mini-stroke.” The symptoms are often indistinguishable from acute stroke and may only last an hour.
Seeking medical attention at the first sign of stroke-like symptoms gives doctors the most options in determining the best course of action.
Reducing the Risk of Thrombotic Stroke
By adopting proactive strategies to address the risk factors for blood clot formation, individuals can minimize the likelihood of thrombotic stroke by taking the following steps:
- Maintain a heart-healthy diet of fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Engage in at least 150 minutes of moderate-intensity exercise per week.
- Manage blood pressure through lifestyle modifications and regular monitoring.
- Reduce LDL cholesterol levels.
- Cease smoking and the use of tobacco products.
Routine consultations with healthcare providers can help you keep an eye on key health markers as well. Regular check-ups and screenings are crucial for early detection of potential risk factors.
Embolic Stroke: Causes, Risks and Recovery

A network of arteries orchestrates the delivery of blood to the brain. If plaque or blood clots form elsewhere in the body, break off, and travel toward the brain, it can result in blockages.
This mobile material (which mainly contains blood clots) is known as emboli; it travels through the bloodstream until reaching critical arteries, which can cause restricted blood flow to the brain.
This process, known as thromboembolism, can result in various complications. Most notably, it can cause an embolic stroke.
Causes and Prognosis of Embolic Strokes
Embolic strokes are “one of the most common causes of mortality” around the world. This is largely because risk factors for embolic stroke, such as cardiovascular disease, are prevalent on a global scale. The association with underlying conditions, many of which contribute to the formation of emboli, can increase the risk of embolic stroke.
Atrial fibrillation (AFib) is considered the most common cause, accounting for “15% of embolic strokes.” This condition can lead to the creation of emboli through thromboembolism. Here’s how:
- Irregular heart rhythms cause the upper chambers of the heart (atria) to fibrillate instead of contract.
- Irregular contractions lead to stagnant or slow-moving blood flow in the atria.
- Stagnant blood provides an environment conducive to the formation of blood clots.
- The blood clots break loose and travel through the bloodstream.
Other causes of embolic stroke include:
- Recent heart attack
- Artificial heart valves
- Dilated cardiomyopathy
- Muscular heart disease
- High cholesterol
- Hypertension
The prognosis of an embolic stroke can vary. Early intervention can improve the chances of recovery, depending on the size and location of the blocked artery, how quickly medical intervention occurs, and the overall health of the individual.
Common Embolic Stroke Symptoms
The common signs and symptoms of embolic stroke can vary and, like any stroke type, occur suddenly and without warning:
- Sudden numbness or weakness, often on one side of the body
- Problems with speech, including slurring or difficulty with comprehension
- Blurred vision or sudden changes in vision
- Cognitive challenges or confusion
- Intense and sudden headache
- Difficulty with walking and balance coordination
Sometimes, however, there are warning signs. The symptoms of a transient ischemic attack (TIA), or mini-stroke, can resemble the symptoms of a full stroke but may only last a few minutes. This brief episode sometimes occurs before a full stroke. If someone begins to experience these signs, it’s crucial to seek medical attention right away.
Addressing Risk Factors for Embolic Strokes
Because embolic strokes are caused by blood clots, proactive measures to minimize the risk of emboli are crucial for prevention. Actively engaging in risk-minimizing strategies can contribute to a reduced likelihood of embolic stroke and support a healthier lifestyle as a whole.
A few ways to mitigate risk include:
- Managing atrial fibrillation, especially in older populations
- Keeping blood pressure in a healthy range
- Maintaining healthy cholesterol levels
- Eating a heart-healthy diet
- Staying physically active
Essentially, focusing on cardiovascular health is a powerful way to be proactive by mitigating risk factors.
In some cases, healthcare providers may prescribe anticoagulant medications to reduce the risk of blood clots. It’s important to visit your doctor regularly to identify and address risk factors as early as possible.
Embolic Strokes vs Thrombotic Strokes: The Differences
Like thrombotic strokes, embolic strokes are classified as ischemic, caused by the blockage of an artery. The difference lies in where the blood clot or blockage is formed.
Understanding the difference between embolic and thrombotic stroke can help individuals adopt targeted preventive measures.
Origin
- Thrombotic strokes originate from blood clots formed in the blood vessels supplying the brain.
- Embolic strokes stem from emboli that form elsewhere in the body and travel through the bloodstream.
Location
- Blockages in thrombotic strokes occur in the same artery where the clot forms.
- Blockages in embolic strokes occur in the arteries in the brain.
Risk Factors
- Thrombotic strokes are linked to atherosclerosis.
- Embolic strokes are linked to cardiovascular conditions and atrial fibrillation.
These differences are instrumental in determining appropriate interventions, as embolic stroke treatment hinges on the origin of emboli.
Cryptogenic Strokes: What it Means When the Cause is Unknown
While it’s crucial to uncover the cause of a stroke, in some cases, the origin is not clear.
Strokes of obscure or unknown origin are known as cryptogenic strokes. It often takes an in-depth investigation to untangle a cryptogenic stroke. The cause of a cryptogenic stroke may even remain hidden or occur as a result of a temporary event or condition.
The lack of answers is frustrating and overwhelming. Shedding light on scientific facts and possible causes surrounding cryptogenic strokes can offer renewed optimism as you work with medical providers on seeking a post-stroke recovery program.
Understanding Cryptogenic Strokes: Facts to Consider
In most cases, a stroke occurs either when the blood supply to the brain is interrupted (ischemic stroke) or a blood vessel bleeds in the brain (hemorrhagic stroke). Consider the following statistics:
- “One in three” ischemic strokes are cryptogenic strokes.
- Nearly “half of cryptogenic strokes are embolic strokes”—a blood clot that forms and travels through the bloodstream to the brain.
- Cryptogenic strokes are more “frequent in younger than older patients.”
A medical provider may deem a stroke as cryptogenic upon a series of tests involving a brain CT scan, MRI, blood tests, and more.
Suspected Causes of Cryptogenic Strokes
While a large percentage of cryptogenic strokes never have a cause determined, there are possible causes that researchers suspect in many cryptogenic strokes:
- Atrial fibrillation (Afib): Afib is an irregular, often fast heartbeat in the heart’s upper chambers. This causes blood to pump inefficiently and clots to form. Symptoms include heart palpitations, fatigue, and shortness of breath. Shifts in the heart’s tissue and electrical system (usually via coronary artery disease or high blood pressure) cause Afib.
- Patent foramen ovale (PFO): PFO is when there is a hole in the heart between the left and right atria. Here’s how this happens: When a fetus is in the womb, it receives oxygenated blood through the umbilical cord. The heart directs this oxygen-rich blood to various parts of the body using a hole or flap between the right and left atriums. This hole is the PFO. When the baby is born, the PFO is supposed to close. But for about one in four people, it remains open. Some people experience zero issues from their PFO and go on to live full, healthy lives. However, problems can occur when clots develop and travel through the body. In individuals with PFO, a clot can enter the left side of the heart and can travel to the rest of the body, including the brain.
- Fabry’s disease: An inherited neurological disorder, Fabry’s disease occurs when a particular enzyme can’t sufficiently break down fatty materials that provide energy in the body. Fabry’s disease primarily affects men. Symptoms include burning pain in the arms and legs, clouded vision, and impaired blood circulation.
Recognizing Cryptogenic Stroke Symptoms
Symptoms of a cryptogenic stroke are the same as those of any type of stroke and can include:
- Sudden numbness or weakness of the face, arm, or leg
- Sudden trouble seeing and/or speaking
- Extreme headache without an obvious cause
- Sudden loss of balance or trouble walking
Minimizing Risk Factors for Cryptogenic Strokes
As “one in four stroke survivors” are at risk for another stroke, it’s essential to identify and minimize the risk factors for a cryptogenic stroke.
There are four main risk factors to help you get started. We encourage you to discuss these with your medical provider:
- High blood pressure: High blood pressure is one of the top risk factors for heart disease and stroke. If not managed, high blood pressure can strain your heart, arteries, and kidneys.
- High cholesterol: Contributing to fatty plaque, high cholesterol clogs arteries, which can lead to heart disease and stroke.
- Blood sugar: Our body breaks down food into glucose or blood sugar to use for energy. When blood sugar levels are too high, diabetes can develop. Diabetes impacts the kidneys, heart, eyes, and nerves.
- Genetic predisposition: A family history of stroke, clotting disorders, or diabetes may put you at greater risk of a stroke. Your doctor can order genetic testing if needed.
The key to combating these risk factors? Regular physical activity and healthy eating. Your doctor may recommend specific programs or regimens depending on where you are health-wise.
If you smoke, the best thing you can do for your health is to quit. Smokers have a high risk of developing heart complications.
Stroke Recovery Options: What to Do After an Ischemic or Hemorrhagic Stroke
Recovery after a stroke is a unique journey for each survivor, and timelines can vary greatly — it’s common and understandable to feel discouraged along the way. Stroke recovery is not always linear and can involve ups and downs. But if it’s been months or even years after the stroke incident and your progress still isn’t where you want to be, you can still have hope.
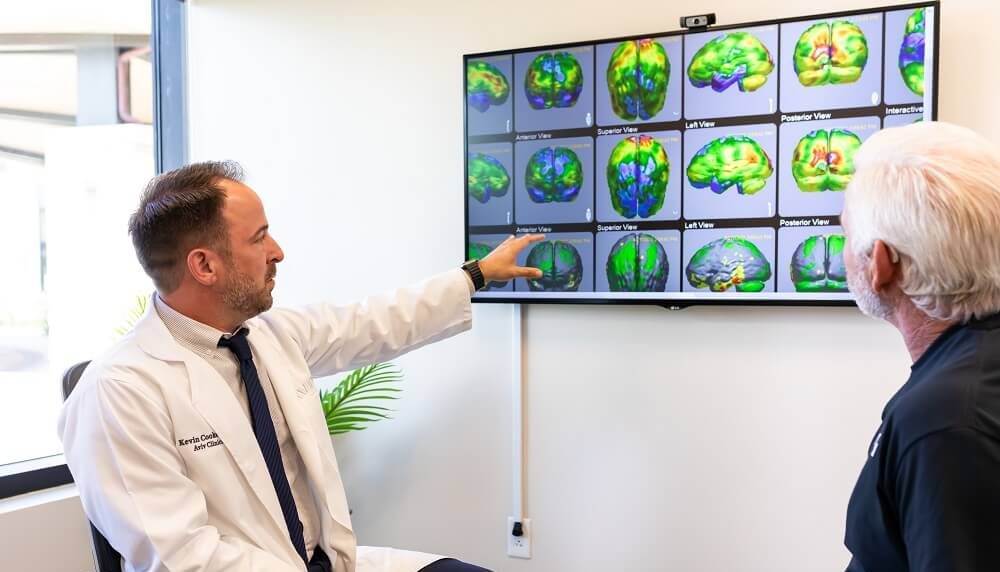
Backed by a diverse medical staff and nearly two decades of leading research, the Aviv Clinics team is here to help empower you. Our post-stroke program has revitalized individuals’ cognitive and physical capabilities, even years after a stroke.
Contact us today to learn if the Aviv Clinics stroke recovery program is right for you or your loved one.
Post Stroke Rehabilitation at Aviv Clinics
Bottom Line
No matter the cause of a stroke, the therapies used in the Aviv Medical Program are designed to optimize recovery outcomes and help you find a viable stroke treatment option. If you or a loved one has experienced an ischemic, hemorrhagic or cryptogenic stroke, recovery doesn’t end at the hospital.
Learn if the Aviv Clinics stroke recovery program is right for you or your loved one. Contact us to learn more about the Aviv Medical Program and how it may benefit your stroke recovery and management.
Last Update: September 30, 2025
Aviv Medical Program provides you with a unique opportunity to invest in your health while you age